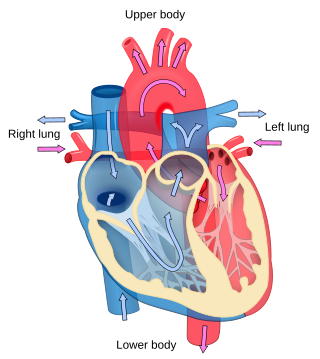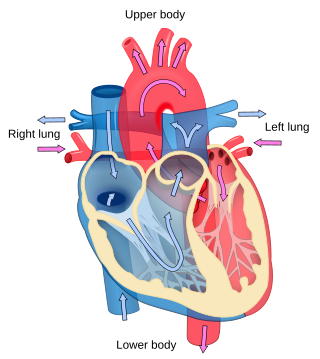
Cardiology is the study of the heart. Cardiology is a branch of medicine that deals with disorders of the heart and the cardiovascular system. The field includes medical diagnosis and treatment of congenital heart defects, coronary artery disease, heart failure, valvular heart disease, and electrophysiology. Physicians who specialize in this field of medicine are called cardiologists, a specialty of internal medicine. Pediatric cardiologists are pediatricians who specialize in cardiology. Physicians who specialize in cardiac surgery are called cardiothoracic surgeons or cardiac surgeons, a specialty of general surgery.

Angina, also known as angina pectoris, is chest pain or pressure, usually caused by insufficient blood flow to the heart muscle (myocardium). It is most commonly a symptom of coronary artery disease.

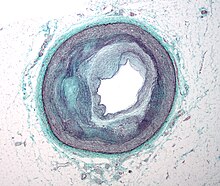
Atherosclerosis is a pattern of the disease arteriosclerosis, characterized by development of abnormalities called lesions in walls of arteries. These lesions may lead to narrowing of the arterial walls due to buildup of atheromatous plaques. At onset there are usually no symptoms, but if they develop, symptoms generally begin around middle age. In severe cases, it can result in coronary artery disease, stroke, peripheral artery disease, or kidney disorders, depending on which body part(s) the affected arteries are located in the body.

The Scandinavian Simvastatin Survival Study, was a multicentre, randomized, double-blind, placebo-controlled clinical trial, which provided the initial data that supported the use of the cholesterol-lowering drug, simvastatin, in people with a moderately raised cholesterol and coronary heart disease (CHD); that is people who had previously had a heart attack or angina. The study was sponsored by the pharmaceutical company Merck and enrolled 4,444 people from 94 centres in Scandinavia.

Interventional cardiology is a branch of cardiology that deals specifically with the catheter based treatment of structural heart diseases. Andreas Gruentzig is considered the father of interventional cardiology after the development of angioplasty by interventional radiologist Charles Dotter.

A cardiac stress test is a cardiological examination that evaluates the cardiovascular system's response to external stress within a controlled clinical setting. This stress response can be induced through physical exercise or intravenous pharmacological stimulation of heart rate.

Coronary thrombosis is defined as the formation of a blood clot inside a blood vessel of the heart. This blood clot may then restrict blood flow within the heart, leading to heart tissue damage, or a myocardial infarction, also known as a heart attack.

An atheroma, or atheromatous plaque, is an abnormal accumulation of material in the inner layer of an arterial wall.

Acute coronary syndrome (ACS) is a syndrome due to decreased blood flow in the coronary arteries such that part of the heart muscle is unable to function properly or dies. The most common symptom is centrally located pressure-like chest pain, often radiating to the left shoulder or angle of the jaw, and associated with nausea and sweating. Many people with acute coronary syndromes present with symptoms other than chest pain, particularly women, older people, and people with diabetes mellitus.

Variant angina, also known as Prinzmetal angina,vasospastic angina, angina inversa, coronary vessel spasm, or coronary artery vasospasm, is a syndrome typically consisting of angina. Variant angina differs from stable angina in that it commonly occurs in individuals who are at rest or even asleep, whereas stable angina is generally triggered by exertion or intense exercise. Variant angina is caused by vasospasm, a narrowing of the coronary arteries due to contraction of the heart's smooth muscle tissue in the vessel walls. In comparison, stable angina is caused by the permanent occlusion of these vessels by atherosclerosis, which is the buildup of fatty plaque and hardening of the arteries.

Unstable angina is a type of angina pectoris that is irregular or more easily provoked. It is classified as a type of acute coronary syndrome.

Percutaneous coronary intervention (PCI) is a minimally invasive non-surgical procedure used to treat narrowing of the coronary arteries of the heart found in coronary artery disease. The procedure is used to place and deploy coronary stents, a permanent wire-meshed tube, to open narrowed coronary arteries. PCI is considered 'non-surgical' as it uses a small hole in a peripheral artery (leg/arm) to gain access to the arterial system, an equivalent surgical procedure would involve the opening of the chest wall to gain access to the heart area. The term 'coronary angioplasty with stent' is synonymous with PCI. The procedure visualises the blood vessels via fluoroscopic imaging and contrast dyes. PCI is performed by an interventional cardiologists in a catheterization laboratory setting.
Coronary vasospasm refers to when a coronary artery suddenly undergoes either complete or sub-total temporary occlusion.

Myocardial perfusion imaging or scanning is a nuclear medicine procedure that illustrates the function of the heart muscle (myocardium).

Coronary ischemia, myocardial ischemia, or cardiac ischemia, is a medical term for abnormally reduced blood flow in the coronary circulation through the coronary arteries. Coronary ischemia is linked to heart disease, and heart attacks. Coronary arteries deliver oxygen-rich blood to the heart muscle. Reduced blood flow to the heart associated with coronary ischemia can result in inadequate oxygen supply to the heart muscle. When oxygen supply to the heart is unable to keep up with oxygen demand from the muscle, the result is the characteristic symptoms of coronary ischemia, the most common of which is chest pain. Chest pain due to coronary ischemia commonly radiates to the arm or neck. Certain individuals such as women, diabetics, and the elderly may present with more varied symptoms. If blood flow through the coronary arteries is stopped completely, cardiac muscle cells may die, known as a myocardial infarction, or heart attack.

A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops in one of the coronary arteries of the heart, causing infarction to the heart muscle. The most common symptom is retrosternal chest pain or discomfort that classically radiates to the left shoulder, arm, or jaw. The pain may occasionally feel like heartburn.
A diagnosis of myocardial infarction is created by integrating the history of the presenting illness and physical examination with electrocardiogram findings and cardiac markers. A coronary angiogram allows visualization of narrowings or obstructions on the heart vessels, and therapeutic measures can follow immediately. At autopsy, a pathologist can diagnose a myocardial infarction based on anatomopathological findings.

Ischemic cardiomyopathy is a type of cardiomyopathy caused by a narrowing of the coronary arteries which supply blood to the heart. Typically, patients with ischemic cardiomyopathy have a history of acute myocardial infarction, however, it may occur in patients with coronary artery disease, but without a past history of acute myocardial infarction. This cardiomyopathy is one of the leading causes of sudden cardiac death. The adjective ischemic means characteristic of, or accompanied by, ischemia — local anemia due to mechanical obstruction of the blood supply.
Remnant cholesterol, also known as remnant lipoprotein, is a very atherogenic lipoprotein composed primarily of very low-density lipoprotein (VLDL) and intermediate-density lipoprotein (IDL). Stated another way, remnant cholesterol is all plasma cholesterol that is not LDL cholesterol or HDL cholesterol, which are triglyceride-poor lipoproteins. However, remnant cholesterol is primarily chylomicron and VLDL, and each remnant particle contains about 40 times more cholesterol than LDL.

Arterial occlusion is a condition involving partial or complete blockage of blood flow through an artery. Arteries are blood vessels that carry oxygenated blood to body tissues. An occlusion of arteries disrupts oxygen and blood supply to tissues, leading to ischemia. Depending on the extent of ischemia, symptoms of arterial occlusion range from simple soreness and pain that can be relieved with rest, to a lack of sensation or paralysis that could require amputation.