Coronary circulation is the circulation of blood in the arteries and veins that supply the heart muscle (myocardium). Coronary arteries supply oxygenated blood to the heart muscle. Cardiac veins then drain away the blood after it has been deoxygenated. Because the rest of the body, and most especially the brain, needs a steady supply of oxygenated blood that is free of all but the slightest interruptions, the heart is required to function continuously. Therefore its circulation is of major importance not only to its own tissues but to the entire body and even the level of consciousness of the brain from moment to moment. Interruptions of coronary circulation quickly cause heart attacks, in which the heart muscle is damaged by oxygen starvation. Such interruptions are usually caused by coronary ischemia linked to coronary artery disease, and sometimes to embolism from other causes like obstruction in blood flow through vessels.

Ventricular fibrillation is an abnormal heart rhythm in which the ventricles of the heart quiver. It is due to disorganized electrical activity. Ventricular fibrillation results in cardiac arrest with loss of consciousness and no pulse. This is followed by sudden cardiac death in the absence of treatment. Ventricular fibrillation is initially found in about 10% of people with cardiac arrest.

Coronary artery bypass surgery, also known as coronary artery bypass graft, is a surgical procedure to treat coronary artery disease (CAD), the buildup of plaques in the arteries of the heart. It can relieve chest pain caused by CAD, slow the progression of CAD, and increase life expectancy. It aims to bypass narrowings in heart arteries by using arteries or veins harvested from other parts of the body, thus restoring adequate blood supply to the previously ischemic heart.
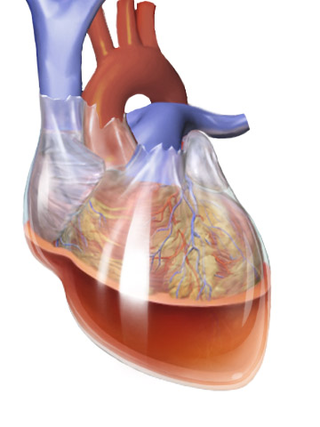
Cardiac tamponade, also known as pericardial tamponade, is a compression of the heart due to pericardial effusion. Onset may be rapid or gradual. Symptoms typically include those of obstructive shock including shortness of breath, weakness, lightheadedness, and cough. Other symptoms may relate to the underlying cause.
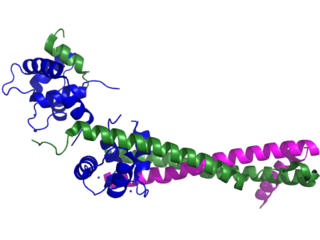
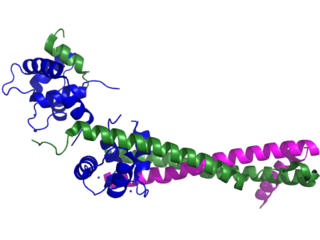
Troponin, or the troponin complex, is a complex of three regulatory proteins that are integral to muscle contraction in skeletal muscle and cardiac muscle, but not smooth muscle. Measurements of cardiac-specific troponins I and T are extensively used as diagnostic and prognostic indicators in the management of myocardial infarction and acute coronary syndrome. Blood troponin levels may be used as a diagnostic marker for stroke or other myocardial injury that is ongoing, although the sensitivity of this measurement is low.
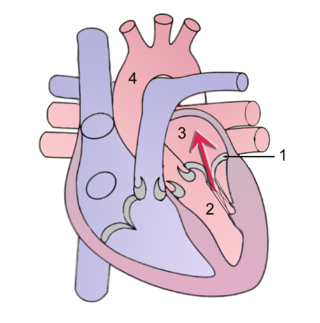
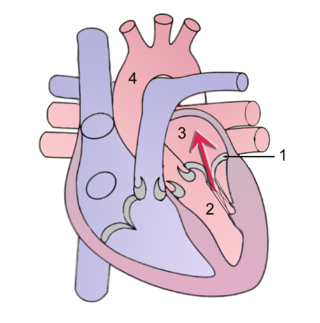
Mitral regurgitation(MR), also known as mitral insufficiency or mitral incompetence, is a form of valvular heart disease in which the mitral valve is insufficient and does not close properly when the heart pumps out blood. It is the abnormal leaking of blood backwards – regurgitation from the left ventricle, through the mitral valve, into the left atrium, when the left ventricle contracts. Mitral regurgitation is the most common form of valvular heart disease.
Dressler syndrome is a secondary form of pericarditis that occurs in the setting of injury to the heart or the pericardium. It consists of fever, pleuritic pain, pericarditis and/or pericardial effusion.
Pulsus paradoxus, also paradoxic pulse or paradoxical pulse, is an abnormally large decrease in stroke volume, systolic blood pressure and pulse wave amplitude during inspiration. Pulsus paradoxus is not related to pulse rate or heart rate, and it is not a paradoxical rise in systolic pressure. Normally, blood pressure drops less precipitously than 10 mmHg during inhalation. Pulsus paradoxus is a sign that is indicative of several conditions most commonly pericardial effusion.

A pericardial effusion is an abnormal accumulation of fluid in the pericardial cavity. The pericardium is a two-part membrane surrounding the heart: the outer fibrous connective membrane and an inner two-layered serous membrane. The two layers of the serous membrane enclose the pericardial cavity between them. This pericardial space contains a small amount of pericardial fluid, normally 15-50 mL in volume. The pericardium, specifically the pericardial fluid provides lubrication, maintains the anatomic position of the heart in the chest, and also serves as a barrier to protect the heart from infection and inflammation in adjacent tissues and organs.

Acute pericarditis is a type of pericarditis usually lasting less than 6 weeks. It is the most common condition affecting the pericardium.

Takotsubo cardiomyopathy or takotsubo syndrome (TTS), also known as stress cardiomyopathy, is a type of non-ischemic cardiomyopathy in which there is a sudden temporary weakening of the muscular portion of the heart. It usually appears after a significant stressor, either physical or emotional; when caused by the latter, the condition is sometimes called broken heart syndrome. Examples of physical stressors that can cause TTS are sepsis, shock, subarachnoid hemorrhage, and pheochromocytoma. Emotional stressors include bereavement, divorce, or the loss of a job. Reviews suggest that of patients diagnosed with the condition, about 70–80% recently experienced a major stressor, including 41–50% with a physical stressor and 26–30% with an emotional stressor. TTS can also appear in patients who have not experienced major stressors.

Accelerated idioventricular rhythm is a ventricular rhythm with a rate of between 40 and 120 beats per minute. Idioventricular means “relating to or affecting the cardiac ventricle alone” and refers to any ectopic ventricular arrhythmia. Accelerated idioventricular arrhythmias are distinguished from ventricular rhythms with rates less than 40 and those faster than 120. Though some other references limit to between 60 and 100 beats per minute. It is also referred to as AIVR and "slow ventricular tachycardia."
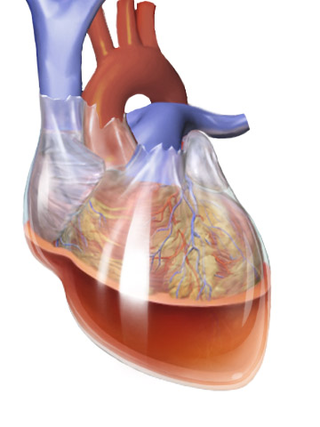
Hemopericardium refers to blood in the pericardial sac of the heart. It is clinically similar to a pericardial effusion, and, depending on the volume and rapidity with which it develops, may cause cardiac tamponade.

A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops in one of the coronary arteries of the heart, causing infarction to the heart muscle. The most common symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck or jaw. Often it occurs in the center or left side of the chest and lasts for more than a few minutes. The discomfort may occasionally feel like heartburn. Other symptoms may include shortness of breath, nausea, feeling faint, a cold sweat, feeling tired, and decreased level of consciousness. About 30% of people have atypical symptoms. Women more often present without chest pain and instead have neck pain, arm pain or feel tired. Among those over 75 years old, about 5% have had an MI with little or no history of symptoms. An MI may cause heart failure, an irregular heartbeat, cardiogenic shock or cardiac arrest.

Primary ventricular fibrillation (PVF) is an unpredictable and potentially fatal arrhythmia occurring during the acute phase of a myocardial infarction leading to immediate collapse and, if left untreated, leads to sudden cardiac death within minutes. In developed countries, PVF is a leading cause of death. Worldwide, the annual number of deaths caused by PVF is comparable to the number of deaths caused by road traffic accidents. A substantial portion of these deaths could be avoided by seeking immediate medical attention when symptoms are noticed.

Reperfusion therapy is a medical treatment to restore blood flow, either through or around, blocked arteries, typically after a heart attack. Reperfusion therapy includes drugs and surgery. The drugs are thrombolytics and fibrinolytics used in a process called thrombolysis. Surgeries performed may be minimally-invasive endovascular procedures such as a percutaneous coronary intervention (PCI), which involves coronary angioplasty. The angioplasty uses the insertion of a balloon and/or stents to open up the artery. Other surgeries performed are the more invasive bypass surgeries that graft arteries around blockages.
Myocardial infarction complications may occur immediately following a heart attack, or may need time to develop. After an infarction, an obvious complication is a second infarction, which may occur in the domain of another atherosclerotic coronary artery, or in the same zone if there are any live cells left in the infarct.
A diagnosis of myocardial infarction is created by integrating the history of the presenting illness and physical examination with electrocardiogram findings and cardiac markers. A coronary angiogram allows visualization of narrowings or obstructions on the heart vessels, and therapeutic measures can follow immediately. At autopsy, a pathologist can diagnose a myocardial infarction based on anatomopathological findings.

Management of acute coronary syndrome is targeted against the effects of reduced blood flow to the affected area of the heart muscle, usually because of a blood clot in one of the coronary arteries, the vessels that supply oxygenated blood to the myocardium. This is achieved with urgent hospitalization and medical therapy, including drugs that relieve chest pain and reduce the size of the infarct, and drugs that inhibit clot formation; for a subset of patients invasive measures are also employed. Basic principles of management are the same for all types of acute coronary syndrome. However, some important aspects of treatment depend on the presence or absence of elevation of the ST segment on the electrocardiogram, which classifies cases upon presentation to either ST segment elevation myocardial infarction (STEMI) or non-ST elevation acute coronary syndrome (NST-ACS); the latter includes unstable angina and non-ST elevation myocardial infarction (NSTEMI). Treatment is generally more aggressive for STEMI patients, and reperfusion therapy is more often reserved for them. Long-term therapy is necessary for prevention of recurrent events and complications.

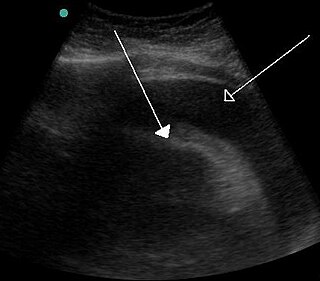
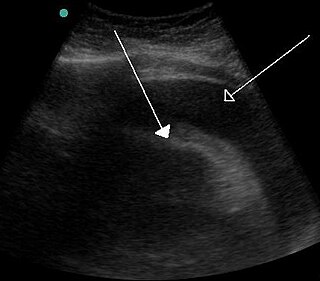
Left ventricular thrombus is a blood clot (thrombus) in the left ventricle of the heart. LVT is a common complication of acute myocardial infarction (AMI). Typically the clot is a mural thrombus, meaning it is on the wall of the ventricle. The primary risk of LVT is the occurrence of cardiac embolism, in which the thrombus detaches from the ventricular wall and travels through the circulation and blocks blood vessels. Blockage can be especially damaging in the heart or brain (stroke).