Bradycardia is a medical term used to describe a resting heart rate under 60 beats per minute (BPM). While bradycardia can result from a variety of pathologic processes, it is commonly a physiologic response to cardiovascular conditioning, or due to asymptomatic type 1 atrioventricular block. Resting heart rates less than 50 BPM are often normal during sleep in young and healthy adults, and in athletes. In large population studies of adults without underlying heart disease, resting heart rates of 45-50 BPM appear to be the lower limits of normal, dependent on age and sex. Bradycardia is most likely to be discovered in the elderly, as both age and underlying cardiac disease progression contribute to its development.

Tachycardia, also called tachyarrhythmia, is a heart rate that exceeds the normal resting rate. In general, a resting heart rate over 100 beats per minute is accepted as tachycardia in adults. Heart rates above the resting rate may be normal or abnormal.

Wolff–Parkinson–White syndrome (WPWS) is a disorder due to a specific type of problem with the electrical system of the heart involving an accessory pathway able to conduct electrical current between the atria and the ventricles, thus bypassing the atrioventricular node. About 60% of people with the electrical problem developed symptoms, which may include an abnormally fast heartbeat, palpitations, shortness of breath, lightheadedness, or syncope. Rarely, cardiac arrest may occur. The most common type of irregular heartbeat that occurs is known as paroxysmal supraventricular tachycardia.

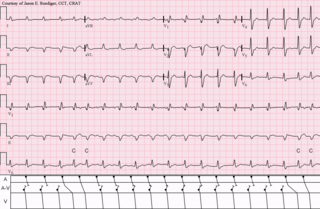
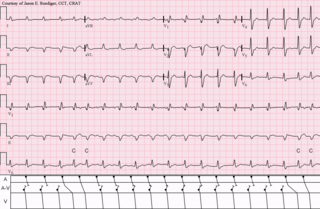
Atrial flutter (AFL) is a common abnormal heart rhythm that starts in the atrial chambers of the heart. When it first occurs, it is usually associated with a fast heart rate and is classified as a type of supraventricular tachycardia. Atrial flutter is characterized by a sudden-onset (usually) regular abnormal heart rhythm on an electrocardiogram (ECG) in which the heart rate is fast. Symptoms may include a feeling of the heart beating too fast, too hard, or skipping beats, chest discomfort, difficulty breathing, a feeling as if one's stomach has dropped, a feeling of being light-headed, or loss of consciousness.

The cardiac conduction system transmits the signals generated by the sinoatrial node – the heart's pacemaker, to cause the heart muscle to contract, and pump blood through the body's circulatory system. The pacemaking signal travels through the right atrium to the atrioventricular node, along the bundle of His, and through the bundle branches to Purkinje fibers in the walls of the ventricles. The Purkinje fibers transmit the signals more rapidly to stimulate contraction of the ventricles.
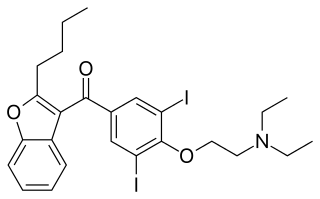
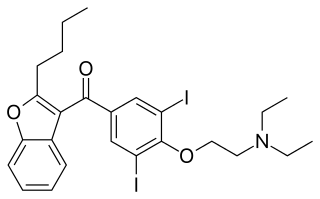
Amiodarone is an antiarrhythmic medication used to treat and prevent a number of types of cardiac dysrhythmias. This includes ventricular tachycardia (VT), ventricular fibrillation (VF), and wide complex tachycardia, as well as atrial fibrillation and paroxysmal supraventricular tachycardia. Evidence in cardiac arrest, however, is poor. It can be given by mouth, intravenously, or intraosseously. When used by mouth, it can take a few weeks for effects to begin.

Ventricular tachycardia is a cardiovascular disorder in which fast heart rate occurs in the ventricles of the heart. Although a few seconds of VT may not result in permanent problems, longer periods are dangerous; and multiple episodes over a short period of time are referred to as an electrical storm. Short periods may occur without symptoms, or present with lightheadedness, palpitations, or chest pain. Ventricular tachycardia may result in ventricular fibrillation (VF) and turn into cardiac arrest. This conversion of the VT into VF is called the degeneration of the VT. It is found initially in about 7% of people in cardiac arrest.

Supraventricular tachycardia (SVT) is an umbrella term for fast heart rhythms arising from the upper part of the heart. This is in contrast to the other group of fast heart rhythms – ventricular tachycardia, which start within the lower chambers of the heart. There are four main types of SVT: atrial fibrillation, atrial flutter, paroxysmal supraventricular tachycardia (PSVT), and Wolff–Parkinson–White syndrome. The symptoms of SVT include palpitations, feeling of faintness, sweating, shortness of breath, and/or chest pain.

AV-nodal reentrant tachycardia (AVNRT) is a type of abnormal fast heart rhythm. It is a type of supraventricular tachycardia (SVT), meaning that it originates from a location within the heart above the bundle of His. AV nodal reentrant tachycardia is the most common regular supraventricular tachycardia. It is more common in women than men. The main symptom is palpitations. Treatment may be with specific physical maneuvers, medications, or, rarely, synchronized cardioversion. Frequent attacks may require radiofrequency ablation, in which the abnormally conducting tissue in the heart is destroyed.
Premature atrial contraction (PAC), also known as atrial premature complexes (APC) or atrial premature beats (APB), are a common cardiac dysrhythmia characterized by premature heartbeats originating in the atria. While the sinoatrial node typically regulates the heartbeat during normal sinus rhythm, PACs occur when another region of the atria depolarizes before the sinoatrial node and thus triggers a premature heartbeat, in contrast to escape beats, in which the normal sinoatrial node fails, leaving a non-nodal pacemaker to initiate a late beat.

Paroxysmal supraventricular tachycardia (PSVT) is a type of supraventricular tachycardia, named for its intermittent episodes of abrupt onset and termination. Often people have no symptoms. Otherwise symptoms may include palpitations, feeling lightheaded, sweating, shortness of breath, and chest pain.

In cardiology, a ventricular escape beat is a self-generated electrical discharge initiated by, and causing contraction of the ventricles of the heart; normally the heart rhythm is begun in the atria of the heart and is subsequently transmitted to the ventricles. The ventricular escape beat follows a long pause in ventricular rhythm and acts to prevent cardiac arrest. It indicates a failure of the electrical conduction system of the heart to stimulate the ventricles.

Wandering atrial pacemaker (WAP) is an atrial rhythm where the pacemaking activity of the heart originates from different locations within the atria. This is different from normal pacemaking activity, where the sinoatrial node is responsible for each heartbeat and keeps a steady rate and rhythm. Causes of wandering atrial pacemaker are unclear, but there may be factors leading to its development. It is often seen in the young, the old, and in athletes, and rarely causes symptoms or requires treatment. Diagnosis of wandering atrial pacemaker is made by an ECG.
An accessory pathway is an additional electrical connection between two parts of the heart. These pathways can lead to abnormal heart rhythms or arrhythmias associated with symptoms of palpitations. Some pathways may activate a region of ventricular muscle earlier than would normally occur, referred to as pre-excitation, and this may be seen on an electrocardiogram. The combination of an accessory pathway that causes pre-excitation with arrhythmias is known as Wolff-Parkinson-White syndrome.

Junctional tachycardia is a form of supraventricular tachycardia characterized by involvement of the AV node. It can be contrasted to atrial tachycardia. It is a tachycardia associated with the generation of impulses in a focus in the region of the atrioventricular node due to an A-V disassociation. In general, the AV junction's intrinsic rate is 40-60 bpm so an accelerated junctional rhythm is from 60-100bpm and then becomes junctional tachycardia at a rate of >100 bpm.

An ectopic pacemaker, also known as ectopic focus or ectopic foci, is an excitable group of cells that causes a premature heart beat outside the normally functioning SA node of the heart. It is thus a cardiac pacemaker that is ectopic, producing an ectopic beat. Acute occurrence is usually non-life-threatening, but chronic occurrence can progress into tachycardia, bradycardia or ventricular fibrillation. In a normal heart beat rhythm, the SA node usually suppresses the ectopic pacemaker activity due to the higher impulse rate of the SA node. However, in the instance of either a malfunctioning SA node or an ectopic focus bearing an intrinsic rate superior to SA node rate, ectopic pacemaker activity may take over the natural heart rhythm. This phenomenon is called an escape rhythm, the lower rhythm having escaped from the dominance of the upper rhythm. As a rule, premature ectopic beats indicate increased myocyte or conducting tissue excitability, whereas late ectopic beats indicate proximal pacemaker or conduction failure with an escape 'ectopic' beat.
Atrial tachycardia is a type of heart rhythm problem in which the heart's electrical impulse comes from an ectopic pacemaker in the upper chambers (atria) of the heart, rather than from the sinoatrial node, the normal origin of the heart's electrical activity. As with any other form of tachycardia, the underlying mechanism can be either the rapid discharge of an abnormal focus, the presence of a ring of cardiac tissue that gives rise to a circle movement (reentry), or a triggered rapid rhythm due to other pathological circumstances.

Arrhythmias, also known as cardiac arrhythmias, heart arrhythmias, or dysrhythmias, are irregularities in the heartbeat, including when it is too fast or too slow. A resting heart rate that is too fast – above 100 beats per minute in adults – is called tachycardia, and a resting heart rate that is too slow – below 60 beats per minute – is called bradycardia. Some types of arrhythmias have no symptoms. Symptoms, when present, may include palpitations or feeling a pause between heartbeats. In more serious cases, there may be lightheadedness, passing out, shortness of breath, chest pain, or decreased level of consciousness. While most cases of arrhythmia are not serious, some predispose a person to complications such as stroke or heart failure. Others may result in sudden death.
An automatic tachycardia is a cardiac arrhythmia which involves an area of the heart generating an abnormally fast rhythm, sometimes also called enhanced automaticity. These tachycardias, or fast heart rhythms, differ from reentrant tachycardias in which there is an abnormal electrical pathway which gives rise to the pathology. Most automatic tachycardias are supraventricular tachycardias (SVT). It is important to recognize an automatic tachycardia because the treatment will be different to that for a reentrant tachycardia. The most useful clue will be the presence of 'warm up' and 'cool down'. This means that whereas a reentrant tachycardia will both begin and end abruptly as cardiac conduction uses then ceases to use the accessory pathway, an automatic tachycardia will rise and fall gradually in rate as the automatic focus increases and decreases its automatic rate of electrical discharge.