Angina, also known as angina pectoris, is chest pain or pressure, usually caused by insufficient blood flow to the heart muscle (myocardium). It is most commonly a symptom of coronary artery disease.

Coronary circulation is the circulation of blood in the arteries and veins that supply the heart muscle (myocardium). Coronary arteries supply oxygenated blood to the heart muscle. Cardiac veins then drain away the blood after it has been deoxygenated. Because the rest of the body, and most especially the brain, needs a steady supply of oxygenated blood that is free of all but the slightest interruptions, the heart is required to function continuously. Therefore its circulation is of major importance not only to its own tissues but to the entire body and even the level of consciousness of the brain from moment to moment. Interruptions of coronary circulation quickly cause heart attacks, in which the heart muscle is damaged by oxygen starvation. Such interruptions are usually caused by coronary ischemia linked to coronary artery disease, and sometimes to embolism from other causes like obstruction in blood flow through vessels.

Ischemia or ischaemia is a restriction in blood supply to any tissue, muscle group, or organ of the body, causing a shortage of oxygen that is needed for cellular metabolism. Ischemia is generally caused by problems with blood vessels, with resultant damage to or dysfunction of tissue i.e. hypoxia and microvascular dysfunction. It also implies local hypoxia in a part of a body resulting from constriction. Ischemia causes not only insufficiency of oxygen, but also reduced availability of nutrients and inadequate removal of metabolic wastes. Ischemia can be partial or total blockage. The inadequate delivery of oxygenated blood to the organs must be resolved either by treating the cause of the inadequate delivery or reducing the oxygen demand of the system that needs it. For example, patients with myocardial ischemia have a decreased blood flow to the heart and are prescribed with medications that reduce chronotrophy and ionotrophy to meet the new level of blood delivery supplied by the stenosed vasculature so that it is adequate.

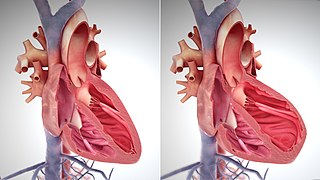
The endocardium is the innermost layer of tissue that lines the chambers of the heart. Its cells are embryologically and biologically similar to the endothelial cells that line blood vessels. The endocardium also provides protection to the valves and heart chambers.

Reperfusion injury, sometimes called ischemia-reperfusion injury (IRI) or reoxygenation injury, is the tissue damage caused when blood supply returns to tissue after a period of ischemia or lack of oxygen. The absence of oxygen and nutrients from blood during the ischemic period creates a condition in which the restoration of circulation results in inflammation and oxidative damage through the induction of oxidative stress rather than restoration of normal function.
In cardiology, hibernating myocardium is a state when some segments of the myocardium exhibit abnormalities of contractile function. These abnormalities can be visualised with echocardiography, cardiac magnetic resonance imaging (CMR), nuclear medicine (PET) or ventriculography. Echocardiography: A wall motion abnormality at rest which improves during a low-dose dobutamine stress test is classified as "hibernating myocardium." Low dose dobutamine stimulates contractile function and thus helps to predict functional recovery after revascularization. Cardiac magnetic resonance: The most frequently used MR contrast agents based on Gd-chelates accumulate in the extracellular space which is increased in scarred myocardium. This leads to a signal increase which can be visualised with the "late gadolinium enhancement technique." This is probably the most accurate way to visualise scarred myocardium. An alternative (or additional) technique with CMR is the use of low dose dobutamine similar to echocardiography. PET: The finding of a perfusion or metabolic mismatch between PET-FDG and PET-NH3 is indicative of decreased metabolism. The wall of the affected segments is hypo-, a-, or dyskinetic.
Ischemic preconditioning (IPC) is an experimental technique for producing resistance to the loss of blood supply, and thus oxygen, to tissues of many types. In the heart, IPC is an intrinsic process whereby repeated short episodes of ischaemia protect the myocardium against a subsequent ischaemic insult. It was first identified in 1986 by Murry et al. This group exposed anesthetised open-chest dogs to four periods of 5 minute coronary artery occlusions followed by a 5-minute period of reperfusion before the onset of a 40-minute sustained occlusion of the coronary artery. The control animals had no such period of “ischaemic preconditioning” and had much larger infarct sizes compared with the dogs that did. The exact molecular pathways behind this phenomenon have yet to be fully understood.

Myocardial perfusion imaging or scanning is a nuclear medicine procedure that illustrates the function of the heart muscle (myocardium).
No reflow phenomenon is the failure of blood to reperfuse an ischemic area after the physical obstruction has been removed or bypassed. The underlying mechanism is related to arterial microvasculature damage. It is primarily seen during percutaneous coronary intervention (PCI) in the setting of acute myocardial infarction (AMI), but has also been observed in other organs, including the brain and kidneys. Coronary no-reflow phenomenon is specifically related to reduced antegrade coronary blood flow despite proximal coronary artery patency. It is an independent predictor of worse clinical outcomes including heart failure, fatal arrhythmias, myocardial infarction, and increased mortality rates.

Anomalous left coronary artery from the pulmonary artery is a rare congenital anomaly occurring in approximately 1 in 300,000 liveborn children. The diagnosis comprises between 0.24 and 0.46% of all cases of congenital heart disease. The anomalous left coronary artery (LCA) usually arises from the pulmonary artery instead of the aortic sinus. In fetal life, the high pressure in the pulmonic artery and the fetal shunts enable oxygen-rich blood to flow in the LCA. By the time of birth, the pressure will decrease in the pulmonic artery and the child will have a postnatal circulation. The myocardium which is supplied by the LCA, will therefore be dependent on collateral blood flow from the other coronary arteries, mainly the RCA. Because the pressure in RCA exceeds the pressure in LCA a collateral circulation will increase. This situation ultimately can lead to blood flowing from the RCA into the LCA retrograde and into the pulmonary artery, thus forming a left-to-right shunt.

Coronary perfusion pressure (CPP) refers to the pressure gradient that drives coronary blood pressure. The heart's function is to perfuse blood to the body; however, the heart's own myocardium must, itself, be supplied for its own muscle function. The heart is supplied by coronary vessels, and therefore CPP is the blood pressure within those vessels. If pressures are too low in the coronary vasculature, then the myocardium risks ischemia with subsequent myocardial infarction or cardiogenic shock.

Reperfusion therapy is a medical treatment to restore blood flow, either through or around, blocked arteries, typically after a heart attack. Reperfusion therapy includes drugs and surgery. The drugs are thrombolytics and fibrinolytics used in a process called thrombolysis. Surgeries performed may be minimally-invasive endovascular procedures such as a percutaneous coronary intervention (PCI), which involves coronary angioplasty. The angioplasty uses the insertion of a balloon and/or stents to open up the artery. Other surgeries performed are the more invasive bypass surgeries that graft arteries around blockages.
A diagnosis of myocardial infarction is created by integrating the history of the presenting illness and physical examination with electrocardiogram findings and cardiac markers. A coronary angiogram allows visualization of narrowings or obstructions on the heart vessels, and therapeutic measures can follow immediately. At autopsy, a pathologist can diagnose a myocardial infarction based on anatomopathological findings.

Cardiac magnetic resonance imaging perfusion, also known as stress CMR perfusion, is a clinical magnetic resonance imaging test performed on patients with known or suspected coronary artery disease to determine if there are perfusion defects in the myocardium of the left ventricle that are caused by narrowing of one or more of the coronary arteries.

Cariporide is a selective Na+/H+ exchange inhibitor. Cariporide has been shown to actively suppress the cell death caused by oxidative stress.

Rottlerin (mallotoxin) is a polyphenol natural product isolated from the Asian tree Mallotus philippensis. Rottlerin displays a complex spectrum of pharmacology.
Cardioprotection includes all mechanisms and means that contribute to the preservation of the heart by reducing or even preventing myocardial damage. Cardioprotection encompasses several regimens that have shown to preserve function and viability of cardiac muscle cell tissue subjected to ischemic insult or reoxygenation. Cardioprotection includes strategies that are implemented before an ischemic event, during an ischemic event and after the event and during reperfusion. These strategies can be further stratified by performing the intervention locally or remotely, creating classes of conditioning known as remote ischemic PC (RIPC), remote ischemic PostC and remote ischemic PerC. Classical (local) preconditioning has an early phase with an immediate onset lasting 2–3 hours that protects against myocardial infarction. The early phase involves post-translational modification of preexisting proteins, brought about by the activation of G protein-coupled receptors as well as downstream MAPK's and PI3/Akt. These signaling events act on the ROS-generating mitochondria, activate PKCε and the Reperfusion Injury Salvage Kinase (RISK) pathway, preventing mitochondrial permeability transition pore (MTP) opening. The late phase with an onset of 12–24 hours that lasts 3–4 days and protects against both infarction and reversible postischemic contractile dysfunction, termed myocardial stunning. This phase involves the synthesis of new cardioprotective proteins stimulated by nitric oxide (NO), ROS and adenosine acting on kinases such as PKCε and Src, which in turn activate gene transcription and upregulation of late PC molecular players.
Remote ischemic conditioning (RIC) is an experimental medical procedure that aims to reduce the severity of ischaemic injury to an organ such as the heart or the brain, most commonly in the situation of a heart attack or a stroke, or during procedures such as heart surgery when the heart may temporary suffer ischaemia during the operation, by triggering the body's natural protection against tissue injury. Although noted to have some benefits in experimental models in animals, this is still an experimental procedure in humans and initial evidence from small studies have not been replicated in larger clinical trials. Successive clinical trials have failed to identify evidence supporting a protective role in humans.
The main pathophysiology of heart failure is a reduction in the efficiency of the heart muscle, through damage or overloading. As such, it can be caused by a wide number of conditions, including myocardial infarction, hypertension and cardiac amyloidosis. Over time these increases in workload will produce changes to the heart itself:

Roberto Ferrari is an Italian cardiologist who currently holds the position of Emeritus Professor at the University of Ferrara, where besides he was the chair of the Cardiology in the School of Medicine until the 2019–2020 academic year.