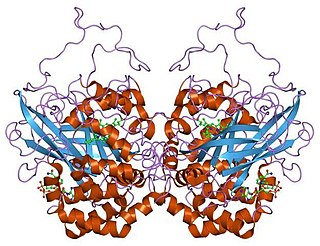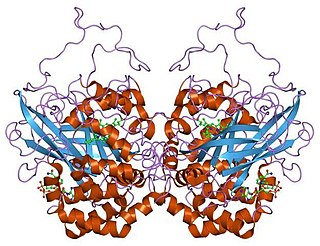
Catalase is a common enzyme found in nearly all living organisms exposed to oxygen which catalyzes the decomposition of hydrogen peroxide to water and oxygen. It is a very important enzyme in protecting the cell from oxidative damage by reactive oxygen species (ROS). Catalase has one of the highest turnover numbers of all enzymes; one catalase molecule can convert millions of hydrogen peroxide molecules to water and oxygen each second.

Heme, or haem, is a ring-shaped iron-containing molecular component of hemoglobin, which is necessary to bind oxygen in the bloodstream. It is composed of four pyrrole rings with 2 vinyl and 2 propionic acid side chains. Heme is biosynthesized in both the bone marrow and the liver.

Hypochlorous acid is an inorganic compound with the chemical formula ClOH, also written as HClO, HOCl, or ClHO. Its structure is H−O−Cl. It is an acid that forms when chlorine dissolves in water, and itself partially dissociates, forming hypochlorite anion, ClO−. HClO and ClO− are oxidizers, and the primary disinfection agents of chlorine solutions. HClO cannot be isolated from these solutions due to rapid equilibration with its precursor, chlorine.

Chronic granulomatous disease (CGD), also known as Bridges–Good syndrome, chronic granulomatous disorder, and Quie syndrome, is a diverse group of hereditary diseases in which certain cells of the immune system have difficulty forming the reactive oxygen compounds used to kill certain ingested pathogens. This leads to the formation of granulomas in many organs. CGD affects about 1 in 200,000 people in the United States, with about 20 new cases diagnosed each year.

Granulomatosis with polyangiitis (GPA), also known as Wegener's granulomatosis (WG), after the German physician Friedrich Wegener, is a rare long-term systemic disorder that involves the formation of granulomas and inflammation of blood vessels (vasculitis). It is an autoimmune disease and a form of vasculitis that affects small- and medium-size vessels in many organs but most commonly affects the upper respiratory tract, lungs and kidneys. The signs and symptoms of GPA are highly varied and reflect which organs are supplied by the affected blood vessels. Typical signs and symptoms include nosebleeds, stuffy nose and crustiness of nasal secretions, and inflammation of the uveal layer of the eye. Damage to the heart, lungs and kidneys can be fatal.

In chemistry, hypochlorite, or chloroxide is an anion with the chemical formula ClO−. It combines with a number of cations to form hypochlorite salts. Common examples include sodium hypochlorite and calcium hypochlorite. The Cl-O distance in ClO− is 1.69 Å.

Myeloperoxidase deficiency is a disorder featuring lack in either the quantity or the function of myeloperoxidase–an iron-containing protein expressed primarily in neutrophil granules. There are two types of myeloperoxidase deficiency: primary/inherited and secondary/acquired. Lack of functional myeloperoxidase leads to less efficient killing of intracellular pathogens, particularly Candida albicans, as well as less efficient production and release of neutrophil extracellular traps (NETs) from the neutrophils to trap and kill extracellular pathogens. Despite these characteristics, more than 95% of individuals with myeloperoxidase deficiency experience no symptoms in their lifetime. For those who do experience symptoms, the most common symptom is frequent infections by Candida albicans. Individuals with myeloperoxidase deficiency also experience higher rates of chronic inflammatory conditions. Myeloperoxidase deficiency is diagnosed using flow cytometry or cytochemical stains. There is no treatment for myeloperoxidase deficiency itself. Rather, in the rare cases that individuals experience symptoms, these infections should be treated.

Anti-neutrophil cytoplasmic antibodies (ANCAs) are a group of autoantibodies, mainly of the IgG type, against antigens in the cytoplasm of neutrophils and monocytes. They are detected as a blood test in a number of autoimmune disorders, but are particularly associated with systemic vasculitis, so called ANCA-associated vasculitides (AAV).
Respiratory burst is the rapid release of the reactive oxygen species (ROS), superoxide anion and hydrogen peroxide, from different cell types.
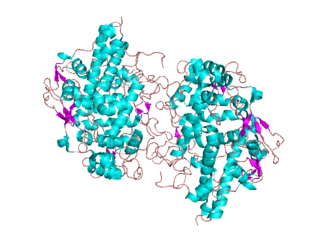
NADPH oxidase is a membrane-bound enzyme complex that faces the extracellular space. It can be found in the plasma membrane as well as in the membranes of phagosomes used by neutrophil white blood cells to engulf microorganisms. Human isoforms of the catalytic component of the complex include NOX1, NOX2, NOX3, NOX4, NOX5, DUOX1, and DUOX2.
Microscopic polyangiitis is an autoimmune disease characterized by a systemic, pauci-immune, necrotizing, small-vessel vasculitis without clinical or pathological evidence of granulomatous inflammation.

Hemopexin, also known as beta-1B-glycoprotein, is a glycoprotein that in humans is encoded by the HPX gene and belongs to the hemopexin family of proteins. Hemopexin is the plasma protein with the highest binding affinity for heme.

Proteinase 3, also known as PRTN3, is an enzyme that in humans is encoded by the PRTN3 gene.

Sulfite oxidase is an enzyme in the mitochondria of all eukaryotes, with exception of the yeasts. It oxidizes sulfite to sulfate and, via cytochrome c, transfers the electrons produced to the electron transport chain, allowing generation of ATP in oxidative phosphorylation. This is the last step in the metabolism of sulfur-containing compounds and the sulfate is excreted.

p-ANCA, or MPO-ANCA, or perinuclear anti-neutrophil cytoplasmic antibodies, are antibodies that stain the material around the nucleus of a neutrophil. They are a special class of anti-neutrophil cytoplasmic antibodies.
Animal heme-dependent peroxidases is a family of peroxidases. Peroxidases are found in bacteria, fungi, plants and animals. On the basis of sequence similarity, a number of animal heme peroxidases can be categorized as members of a superfamily: myeloperoxidase (MPO); eosinophil peroxidase (EPO); lactoperoxidase (LPO); thyroid peroxidase (TPO); prostaglandin H synthase (PGHS); and peroxidasin.
Haloperoxidases are peroxidases that are able to mediate the oxidation of halides by hydrogen peroxide. Both halides and hydrogen peroxide are widely available in the environment.

Necrotizing vasculitis, also called systemic necrotizing vasculitis, is a general term for the inflammation of veins and arteries that develops into necrosis and narrows the vessels.
Ronald Jonathan Falk, MD, FACP, FASN is the Nan and Hugh Cullman Eminent Professor and Chair of the Department of Medicine at the University of North Carolina-Chapel Hill (UNC). He is a clinical nephrologist and internationally recognized expert in anti-neutrophil cytoplasmic autoantibody (ANCA)-induced vasculitis and autoimmune kidney disease. His career as a translational physician-scientist spans more than three decades. His clinical practice and translational research focus on characterizing the cell, tissue and physiologic changes in the development of specific autoimmune kidney diseases and developing new approaches for studying autoimmunity, inflammation and basic neutrophil/monocyte biology. He was Chief of the UNC Division of Nephrology and Hypertension from 1993-2015. He co-founded the UNC Kidney Center in 2005 and continues as Co-Director. Falk is a Past-President of the American Society of Nephrology (ASN). Since 2015, he has served as Chair of the Department of Medicine at UNC.

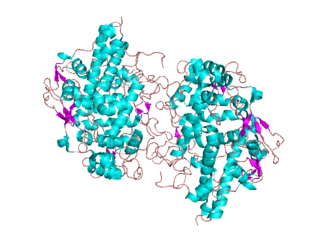
Eosinophil peroxidase is an enzyme found within the eosinophil granulocytes, innate immune cells of humans and mammals. This oxidoreductase protein is encoded by the gene EPX, expressed within these myeloid cells. EPO shares many similarities with its orthologous peroxidases, myeloperoxidase (MPO), lactoperoxidase (LPO), and thyroid peroxidase (TPO). The protein is concentrated in secretory granules within eosinophils. Eosinophil peroxidase is a heme peroxidase, its activities including the oxidation of halide ions to bacteriocidal reactive oxygen species, the cationic disruption of bacterial cell walls, and the post-translational modification of protein amino acid residues.