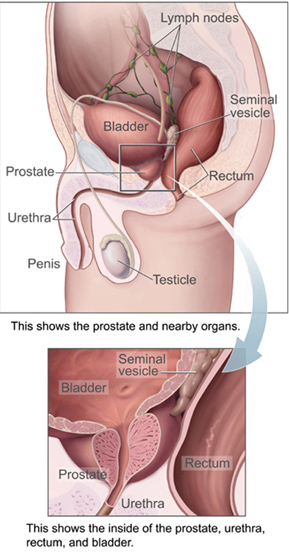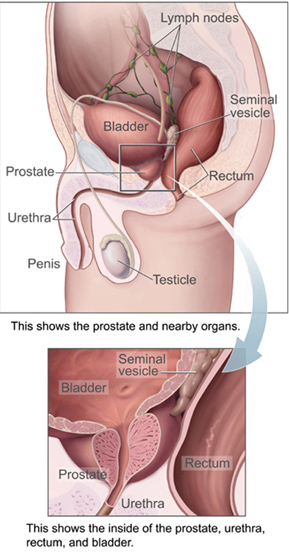
The prostate is both an accessory gland of the male reproductive system and a muscle-driven mechanical switch between urination and ejaculation. It is found in all male mammals. It differs between species anatomically, chemically, and physiologically. Anatomically, the prostate is found below the bladder, with the urethra passing through it. It is described in gross anatomy as consisting of lobes and in microanatomy by zone. It is surrounded by an elastic, fibromuscular capsule and contains glandular tissue, as well as connective tissue.

Prostate cancer is the uncontrolled growth of cells in the prostate, a gland in the male reproductive system below the bladder. Early prostate cancer causes no symptoms. Abnormal growth of prostate tissue is usually detected through screening tests, typically blood tests that check for prostate-specific antigen (PSA) levels. Those with high levels of PSA in their blood are at increased risk for developing prostate cancer. Diagnosis requires a biopsy of the prostate. If cancer is present, the pathologist assigns a Gleason score, and a higher score represents a more dangerous tumor. Medical imaging is performed to look for cancer that has spread outside the prostate. Based on the Gleason score, PSA levels, and imaging results, a cancer case is assigned a stage 1 to 4. A higher stage signifies a more advanced, more dangerous disease.

Benign prostatic hyperplasia (BPH), also called prostate enlargement, is a noncancerous increase in size of the prostate gland. Symptoms may include frequent urination, trouble starting to urinate, weak stream, inability to urinate, or loss of bladder control. Complications can include urinary tract infections, bladder stones, and chronic kidney problems.
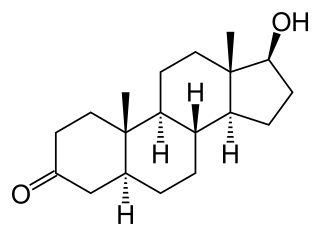
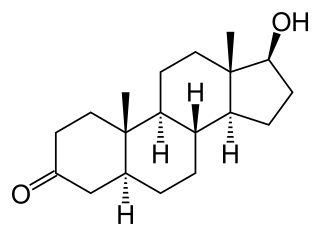
Dihydrotestosterone is an endogenous androgen sex steroid and hormone primarily involved in the growth and repair of the prostate and the penis, as well as the production of sebum and body hair composition.
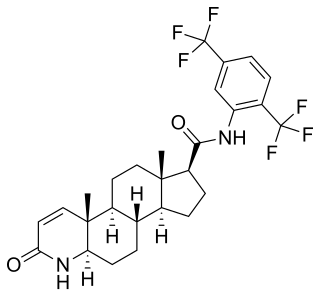
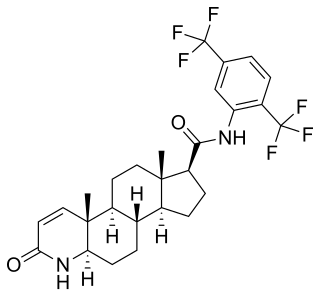
Dutasteride, sold under the brand name Avodart among others, is a medication primarily used to treat the symptoms of a benign prostatic hyperplasia (BPH), an enlarged prostate not associated with cancer. A few months may be required before benefits occur. It is also used for scalp hair loss in men and as a part of hormone therapy in transgender women. It is usually taken by mouth.

Prostate biopsy is a procedure in which small hollow needle-core samples are removed from a man's prostate gland to be examined for the presence of prostate cancer. It is typically performed when the result from a PSA blood test is high. It may also be considered advisable after a digital rectal exam (DRE) finds possible abnormality. PSA screening is controversial as PSA may become elevated due to non-cancerous conditions such as benign prostatic hyperplasia (BPH), by infection, or by manipulation of the prostate during surgery or catheterization. Additionally many prostate cancers detected by screening develop so slowly that they would not cause problems during a man's lifetime, making the complications due to treatment unnecessary.

Prostatic acid phosphatase (PAP), also prostatic specific acid phosphatase (PSAP), is an enzyme produced by the prostate. It may be found in increased amounts in men who have prostate cancer or other diseases.
Prostate cancer screening is the screening process used to detect undiagnosed prostate cancer in men without signs or symptoms. When abnormal prostate tissue or cancer is found early, it may be easier to treat and cure, but it is unclear if early detection reduces mortality rates.
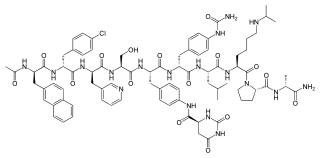
Kallikreins are a subgroup of serine proteases, enzymes capable of cleaving peptide bonds in proteins. In humans, plasma kallikrein has no known paralogue, while tissue kallikrein-related peptidases (KLKs) encode a family of fifteen closely related serine proteases. These genes are localised to chromosome 19q13, forming the largest contiguous cluster of proteases within the human genome. Kallikreins are responsible for the coordination of various physiological functions including blood pressure, semen liquefaction and skin desquamation.
Early prostate cancer antigen-2 (EPCA-2) is a protein of which blood levels are elevated in prostate cancer. It appears to provide more accuracy in identifying early prostate cancer than the standard prostate cancer marker, PSA.

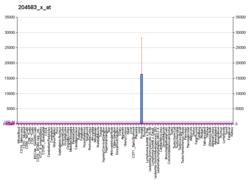
Kallikrein-related peptidase 4 is a protein which in humans is encoded by the KLK4 gene.
Lower urinary tract symptoms (LUTS) refer to a group of clinical symptoms involving the bladder, urinary sphincter, urethra and, in men, the prostate. The term is more commonly applied to men – over 40% of older men are affected – but lower urinary tract symptoms also affect women. The condition is also termed prostatism in men, but LUTS is preferred.

Brachytherapy is a type of radiotherapy, or radiation treatment, offered to certain cancer patients. There are two types of brachytherapy – high dose-rate (HDR) and low dose-rate (LDR). LDR brachytherapy is the one most commonly used to treat prostate cancer. It may be referred to as 'seed implantation' or it may be called 'pinhole surgery'.

Prostate cancer antigen 3 is a gene that expresses a non-coding RNA. PCA3 is only expressed in human prostate tissue, and the gene is highly overexpressed in prostate cancer. Because of its restricted expression profile, the PCA3 RNA is useful as a tumor marker.
Degarelix, sold under the brand name Firmagon among others, is a hormonal therapy used in the treatment of prostate cancer.

The objective of cancer screening is to detect cancer before symptoms appear, involving various methods such as blood tests, urine tests, DNA tests, and medical imaging. The purpose of screening is early cancer detection, to make the cancer easier to treat and extending life expectancy. In 2019, cancer was the second leading cause of death globally; more recent data is pending due to the COVID-19 pandemic.
Treatment for prostate cancer may involve active surveillance, surgery, radiation therapy – including brachytherapy and external-beam radiation therapy, proton therapy, high-intensity focused ultrasound (HIFU), cryosurgery, hormonal therapy, chemotherapy, or some combination. Treatments also extend to survivorship based interventions. These interventions are focused on five domains including: physical symptoms, psychological symptoms, surveillance, health promotion and care coordination. However, a published review has found only high levels of evidence for interventions that target physical and psychological symptom management and health promotion, with no reviews of interventions for either care coordination or surveillance. The favored treatment option depends on the stage of the disease, the Gleason score, and the PSA level. Other important factors include the man's age, his general health, and his feelings about potential treatments and their possible side-effects. Because all treatments can have significant side-effects, such as erectile dysfunction and urinary incontinence, treatment discussions often focus on balancing the goals of therapy with the risks of lifestyle alterations.

Active surveillance is a management option for localized prostate cancer that can be offered to appropriate patients who would also be candidates for aggressive local therapies, with the intent to intervene if the disease progresses. Active surveillance should not be confused with watchful waiting, another observational strategy for men that would not be candidates for curative therapy because of a limited life expectancy. Active surveillance offers men with a prostate cancer that is thought to have a low risk of causing harm in the absence of treatment, a chance to delay or avoid aggressive treatment and its associated side effects. While prostate cancer is the most common non-cutaneous cancer and second leading cause of cancer-related death in American men, it is conservatively estimated that approximately 100,000 men per year in the United States who would be eligible for conservative treatment through active surveillance, undergo unnecessary treatments. The management of localized prostate cancer is controversial and men with localized disease diagnosed today often undergo treatments with significant side effects that will not improve overall health outcomes. The 2011 NIH State-of-the-Science Conference Statement on the "Role of active surveillance in the management of men with localized prostate cancer" pointed out the many unanswered questions about observational strategies for prostate cancer that require further research and clarification. These included:
Andrew Julian Vickers is a biostatistician and attending research methodologist at Memorial Sloan Kettering Cancer Center. Since 2013, he has also been professor of public health at Weill Cornell Medical College. He is the statistical editor for the peer-reviewed journal European Urology.

GTx-758 is a synthetic nonsteroidal estrogen which was under development by GTx, Inc. for the treatment of advanced prostate cancer. As of 2016, it had completed two phase II clinical trials.