Mesothelioma is a type of cancer that develops from the thin layer of tissue that covers many of the internal organs. The area most commonly affected is the lining of the lungs and chest wall. Less commonly the lining of the abdomen and rarely the sac surrounding the heart, or the sac surrounding the testis may be affected. Signs and symptoms of mesothelioma may include shortness of breath due to fluid around the lung, a swollen abdomen, chest wall pain, cough, feeling tired, and weight loss. These symptoms typically come on slowly.

A bone tumor is an abnormal growth of tissue in bone, traditionally classified as noncancerous (benign) or cancerous (malignant). Cancerous bone tumors usually originate from a cancer in another part of the body such as from lung, breast, thyroid, kidney and prostate. There may be a lump, pain, or neurological signs from pressure. A bone tumor might present with a pathologic fracture. Other symptoms may include fatigue, fever, weight loss, anemia and nausea. Sometimes there are no symptoms and the tumour is found when investigating another problem.

Fibromas are benign tumors that are composed of fibrous or connective tissue. They can grow in all organs, arising from mesenchyme tissue. The term "fibroblastic" or "fibromatous" is used to describe tumors of the fibrous connective tissue. When the term fibroma is used without modifier, it is usually considered benign, with the term fibrosarcoma reserved for malignant tumors.

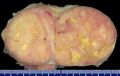
Sex cord–gonadal stromal tumour is a group of tumors derived from the stromal component of the ovary and testis, which comprises the granulosa, thecal cells and fibrocytes. In contrast, the epithelial cells originate from the outer epithelial lining surrounding the gonad while the germ cell tumors arise from the precursor cells of the gametes, hence the name germ cell. In humans, this group accounts for 8% of ovarian cancers and under 5% of testicular cancers. Their diagnosis is histological: only a biopsy of the tumour can make an exact diagnosis. They are often suspected of being malignant prior to operation, being solid ovarian tumours that tend to occur most commonly in post menopausal women.
In medicine, Meigs's syndrome, also Meigs syndrome or Demons–Meigs syndrome, is the triad of ascites, pleural effusion, and benign ovarian tumor. Meigs syndrome resolves after the resection of the tumor. Because the transdiaphragmatic lymphatic channels are larger in diameter on the right, the pleural effusion is classically on the right side. The causes of the ascites and pleural effusion are poorly understood. Atypical Meigs syndrome, characterized by a benign pelvic mass with right-sided pleural effusion but without ascites, can also occur. As in typical Meigs syndrome, pleural effusion resolves after removal of the pelvic mass.
The International Classification of Diseases for Oncology (ICD-O) is a domain-specific extension of the International Statistical Classification of Diseases and Related Health Problems for tumor diseases. This classification is widely used by cancer registries.

A hemangiopericytoma is a type of soft-tissue sarcoma that originates in the pericytes in the walls of capillaries. When inside the nervous system, although not strictly a meningioma tumor, it is a meningeal tumor with a special aggressive behavior. It was first characterized in 1942.

Aneurysmal bone cyst (ABC) is a non-cancerous bone tumor composed of multiple varying sizes of spaces in a bone which are filled with blood. The term is a misnomer, as the lesion is neither an aneurysm nor a cyst. It generally presents with pain and swelling in the affected bone. Pressure on neighbouring tissues may cause compression effects such as neurological symptoms.

An odontogenic keratocyst is a rare and benign but locally aggressive developmental cyst. It most often affects the posterior mandible and most commonly presents in the third decade of life. Odontogenic keratocysts make up around 19% of jaw cysts.

An ameloblastic fibroma is a fibroma of the ameloblastic tissue, that is, an odontogenic tumor arising from the enamel organ or dental lamina. It may be either truly neoplastic or merely hamartomatous. In neoplastic cases, it may be labeled an ameloblastic fibrosarcoma in accord with the terminological distinction that reserves the word fibroma for benign tumors and assigns the word fibrosarcoma to malignant ones. It is more common in the first and second decades of life, when odontogenesis is ongoing, than in later decades. In 50% of cases an unerupted tooth is involved.

Adenocarcinoma in situ (AIS) of the lung —previously included in the category of "bronchioloalveolar carcinoma" (BAC)—is a subtype of lung adenocarcinoma. It tends to arise in the distal bronchioles or alveoli and is defined by a non-invasive growth pattern. This small solitary tumor exhibits pure alveolar distribution and lacks any invasion of the surrounding normal lung. If completely removed by surgery, the prognosis is excellent with up to 100% 5-year survival.
Pleural disease occurs in the pleural space, which is the thin fluid-filled area in between the two pulmonary pleurae in the human body. There are several disorders and complications that can occur within the pleural area, and the surrounding tissues in the lung.
Infantile digital fibromatosis (IDF), also termed inclusion body fibromatosis, Reye tumor, or Reye's tumor, usually occurs as a single, small, asymptomatic, nodule in the dermis on a finger or toe of infants and young children. IMF is a rare disorder with approximately 200 cases reported in the medical literature as of 2021. The World Health Organization in 2020 classified these nodules as a specific benign tumor type in the category of fibroblastic and myofibroblastic tumors. IDF was first described by the Australian pathologist, Douglas Reye, in 1965.
Mucinous cystadenocarcinoma of the lung (MCACL) is a very rare malignant mucus-producing neoplasm arising from the uncontrolled growth of transformed epithelial cells originating in lung tissue.
Cardiac fibroma, also known as cardiac fibromatosis, cardiac fibrous hamartoma, fibroelastic hamartoma of heart and fibroma of heart is the second highest type of primary cardiac tumor seen in infants and children. This benign tumor made by connective tissue and fibroblast is largely observed in the ventricles of the heart. The left ventricle is the most common location of cardiac fibroma and accounts for approximately 57% of cardiac fibroma cases followed by the right ventricle with 27.5% of cases. Symptoms of the disease depend on the size of the tumor, its location relative to the conduction system, and whether it obstructs blood flow. Two-thirds of children with this tumor are asymptomatic, showing no signs and symptoms. Therefore the cause of cardiac fibroma is unexplained but has been associated with Gorlin Syndrome. Echocardiography is the primarily diagnostic method used to detect if an individual has cardiac fibroma. Resection of the tumor is recommended however heart transplantation is done if surgery is not possible. Overall prognosis of resection is favorable and the chance of recurrence is scarcely reported.

Mammary-type myofibroblastoma (MFB), also named mammary and extramammary myofibroblastoma, was first termed myofibrolastoma of the breast, or, more simply, either mammary myofibroblastoma (MMFB) or just myofibroblastoma. The change in this terminology occurred because the initial 1987 study and many subsequent studies found this tumor only in breast tissue. However, a 2001 study followed by numerous reports found tumors with the microscopic histopathology and other key features of mammary MFB in a wide range of organs and tissues. Further complicating the issue, early studies on MFB classified it as one of various types of spindle cell tumors that, except for MFB, were ill-defined. These other tumors, which have often been named interchangeably in different reports, are: myelofibroblastoma, benign spindle cell tumor, fibroma, spindle cell lipoma, myogenic stromal tumor, and solitary stromal tumor. Finally, studies suggest that spindle cell lipoma and cellular angiofibroma are variants of MFB. Here, the latter two tumors are tentatively classified as MFB variants but otherwise MFB is described as it is more strictly defined in most recent publications. The World Health Organization in 2020 classified mammary type myofibroblastoma tumors and myofibroblastoma tumors as separate tumor forms within the category of fibroblastic and myofibroblastic tumors.

Asbestos-related diseases are disorders of the lung and pleura caused by the inhalation of asbestos fibres. Asbestos-related diseases include non-malignant disorders such as asbestosis, diffuse pleural thickening, pleural plaques, pleural effusion, rounded atelectasis and malignancies such as lung cancer and malignant mesothelioma.
Hyperthermic intrathoracic chemotherapy (HITOC) is part of a surgical strategy employed in the treatment of various pleural malignancies. The pleura in this situation could be considered to include the surface linings of the chest wall, lungs, mediastinum, and diaphragm. HITOC is the chest counterpart of HIPEC. Traditionally used in the treatment of malignant mesothelioma, a primary malignancy of the pleura, this modality has recently been evaluated in the treatment of secondary pleural malignancies.
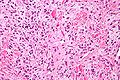
Fibroblastic and myofibroblastic tumors (FMTs) develop from the mesenchymal stem cells which differentiate into fibroblasts and/or the myocytes/myoblasts that differentiate into muscle cells. FMTs are a heterogeneous group of soft tissue neoplasms. The World Health Organization (2020) defined tumors as being FMTs based on their morphology and, more importantly, newly discovered abnormalities in the expression levels of key gene products made by these tumors' neoplastic cells. Histopathologically, FMTs consist of neoplastic connective tissue cells which have differented into cells that have microscopic appearances resembling fibroblasts and/or myofibroblasts. The fibroblastic cells are characterized as spindle-shaped cells with inconspicuous nucleoli that express vimentin, an intracellular protein typically found in mesenchymal cells, and CD34, a cell surface membrane glycoprotein. Myofibroblastic cells are plumper with more abundant cytoplasm and more prominent nucleoli; they express smooth muscle marker proteins such as smooth muscle actins, desmin, and caldesmon. The World Health Organization further classified FMTs into four tumor forms based on their varying levels of aggressiveness: benign, intermediate, intermediate, and malignant.
Angiofibroma of soft tissue (AFST), also termed angiofibroma, not otherwise specified, is a recently recognized and rare disorder that was classified in the category of benign fibroblastic and myofibroblastic tumors by the World Health Organization in 2020. An AFST tumor is a neoplasm that was first described by A. Mariño-Enríquez and C.D. Fletcher in 2012.