Hemicorporectomy is a radical surgery in which the body below the waist is amputated, transecting the lumbar spine. This removes the legs, the genitalia, urinary system, pelvic bones, anus, and rectum. It is an extremely mutilating procedure recommended only as a last resort for people with severe and potentially fatal illnesses such as osteomyelitis, tumors, severe traumas and intractable decubiti in, or around, the pelvis. By 2009, 66 cases have been reported in medical literature. The most recent documented operation was in September 2019.

Cervical spine disorders are illnesses that affect the cervical spine, which is made up of the upper first seven vertebrae, encasing and shielding the spinal cord. This fragment of the spine starts from the region above the shoulder blades and ends by supporting and connecting the skull.

Major trauma is any injury that has the potential to cause prolonged disability or death. There are many causes of major trauma, blunt and penetrating, including falls, motor vehicle collisions, stabbing wounds, and gunshot wounds. Depending on the severity of injury, quickness of management, and transportation to an appropriate medical facility may be necessary to prevent loss of life or limb. The initial assessment is critical, and involves a physical evaluation and also may include the use of imaging tools to determine the types of injuries accurately and to formulate a course of treatment.

Clearing the cervical spine is the process by which medical professionals determine whether cervical spine injuries exist, mainly regarding cervical fracture. It is generally performed in cases of major trauma. This process can take place in the emergency department or in the field by appropriately trained EMS personnel.
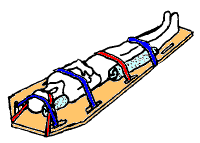
A spinal board, is a patient handling device used primarily in pre-hospital trauma care. It is designed to provide rigid support during movement of a person with suspected spinal or limb injuries. They are most commonly used by ambulance staff, as well as lifeguards and ski patrollers. Historically, backboards were also used in an attempt to "improve the posture" of young people, especially girls.

Spondylosis is the degeneration of the vertebral column from any cause. In the more narrow sense it refers to spinal osteoarthritis, the age-related wear and tear of the spinal column, which is the most common cause of spondylosis. The degenerative process in osteoarthritis chiefly affects the vertebral bodies, the neural foramina and the facet joints. If severe, it may cause pressure on the spinal cord or nerve roots with subsequent sensory or motor disturbances, such as pain, paresthesia, imbalance, and muscle weakness in the limbs.

A spinal cord injury (SCI) is damage to the spinal cord that causes temporary or permanent changes in its function. Symptoms may include loss of muscle function, sensation, or autonomic function in the parts of the body served by the spinal cord below the level of the injury. Injury can occur at any level of the spinal cord and can be complete, with a total loss of sensation and muscle function at lower sacral segments, or incomplete, meaning some nervous signals are able to travel past the injured area of the cord up to the Sacral S4-5 spinal cord segments. Depending on the location and severity of damage, the symptoms vary, from numbness to paralysis, including bowel or bladder incontinence. Long term outcomes also range widely, from full recovery to permanent tetraplegia or paraplegia. Complications can include muscle atrophy, loss of voluntary motor control, spasticity, pressure sores, infections, and breathing problems.

A cervical collar, also known as a neck brace, is a medical device used to support a person's neck. It is also applied by emergency personnel to those who have had traumatic head or neck injuries, and can be used to treat chronic medical conditions.

The scoop stretcher is a device used specifically for moving injured people. It is ideal for carrying casualties with possible spinal injuries.

A cervical fracture, commonly called a broken neck, is a fracture of any of the seven cervical vertebrae in the neck. Examples of common causes in humans are traffic collisions and diving into shallow water. Abnormal movement of neck bones or pieces of bone can cause a spinal cord injury resulting in loss of sensation, paralysis, or usually instant death.

Neurogenic shock is a distributive type of shock resulting in hypotension, often with bradycardia, caused by disruption of autonomic nervous system pathways. It can occur after damage to the central nervous system, such as spinal cord injury and traumatic brain injury. Low blood pressure occurs due to decreased systemic vascular resistance resulting from loss of sympathetic tone, which in turn causes blood pooling within the extremities rather than being available to circulate throughout the body. The slowed heart rate results from a vagal response unopposed by a sympathetic nervous system (SNS) response. Such cardiovascular instability is exacerbated by hypoxia, or treatment with endotracheal or endobronchial suction used to prevent pulmonary aspiration.

Central cord syndrome (CCS) is the most common form of cervical spinal cord injury. It is characterized by loss of motion and sensation in arms and hands. It usually results from trauma which causes damage to the neck, leading to major injury to the central corticospinal tract of the spinal cord. The syndrome is more common in people over the age of 50 because osteoarthritis in the neck region causes weakening of the vertebrae. CCS most frequently occurs among older persons with cervical spondylosis, however, it also may occur in younger individuals.

Penetrating trauma is an injury that occurs when an object pierces the skin and enters a tissue of the body, creating an open wound. The penetrating object may remain in the tissues, come back out the way it entered, or pass through the tissues and exit from another area. An injury in which an object enters the body or a structure and passes all the way through is called a perforating injury, while penetrating trauma implies that the object does not pass through. Perforating trauma is associated with an entrance wound and an often larger exit wound.

Brown-Séquard syndrome is caused by damage to one half of the spinal cord, i.e. hemisection of the spinal cord resulting in paralysis and loss of proprioception on the same side as the injury or lesion, and loss of pain and temperature sensation on the opposite side as the lesion. It is named after physiologist Charles-Édouard Brown-Séquard, who first described the condition in 1850.

Posterior cord syndrome (PCS), also known as posterior spinal artery syndrome (PSA), is a type of incomplete spinal cord injury. PCS is the least commonly occurring of the six clinical spinal cord injury syndromes, with an incidence rate of less than 1%.
Grady straps are a specific strapping configuration used in full body spinal immobilization.

A spinal fracture, also called a vertebral fracture or a broken back, is a fracture affecting the vertebrae of the spinal column. Most types of spinal fracture confer a significant risk of spinal cord injury. After the immediate trauma, there is a risk of spinal cord injury if the fracture is unstable, that is, likely to change alignment without internal or external fixation.

Spinal stenosis is an abnormal narrowing of the spinal canal or neural foramen that results in pressure on the spinal cord or nerve roots. Symptoms may include pain, numbness, or weakness in the arms or legs. Symptoms are typically gradual in onset and improve with bending forwards. Severe symptoms may include loss of bladder control, loss of bowel control, or sexual dysfunction.
Spinal cord injury without radiographic abnormality (SCIWORA) is symptoms of a spinal cord injury (SCI) with no evidence of injury to the spinal column on X-rays or CT scan. Symptoms may include numbness, weakness, abnormal reflexes, or loss of bladder or bowel control. Neck or back pain is also common. Symptoms may be brief or persistent. Some do not develop symptoms until a few days after the injury.

Bizhan Aarabi is an Iranian-American neurosurgeon, researcher, author and academic. He is Professor of Neurosurgery at University of Maryland and the Director of Neurotrauma at the R Adams Cowley Shock Trauma Center.