Orthostatic hypotension, also known as postural hypotension, is a medical condition wherein a person's blood pressure drops when standing up or sitting down. Primary orthostatic hypotension is also often referred to as neurogenic orthostatic hypotension. The drop in blood pressure may be sudden, within 3 minutes or gradual. It is defined as a fall in systolic blood pressure of at least 20 mmHg or diastolic blood pressure of at least 10 mmHg after 3 minutes of standing. It occurs predominantly by delayed constriction of the lower body blood vessels, which is normally required to maintain adequate blood pressure when changing the position to standing. As a result, blood pools in the blood vessels of the legs for a longer period, and less is returned to the heart, thereby leading to a reduced cardiac output and inadequate blood flow to the brain.

Dysautonomia, autonomic failure, or autonomic dysfunction is a condition in which the autonomic nervous system (ANS) does not work properly. This may affect the functioning of the heart, bladder, intestines, sweat glands, pupils, and blood vessels. Dysautonomia has many causes, not all of which may be classified as neuropathic. A number of conditions can feature dysautonomia, such as Parkinson's disease, multiple system atrophy, dementia with Lewy bodies, Ehlers–Danlos syndromes, autoimmune autonomic ganglionopathy and autonomic neuropathy, HIV/AIDS, mitochondrial cytopathy, pure autonomic failure, autism, and postural orthostatic tachycardia syndrome.

Sinus node dysfunction (SND), also known as sick sinus syndrome (SSS), is a group of abnormal heart rhythms (arrhythmias) usually caused by a malfunction of the sinus node, the heart's primary pacemaker. Tachycardia-bradycardia syndrome is a variant of sick sinus syndrome in which the arrhythmia alternates between fast and slow heart rates.

Palpitations are perceived abnormalities of the heartbeat characterized by awareness of cardiac muscle contractions in the chest, which is further characterized by the hard, fast and/or irregular beatings of the heart.
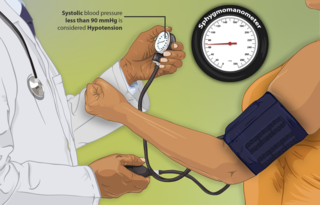
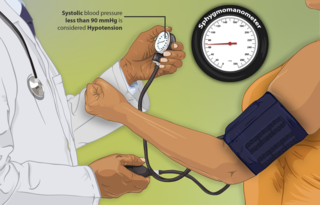
Hypotension, also known as low blood pressure, is a cardiovascular condition characterized by abnormally reduced blood pressure. Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps out blood and is indicated by two numbers, the systolic blood pressure and the diastolic blood pressure, which are the maximum and minimum blood pressures within the cardiac cycle, respectively. A systolic blood pressure of less than 90 millimeters of mercury (mmHg) or diastolic of less than 60 mmHg is generally considered to be hypotension. Different numbers apply to children. However, in practice, blood pressure is considered too low only if noticeable symptoms are present.

Dizziness is an imprecise term that can refer to a sense of disorientation in space, vertigo, or lightheadedness. It can also refer to disequilibrium or a non-specific feeling, such as giddiness or foolishness.

Reflex syncope is a brief loss of consciousness due to a neurologically induced drop in blood pressure and/or a decrease in heart rate. Before an affected person passes out, there may be sweating, a decreased ability to see, or ringing in the ears. Occasionally, the person may twitch while unconscious. Complications of reflex syncope include injury due to a fall.
Orthostatic intolerance (OI) is the development of symptoms when standing upright that are relieved when reclining. There are many types of orthostatic intolerance. OI can be a subcategory of dysautonomia, a disorder of the autonomic nervous system occurring when an individual stands up. Some animal species with orthostatic hypotension have evolved to cope with orthostatic disturbances.

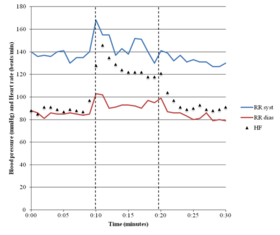
Postural orthostatic tachycardia syndrome (POTS) is a condition characterized by an abnormally large increase in heart rate upon sitting up or standing. POTS is a disorder of the autonomic nervous system that can lead the individual to experience a variety of symptoms. Symptoms may include lightheadedness, brain fog, blurred vision, weakness, fatigue, headaches, heart palpitations, exercise intolerance, nausea, diminished concentration, tremulousness (shaking), syncope (fainting), coldness or pain in the extremities, chest pain and shortness of breath. Other conditions associated with POTS include migraine headaches, Ehlers–Danlos syndrome, asthma, autoimmune disease, vasovagal syncope and mast cell activation syndrome. POTS symptoms may be treated with lifestyle changes such as increasing fluid and salt intake, wearing compression stockings, gentler and slow postural changes, avoiding prolonged bedrest, medication, increasing electrolyte intake, and physical therapy.

Sinus tachycardia is a sinus rhythm of the heart, with an increased rate of electrical discharge from the sinoatrial node, resulting in a tachycardia, a heart rate that is higher than the upper limit of normal.
Lightheadedness is a common and typically unpleasant sensation of dizziness or a feeling that one may faint. The sensation of lightheadedness can be short-lived, prolonged, or, rarely, recurring. In addition to dizziness, the individual may feel as though their head is weightless. The individual may also feel as though the room is "spinning" or moving (vertigo). Most causes of lightheadedness are not serious and either cure themselves quickly or are easily treated.

Pure autonomic failure (PAF) is an uncommon, sporadic neurodegenerative condition marked by a steadily declining autonomic regulation. Bradbury and Eggleston originally described pure autonomic failure in 1925.

Inappropriate sinus tachycardia (IST) is defined as sinus tachycardia that is not caused by identifiable medical ailments, a physiological reaction, or pharmaceuticals and is accompanied by symptoms, frequently invalidating and affecting quality of life. IST symptoms include palpitations, chest discomfort, exhaustion, shortness of breath, presyncope, and syncope.

Syncope, commonly known as fainting or passing out, is a loss of consciousness and muscle strength characterized by a fast onset, short duration, and spontaneous recovery. It is caused by a decrease in blood flow to the brain, typically from low blood pressure. There are sometimes symptoms before the loss of consciousness such as lightheadedness, sweating, pale skin, blurred vision, nausea, vomiting, or feeling warm. Syncope may also be associated with a short episode of muscle twitching. Psychiatric causes can also be determined when a patient experiences fear, anxiety, or panic; particularly before a stressful event, usually medical in nature. When consciousness and muscle strength are not completely lost, it is called presyncope. It is recommended that presyncope be treated the same as syncope.

Orthostatic headache is a medical condition in which a person develops a headache while vertical and the headache is relieved when horizontal. Previously it was often misdiagnosed as different primary headache disorders such as migraine or tension headaches. Increasing awareness of the symptom and its causes has prevented delayed or missed diagnosis.

Pacemaker syndrome is a condition that represents the clinical consequences of suboptimal atrioventricular (AV) synchrony or AV dyssynchrony, regardless of the pacing mode, after pacemaker implantation. It is an iatrogenic disease—an adverse effect resulting from medical treatment—that is often underdiagnosed. In general, the symptoms of the syndrome are a combination of decreased cardiac output, loss of atrial contribution to ventricular filling, loss of total peripheral resistance response, and nonphysiologic pressure waves.
Orthostatic syncope refers to syncope resulting from a postural decrease in blood pressure, termed orthostatic hypotension.
Orthostatic hypertension is a medical condition consisting of a sudden and abrupt increase in blood pressure (BP) when a person stands up. Orthostatic hypertension is diagnosed by a rise in systolic BP of 20 mmHg or more when standing. Orthostatic diastolic hypertension is a condition in which the diastolic BP raises to 98 mmHg or over in response to standing, but this definition currently lacks clear medical consensus, so is subject to change. Orthostatic hypertension involving the systolic BP is known as systolic orthostatic hypertension.

Autoimmune autonomic ganglionopathy is a type of immune-mediated autonomic failure that is associated with antibodies against the ganglionic nicotinic acetylcholine receptor present in sympathetic, parasympathetic, and enteric ganglia. Typical symptoms include gastrointestinal dysmotility, orthostatic hypotension, and tonic pupils. Many cases have a sudden onset, but others worsen over time, resembling degenerative forms of autonomic dysfunction. For milder cases, supportive treatment is used to manage symptoms. Plasma exchange, intravenous immunoglobulin, corticosteroids, or immunosuppression have been used successfully to treat more severe cases.
Blair P. Grubb is an American physician, surgeon, researcher and scientist, currently a distinguished university professor of medicine and pediatrics at the University of Toledo. He is well known for his contributions to the study of syncope and disorders of the autonomic nervous system (3).