Orthostatic hypotension, also known as postural hypotension, is a medical condition wherein a person's blood pressure drops when standing up or sitting down. Primary orthostatic hypotension is also often referred to as neurogenic orthostatic hypotension. The drop in blood pressure may be sudden, within 3 minutes or gradual. It is defined as a fall in systolic blood pressure of at least 20 mmHg or diastolic blood pressure of at least 10 mmHg after 3 minutes of standing. It occurs predominantly by delayed constriction of the lower body blood vessels, which is normally required to maintain adequate blood pressure when changing the position to standing. As a result, blood pools in the blood vessels of the legs for a longer period, and less is returned to the heart, thereby leading to a reduced cardiac output and inadequate blood flow to the brain.

Myalgia is the medical term for muscle pain. Myalgia is a symptom of many diseases. The most common cause of acute myalgia is the overuse of a muscle or group of muscles; another likely cause is viral infection, especially when there has been no trauma.

Ehlers–Danlos syndromes (EDS) are a group of 13 genetic connective-tissue disorders. Symptoms often include loose joints, joint pain, stretchy velvety skin, and abnormal scar formation. These may be noticed at birth or in early childhood. Complications may include aortic dissection, joint dislocations, scoliosis, chronic pain, or early osteoarthritis. The current classification was last updated in 2017, when a number of rarer forms of EDS were added.

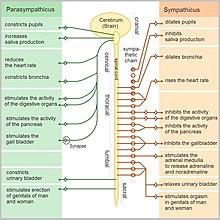
Autonomic neuropathy is a form of polyneuropathy that affects the non-voluntary, non-sensory nervous system, affecting mostly the internal organs such as the bladder muscles, the cardiovascular system, the digestive tract, and the genital organs. These nerves are not under a person's conscious control and function automatically. Autonomic nerve fibers form large collections in the thorax, abdomen, and pelvis outside the spinal cord. They have connections with the spinal cord and ultimately the brain, however. Most commonly autonomic neuropathy is seen in persons with long-standing diabetes mellitus type 1 and 2. In most—but not all—cases, autonomic neuropathy occurs alongside other forms of neuropathy, such as sensory neuropathy.

Dizziness is an imprecise term that can refer to a sense of disorientation in space, vertigo, or lightheadedness. It can also refer to disequilibrium or a non-specific feeling, such as giddiness or foolishness.

Multiple system atrophy (MSA) is a rare neurodegenerative disorder characterized by tremors, slow movement, muscle rigidity, and postural instability, autonomic dysfunction and ataxia. This is caused by progressive degeneration of neurons in several parts of the brain including the basal ganglia, inferior olivary nucleus, and cerebellum.
Familial dysautonomia (FD), also known as Riley-Day syndrome, is a rare, progressive, recessive genetic disorder of the autonomic nervous system that affects the development and survival of sensory, sympathetic, and some parasympathetic neurons in the autonomic and sensory nervous system.
Orthostatic intolerance (OI) is the development of symptoms when standing upright that are relieved when reclining. There are many types of orthostatic intolerance. OI can be a subcategory of dysautonomia, a disorder of the autonomic nervous system occurring when an individual stands up. Some animal species with orthostatic hypotension have evolved to cope with orthostatic disturbances.

Postural orthostatic tachycardia syndrome (POTS) is a condition characterized by an abnormally large increase in heart rate upon sitting up or standing. POTS is a disorder of the autonomic nervous system that can lead the individual to experience a variety of symptoms. Symptoms may include lightheadedness, brain fog, blurred vision, weakness, fatigue, headaches, heart palpitations, exercise intolerance, nausea, diminished concentration, tremulousness (shaking), syncope (fainting), coldness or pain in the extremities, chest pain and shortness of breath. Other conditions associated with POTS include migraine headaches, Ehlers–Danlos syndrome, asthma, autoimmune disease, vasovagal syncope and mast cell activation syndrome. POTS symptoms may be treated with lifestyle changes such as increasing fluid, electrolyte, and salt intake, wearing compression stockings, gentler and slow postural changes, avoiding prolonged bedrest, medication, and physical therapy.

Pure autonomic failure (PAF) is an uncommon, sporadic neurodegenerative condition marked by a steadily declining autonomic regulation. Bradbury and Eggleston originally described pure autonomic failure in 1925.

Inappropriate sinus tachycardia (IST) is defined as sinus tachycardia that is not caused by identifiable medical ailments, a physiological reaction, or pharmaceuticals (a diagnosis of exclusion) and is accompanied by symptoms, frequently invalidating and affecting quality of life. IST symptoms include palpitations, chest discomfort, exhaustion, shortness of breath, presyncope, and syncope.
Da Costa's syndrome, also known as soldier's heart among other names, was a syndrome or a set of symptoms similar to those of heart disease. These include fatigue upon exertion, shortness of breath, palpitations, sweating, chest pain, and sometimes orthostatic intolerance. It was originally thought to be a cardiac condition, and treated with a predecessor to modern cardiac drugs. In modern times, it is believed to represent several unrelated disorders, some of which have a known medical basis.
Small fiber peripheral neuropathy is a type of peripheral neuropathy that occurs from damage to the small unmyelinated and myelinated peripheral nerve fibers. These fibers, categorized as C fibers and small Aδ fibers, are present in skin, peripheral nerves, and organs. The role of these nerves is to innervate some skin sensations and help control autonomic function. It is estimated that 15–20 million people in the United States have some form of peripheral neuropathy.

A neurological disorder is any disorder of the nervous system. Structural, biochemical or electrical abnormalities in the brain, spinal cord or other nerves can result in a range of symptoms. Examples of symptoms include paralysis, muscle weakness, poor coordination, loss of sensation, seizures, confusion, pain, tauopathies, and altered levels of consciousness. There are many recognized neurological disorders, some are relatively common, but many are rare.

Orthostatic headache is a medical condition in which a person develops a headache while vertical and the headache is relieved when horizontal. Previously it was often misdiagnosed as different primary headache disorders such as migraine or tension headaches. Increasing awareness of the symptom and its causes has prevented delayed or missed diagnosis.

Dopamine beta (β)-hydroxylase deficiency is a human medical condition involving inadequate dopamine beta-hydroxylase. It is characterized by increased amounts of serum dopamine and the absence of norepinephrine (NE) and epinephrine.
Orthostatic syncope refers to syncope resulting from a postural decrease in blood pressure, termed orthostatic hypotension.

Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a debilitating long-term medical condition. People with ME/CFS experience delayed worsening of the illness after minor physical or mental activity, which is the hallmark symptom of the illness. Other core symptoms are a greatly reduced ability to do tasks that were previously routine, severe fatigue that does not improve much with rest, and sleep disturbances. Further common symptoms include dizziness or nausea when sitting or standing, along with memory and concentration issues and pain.
Heat intolerance is a symptom characterized by feeling overheated in warm environments or when the surrounding environment's temperature rises. Typically, the person feels uncomfortably hot and sweats excessively.

Autoimmune autonomic ganglionopathy is a type of immune-mediated autonomic failure that is associated with antibodies against the ganglionic nicotinic acetylcholine receptor present in sympathetic, parasympathetic, and enteric ganglia. Typical symptoms include gastrointestinal dysmotility, orthostatic hypotension, and tonic pupils. Many cases have a sudden onset, but others worsen over time, resembling degenerative forms of autonomic dysfunction. For milder cases, supportive treatment is used to manage symptoms. Plasma exchange, intravenous immunoglobulin, corticosteroids, or immunosuppression have been used successfully to treat more severe cases.