Overview
In most countries, immunohematology and transfusion medicine specialists provide expert opinion on massive transfusions, difficult/incompatible transfusions and rational use of specialised blood product therapy like irradiated blood/leukodepleted/washed blood products.
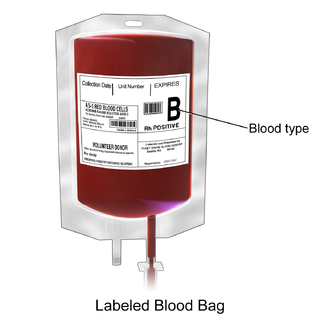
The blood donor center is the facility that collects blood components from screened blood donors, either whole blood or separate components such as plasma or platelets only via apheresis. These blood components are then transported to a central location for processing such as fractionation, testing and redistribution. The testing includes determining blood type and testing for infectious diseases. Whole blood is fractionated into red blood cells, platelets and plasma whilst plasma can be further refined into separate components such as albumin, clotting factor concentrates and immunoglobulin.
The blood bank is the section of the clinical laboratory where laboratory scientists store and distribute blood components. Both areas are typically overseen by a specialist in transfusion medicine. Transfusion medicine was earlier a branch of clinical pathology, however the field has now expanded into a clinical, hospital-based specialty. The practice of transfusion medicine involves both laboratory and clinical aspects of transfusion as communication between blood bank and patients, treating specialists and other medical staff is vital in situations such as massive transfusions or transfusion reactions.
To ensure the safety of blood components, regimented procedures and quality assurance systems must be in place covering all aspects of the transfusion chain, from donation to transfusion outcomes. Within hospitals, transfusion committees are established to ensure safe hospital transfusion practice such as compliance with standards and guidelines, reviewing transfusion reactions and management of blood supply. These multidisciplinary committees are composed of transfusion medicine specialists, transfusion nurses, laboratory scientists, clinicians and staff from hospital management and the quality team.
National differences and how to specialise
Australia
In Australia, transfusion medicine is a sub-specialty of haematology. Training in transfusion medicine is covered by the Royal College of Pathologists of Australasia (RCPA).
Australia has national blood services operated by the Australian Red Cross Blood Service. There are a series of guidelines and standards relevant to the laboratory released by the National Association of Testing Authorities, Australia (NATA), [2] Australian and New Zealand Society of Blood Transfusion (ANZSBT) [3] and RCPA. [4] Similarly, there are a series of clinical practice, patient blood management guidelines by the National Blood Authority.
In Australia, the Serious Transfusion Incident Reporting (STIR) system is in place to capture serious transfusion incidents and near-miss incidents. [5]
- Denmark
In Denmark, the subject is covered by the specialty, "Clinical Immunology".
- Germany
In Germany, transfusion medicine is an independent specialty. Physicians complete a three-year residency in transfusion medicine and two years in another relevant clinical settings like internal medicine or surgery.
- India
In India, Immunohematology and Transfusion Medicine is a medical post graduate specialty (MD) recognized by Medical Council of India since 2009.
- Malaysia
Physicians completing their internship may pursue a four-year Master of Medicine (Transfusion Medicine) programme to specialize in transfusion medicine in Malaysia. [6] They are eligible for registration with National Specialist Registry as transfusion medicine specialists after completion of gazettement upon graduation. [7] Transfusion medicine specialists in Malaysia may further their sub-specialty training in the field of immunohaematology, cord blood, patient blood management, cellular therapy, and regenerative medicine.
- Norway
In Norway, the subject is covered by the specialty, "Immunology and Transfusion medicine"
- United Kingdom
In the United Kingdom, transfusion medicine is a sub-speciality of hematology.
Serious Hazards of Transfusion (SHOT) collects and analyses reports of adverse events related to transfusion, aiming to improve patient safety. [8] Its reports have led to wider training for medical staff in the UK and a central reporting scheme to allow errors to be reported. [9]
There is the Better Blood Continuing Education Programme, which is organised by the EUB which is part of the SNBTS. The EUB consists of many specialist healthcare professionals. The programme's aim is to improve transfusion medicine practise. The programme is reviewed each annually in January. [10]
In the UK, there are restrictions in place to decrease the risk of the transmission of Creutzfeldt–Jakob disease.
- United States
Physicians from a wide range of backgrounds, including pathology, internal medicine, anesthesiology and pediatrics, are eligible for board certification in Transfusion Medicine following a 1–2 year fellowship. It is a board-certified sub-specialty recognized by the American Board of Pathology. [11] These specialists are often considered consultants for physicians who require expert advice on the subjects listed above. Transfusiology is not a recognized term in the US.

Blood transfusion is the process of transferring blood products into a person's circulation intravenously. Transfusions are used for various medical conditions to replace lost components of the blood. Early transfusions used whole blood, but modern medical practice commonly uses only components of the blood, such as red blood cells, white blood cells, plasma, platelets, and other clotting factors.
A blood bank is a center where blood gathered as a result of blood donation is stored and preserved for later use in blood transfusion. The term "blood bank" typically refers to a department of a hospital usually within a clinical pathology laboratory where the storage of blood product occurs and where pre-transfusion and blood compatibility testing is performed. However, it sometimes refers to a collection center, and some hospitals also perform collection. Blood banking includes tasks related to blood collection, processing, testing, separation, and storage.

AABB is an international, not-for-profit organization representing individuals and institutions involved in the field of transfusion medicine and biotherapies.

Plateletpheresis is the process of collecting thrombocytes, more commonly called platelets, a component of blood involved in blood clotting. The term specifically refers to the method of collecting the platelets, which is performed by a device used in blood donation that separates the platelets and returns other portions of the blood to the donor. Platelet transfusion can be a life-saving procedure in preventing or treating serious complications from bleeding and hemorrhage in patients who have disorders manifesting as thrombocytopenia or platelet dysfunction. This process may also be used therapeutically to treat disorders resulting in extraordinarily high platelet counts such as essential thrombocytosis.
Clinical pathology is a medical specialty that is concerned with the diagnosis of disease based on the laboratory analysis of bodily fluids, such as blood, urine, and tissue homogenates or extracts using the tools of chemistry, microbiology, hematology, molecular pathology, and Immunohaematology. This specialty requires a medical residency.

A medical laboratory scientist (MLS) or clinical laboratory scientist (CLS) or medical technologist (MT) performs diagnostic testing of blood and body fluids in clinical laboratories. The scope of a medical laboratory scientist's work begins with the receipt of patient or client specimens and terminates with the delivery of test results to physicians and other healthcare providers. The utility of clinical diagnostic testing relies squarely on the validity of test methodology. To this end, much of the work done by medical laboratory scientists involves ensuring specimen quality, interpreting test results, data-logging, testing control products, performing calibration, maintenance, validation, and troubleshooting of instrumentation as well as performing statistical analyses to verify the accuracy and repeatability of testing. Medical laboratory scientists may also assist healthcare providers with test selection and specimen collection and are responsible for prompt verbal delivery of critical lab results. Medical Laboratory Scientists in healthcare settings also play an important role in clinical diagnosis. An estimated 70% of medical decisions are based on laboratory test results and MLS contributions affect 95% of a health system's costs.

Platelet transfusion, also known as platelet concentrate, is used to prevent or treat bleeding in people with either a low platelet count or poor platelet function. Often this occurs in people receiving cancer chemotherapy. Preventive transfusion is often done in those with platelet levels of less than 10 x 109/L. In those who are bleeding transfusion is usually carried out at less than 50 x 109/L. Blood group matching (ABO, RhD) is typically recommended before platelets are given. Unmatched platelets, however, are often used due to the unavailability of matched platelets. They are given by injection into a vein.
Philip Levine was an immuno-hematologist whose clinical research advanced knowledge on the Rhesus factor, Hemolytic disease of the newborn (HDN) and blood transfusion.

The Health Sciences Authority (HSA) is a statutory board under the Ministry of Health of the Government of Singapore. It is a multi-disciplinary agency responsible for applying medical, pharmaceutical, and scientific expertise to protect and advance public health and safety.

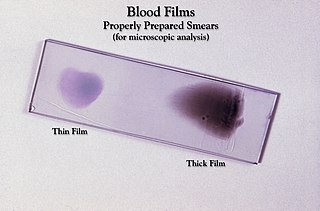
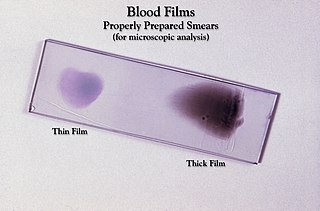
Immunohematology is a branch of hematology and transfusion medicine which studies antigen-antibody reactions and analogous phenomena as they relate to the pathogenesis and clinical manifestations of blood disorders. A person employed in this field is referred to as an immunohematologist. Their day-to-day duties include blood typing, cross-matching and antibody identification.
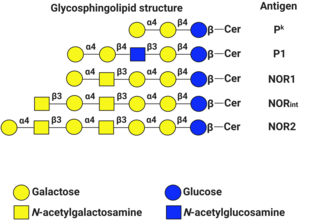
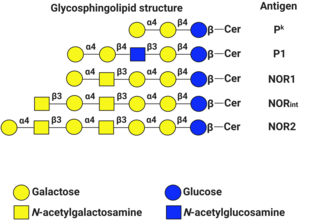
P1PK is a human blood group system based upon the A4GALT gene on chromosome 22. The P antigen was first described by Karl Landsteiner and Philip Levine in 1927. The P1PK blood group system consists of three glycosphingolipid antigens: Pk, P1 and NOR. In addition to glycosphingolipids, terminal Galα1→4Galβ structures are present on complex-type N-glycans. The GLOB antigen is now the member of the separate GLOB blood group system.
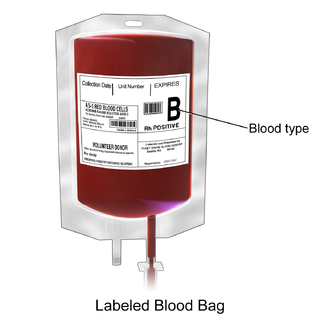
Packed red blood cells, also known as packed cells, are red blood cells that have been separated for blood transfusion. The packed cells are typically used in anemia that is either causing symptoms or when the hemoglobin is less than usually 70–80 g/L. In adults, one unit brings up hemoglobin levels by about 10 g/L. Repeated transfusions may be required in people receiving cancer chemotherapy or who have hemoglobin disorders. Cross-matching is typically required before the blood is given. It is given by injection into a vein.

A medical laboratory or clinical laboratory is a laboratory where tests are conducted out on clinical specimens to obtain information about the health of a patient to aid in diagnosis, treatment, and prevention of disease. Clinical medical laboratories are an example of applied science, as opposed to research laboratories that focus on basic science, such as found in some academic institutions.
Gulf Coast Regional Blood Center is the only blood provider in Houston and its surrounding communities 24 hours a day, 7 days a week. It is one of the largest independent community blood centers in the United States serving 26 counties from the Texas Gulf Coast to Brazos Valley to East Texas. The nonprofit supplies blood to more than 170 hospitals and health care institutions including the Texas Medical Center, the largest medical center in the world. Gulf Coast Regional Blood Center is a proud member of the American Association of Blood Banks (AABB), Blood Centers of America, South Central Association of Blood Banks, Texas Medical Center and America's Blood Centers. Operations started on January 1, 1975, with 64 employees. Today, Gulf Coast Regional Blood Center has over 650 staff members. The overall supervision of Gulf Coast Regional Blood Center's activities is the responsibility of a chief executive officer appointed by the board of trustees. Medical supervision and direction for Gulf Coast Regional Blood Center are provided by a Chief Medical Officer also appointed by the board of trustees.
Patient Blood Management (PBM) is a set of medical practices designed to optimise the care of patients who might need a blood transfusion. Patient blood management programs use an organized framework to improve blood health, thus increasing patient safety and quality of life, reducing costs, and improving clinical outcomes. Some strategies to accomplish this include ensuring that anemia is treated prior to a surgical operation, using surgical techniques that limit blood loss, and returning blood lost during surgery to the patient via intraoperative blood salvage.
Mark Elliot Brecher is a physician specializing in pathology, in particular blood transfusion.
George William Gregory Bird was a British medical doctor, academic, researcher and haematologist known for his expertise in the fields of blood transfusion and immunohaematology. He founded the Department of Transfusion Medicine at the Armed Forces Medical College, Pune and was inducted into their Hall of Fame in 2010. A winner of the Karl Landsteiner Memorial Prize and Morten Grove Rasmussen Memorial Award of the American Association of Blood Banks, Gregory Bird was honoured by the Government of India in 1963, with the award of Padma Shri, the fourth highest Indian civilian award for his services to the nation.
There are more than 100 different titles that are used as another name to Transfusion Practitioner (TP). The most common titles used include Transfusion Practitioner, Haemovigilance Officer, Transfusion Safety Officer, Transfusion Nurse, Patient Blood Management (PBM) Practitioner, and PBM Nurse.

Willy Albert Flegel is a German-American medical researcher, geneticist, and physician who is best known for his work in the field of the Rh blood group. Flegel is the chief of the laboratory services section of the Department of Transfusion Medicine at the National Institutes of Health Clinical Center (NIH).
Dana Devine is a blood transfusion researcher and the president of AABB. She was the editor-in-chief of Vox Sanguinis from 2012 to 2020. Devine is also the Chief Scientist at Canadian Blood Services and the director of the Centre for Blood Research at the University of British Columbia. In 2015, she was elected as a fellow of the Canadian Academy of Health Sciences. In 2022, she was elected as the President of the Biomedical Excellence for Safer Transfusion Collaborative.