Chemotherapy is a type of cancer treatment that uses one or more anti-cancer drugs as part of a standardized chemotherapy regimen. Chemotherapy may be given with a curative intent or it may aim to prolong life or to reduce symptoms. Chemotherapy is one of the major categories of the medical discipline specifically devoted to pharmacotherapy for cancer, which is called medical oncology.
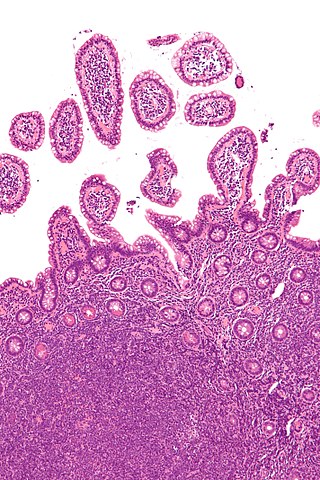
Non-Hodgkin lymphoma (NHL), also known as non-Hodgkin's lymphoma, is a group of blood cancers that includes all types of lymphomas except Hodgkin lymphomas. Symptoms include enlarged lymph nodes, fever, night sweats, weight loss, and tiredness. Other symptoms may include bone pain, chest pain, or itchiness. Some forms are slow-growing while others are fast-growing.

Lymphoma is a group of blood and lymph tumors that develop from lymphocytes. The name typically refers to just the cancerous versions rather than all such tumours. Signs and symptoms may include enlarged lymph nodes, fever, drenching sweats, unintended weight loss, itching, and constantly feeling tired. The enlarged lymph nodes are usually painless. The sweats are most common at night.

A myelodysplastic syndrome (MDS) is one of a group of cancers in which immature blood cells in the bone marrow do not mature, and as a result, do not develop into healthy blood cells. Early on, no symptoms typically are seen. Later, symptoms may include fatigue, shortness of breath, bleeding disorders, anemia, or frequent infections. Some types may develop into acute myeloid leukemia.

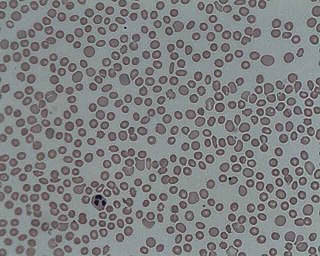
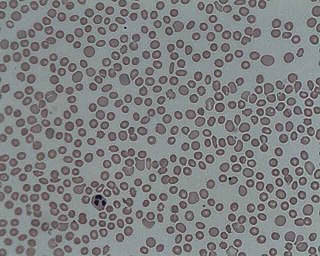
Thalassemias are inherited blood disorders that result in abnormal hemoglobin. Symptoms depend on the type of thalassemia and can vary from none to severe. Often there is mild to severe anemia as thalassemia can affect the production of red blood cells and also affect how long the red blood cells live. Symptoms of anemia include feeling tired and having pale skin. Other symptoms of thalassemia include bone problems, an enlarged spleen, yellowish skin, pulmonary hypertension, and dark urine. Slow growth may occur in children. Symptoms and presentations of thalassemia can change over time.

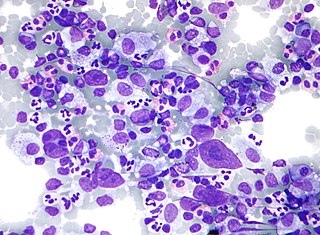
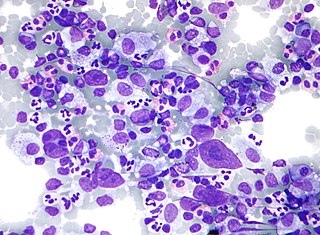
Multiple myeloma (MM), also known as plasma cell myeloma and simply myeloma, is a cancer of plasma cells, a type of white blood cell that normally produces antibodies. Often, no symptoms are noticed initially. As it progresses, bone pain, anemia, kidney dysfunction, and infections may occur. Complications may include hypercalcemia and amyloidosis.
In hematology, thrombocytopenia is a condition characterized by abnormally low levels of platelets in the blood. Low levels of platelets in turn may lead to prolonged or excessive bleeding. It is the most common coagulation disorder among intensive care patients and is seen in a fifth of medical patients and a third of surgical patients.
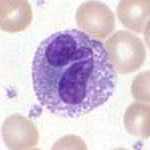
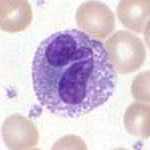
Granulocytes are cells in the innate immune system characterized by the presence of specific granules in their cytoplasm. Such granules distinguish them from the various agranulocytes. All myeloblastic granulocytes are polymorphonuclear, that is, they have varying shapes (morphology) of the nucleus ; and are referred to as polymorphonuclear leukocytes. In common terms, polymorphonuclear granulocyte refers specifically to "neutrophil granulocytes", the most abundant of the granulocytes; the other types have varying morphology. Granulocytes are produced via granulopoiesis in the bone marrow.

Acute lymphoblastic leukemia (ALL) is a cancer of the lymphoid line of blood cells characterized by the development of large numbers of immature lymphocytes. Symptoms may include feeling tired, pale skin color, fever, easy bleeding or bruising, enlarged lymph nodes, or bone pain. As an acute leukemia, ALL progresses rapidly and is typically fatal within weeks or months if left untreated.

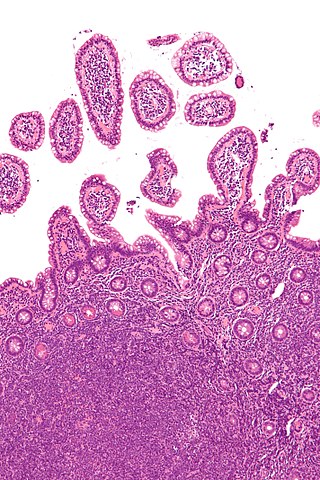
Gastrointestinal bleeding, also called gastrointestinal hemorrhage (GIB), is all forms of bleeding in the gastrointestinal tract, from the mouth to the rectum. When there is significant blood loss over a short time, symptoms may include vomiting red blood, vomiting black blood, bloody stool, or black stool. Small amounts of bleeding over a long time may cause iron-deficiency anemia resulting in feeling tired or heart-related chest pain. Other symptoms may include abdominal pain, shortness of breath, pale skin, or passing out. Sometimes in those with small amounts of bleeding no symptoms may be present.

Plateletpheresis is the process of collecting thrombocytes, more commonly called platelets, a component of blood involved in blood clotting. The term specifically refers to the method of collecting the platelets, which is performed by a device used in blood donation that separates the platelets and returns other portions of the blood to the donor. Platelet transfusion can be a life-saving procedure in preventing or treating serious complications from bleeding and hemorrhage in patients who have disorders manifesting as thrombocytopenia or platelet dysfunction. This process may also be used therapeutically to treat disorders resulting in extraordinarily high platelet counts such as essential thrombocytosis.

Tranexamic acid (TXA) is a medication used to treat or prevent excessive blood loss from major trauma, postpartum bleeding, surgery, tooth removal, nosebleeds, and heavy menstruation. It is also used for hereditary angioedema. It is taken either orally or by injection into a vein.

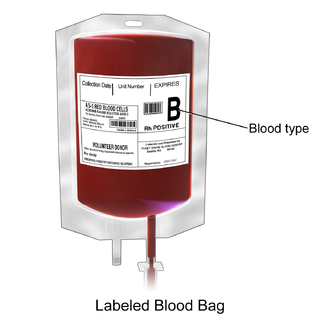
Fresh frozen plasma (FFP) is a blood product made from the liquid portion of whole blood. It is used to treat conditions in which there are low blood clotting factors or low levels of other blood proteins. It may also be used as the replacement fluid in plasma exchange. Using ABO compatible plasma, while not required, may be recommended. Use as a volume expander is not recommended. It is administered by slow injection into a vein.
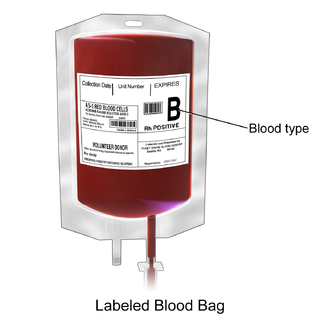
Packed red blood cells, also known as packed cells, are red blood cells that have been separated for blood transfusion. The packed cells are typically used in anemia that is either causing symptoms or when the hemoglobin is less than usually 70–80 g/L. In adults, one unit brings up hemoglobin levels by about 10 g/L. Repeated transfusions may be required in people receiving cancer chemotherapy or who have hemoglobin disorders. Cross-matching is typically required before the blood is given. It is given by injection into a vein.
Platelet transfusion refractoriness is the repeated failure to achieve the desired level of blood platelets in a patient following a platelet transfusion. The cause of refractoriness may be either immune or non-immune. Among immune-related refractoriness, antibodies against HLA antigens are the primary cause. Non-immune causes include splenomegaly, fever, and sepsis.
Patient Blood Management (PBM) is a set of medical practices designed to optimise the care of patients who might need a blood transfusion. Patient blood management programs use an organized framework to improve blood health, thus increasing patient safety and quality of life, reducing costs, and improving clinical outcomes. Some strategies to accomplish this include ensuring that anemia is treated prior to a surgical operation, using surgical techniques that limit blood loss, and returning blood lost during surgery to the patient via intraoperative blood salvage.
Hodgkin lymphoma (HL) is a type of lymphoma in which cancer originates from a specific type of white blood cell called lymphocytes, where multinucleated Reed–Sternberg cells are present in the patient's lymph nodes. The condition was named after the English physician Thomas Hodgkin, who first described it in 1832. Symptoms may include fever, night sweats, and weight loss. Often, nonpainful enlarged lymph nodes occur in the neck, under the arm, or in the groin. Persons affected may feel tired or be itchy.
Red blood cells (erythrocytes) from donors contain normal hemoglobin (HbA), and transfusion of normal red blood cells into people with sickle cell disease reduces the percentage of red cells in the circulation containing the abnormal hemoglobin (HbS). Although transfusion of donor red blood cells can ameliorate and even prevent complications of sickle cell disease in certain circumstances, transfusion therapy is not universally beneficial in sickle cell disease.
Neonates are defined as babies up to 28 days after birth. Most extremely preterm babies require at least one red cell transfusion; this is partly due to the amount of blood removed with blood samples compared to the baby's total blood volume and partly due to anemia of prematurity. Most transfusions are given as small volume top-up transfusions to increase the baby's hemoglobin above a certain pre-defined level, or because the baby is unwell due to the anemia. Possible side-effects of anemia in babies can be poor growth, lethargy and episodes of apnea. Exchange blood transfusion is used to treat a rapidly rising bilirubin that does not respond to treatment with phototherapy or intravenous immunoglobulin. This is usually due to hemolytic disease of the newborn, but may also be due to other causes, e.g., G6PD deficiency.
A granulocyte transfusion is a medical procedure in which granulocytes are infused into a person's blood. Granulocyte transfusions were historically used to prevent and treat infections in people with neutropenia, but the practice declined in popularity in the 1980s. Interest in the procedure increased in the 1990s due to the development of more effective methods for harvesting granulocytes and a growing population of people with severe neutropenia from chemotherapy. However, the treatment's efficacy remains poorly understood and its use is controversial.