A blood type is a classification of blood, based on the presence and absence of antibodies and inherited antigenic substances on the surface of red blood cells (RBCs). These antigens may be proteins, carbohydrates, glycoproteins, or glycolipids, depending on the blood group system. Some of these antigens are also present on the surface of other types of cells of various tissues. Several of these red blood cell surface antigens can stem from one allele and collectively form a blood group system.
Rh disease is a type of hemolytic disease of the fetus and newborn (HDFN). HDFN due to anti-D antibodies is the proper and currently used name for this disease as the Rh blood group system actually has more than 50 antigens and not only D-antigen. The term "Rh Disease" is commonly used to refer to HDFN due to anti-D antibodies, and prior to the discovery of anti-Rho(D) immune globulin, it was the most common type of HDFN. The disease ranges from mild to severe, and occurs in the second or subsequent pregnancies of Rh-D negative women when the biologic father is Rh-D positive.
Glycophorin C plays a functionally important role in maintaining erythrocyte shape and regulating membrane material properties, possibly through its interaction with protein 4.1. Moreover, it has previously been shown that membranes deficient in protein 4.1 exhibit decreased content of glycophorin C. It is also an integral membrane protein of the erythrocyte and acts as the receptor for the Plasmodium falciparum protein PfEBP-2.
A Coombs test, also known as antiglobulin test (AGT) is either of two blood tests used in immunohematology. They are the direct and indirect Coombs tests. The direct Coombs test detects antibodies that are stuck to the surface of the red blood cells. Since these antibodies sometimes destroy red blood cells, a person can be anemic and this test can help clarify the condition. The indirect Coombs detects antibodies that are floating freely in the blood. These antibodies could act against certain red blood cells and the test can be done to diagnose reactions to a blood transfusion.

The ABO blood group system is used to denote the presence of one, both, or neither of the A and B antigens on erythrocytes. In human blood transfusions it is the most important of the 38 different blood type classification systems currently recognized. A mismatch in this, or any other serotype, can cause a potentially fatal adverse reaction after a transfusion, or an unwanted immune response to an organ transplant. The associated anti-A and anti-B antibodies are usually IgM antibodies, produced in the first years of life by sensitization to environmental substances such as food, bacteria, and viruses.
In ABO hemolytic disease of the newborn maternal IgG antibodies with specificity for the ABO blood group system pass through the placenta to the fetal circulation where they can cause hemolysis of fetal red blood cells which can lead to fetal anemia and HDN. In contrast to Rh disease, about half of the cases of ABO HDN occur in a firstborn baby and ABO HDN does not become more severe after further pregnancies.
Hemolytic disease of the newborn (anti-Kell1) is the second most common cause of severe hemolytic disease of the newborn (HDN) after Rh disease. Anti-Kell1 is becoming relatively more important as prevention of Rh disease is also becoming more effective.
The Kell antigen system is a human blood group system, that is, group of antigens on the human red blood cell surface which are important determinants of blood type and are targets for autoimmune or alloimmune diseases which destroy red blood cells. The Kell antigens are K, k, Kpa, Kpb, Jsa and Jsb. The Kell antigens are peptides found within the Kell protein, a 93-kilodalton transmembrane zinc-dependent endopeptidase which is responsible for cleaving endothelin-3.
The Kidd antigen system are proteins found in the Kidd's blood group, which act as antigens, i.e., they have the ability to produce antibodies under certain circumstances. The Jk antigen is found on a protein responsible for urea transport in the red blood cells and the kidney. They are important in transfusion medicine. People with two Jk(a) antigens, for instance, may form antibodies against donated blood containing two Jk(b) antigens. This can lead to hemolytic anemia, in which the body destroys the transfused blood, leading to low red blood cell counts. Another disease associated with the Jk antigen is hemolytic disease of the newborn, in which a pregnant woman's body creates antibodies against the blood of her fetus, leading to destruction of the fetal blood cells. Hemolytic disease of the newborn associated with Jk antibodies is typically mild, though fatal cases have been reported.

The Rh blood group system is a human blood group system. It contains proteins on the surface of red blood cells. After the ABO blood group system, it is the most likely to be involved in transfusion reactions. The Rh blood group system consists of 49 defined blood group antigens, among which the five antigens D, C, c, E, and e are the most important. There is no d antigen. Rh(D) status of an individual is normally described with a positive or negative suffix after the ABO type. The terms Rh factor, Rh positive, and Rh negative refer to the Rh(D) antigen only. Antibodies to Rh antigens can be involved in hemolytic transfusion reactions and antibodies to the Rh(D) and Rh antigens confer significant risk of hemolytic disease of the fetus and newborn.
hh, or the Bombay blood group, is a rare blood type. This blood phenotype was first discovered in Bombay by Dr. Y. M. Bhende in 1952. It is mostly found in the Indian sub-continent and parts of the Middle East such as Iran.
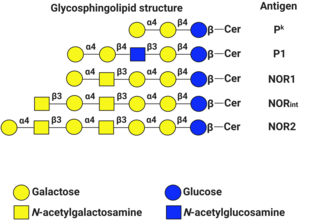
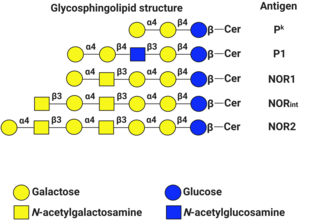
P1PK is a human blood group system based upon the A4GALT gene on chromosome 22. The P antigen was first described by Karl Landsteiner and Philip Levine in 1927. The P1PK blood group system consists of three glycosphingolipid antigens: Pk, P1 and NOR. In addition to glycosphingolipids, terminal Galα1→4Galβ structures are present on complex-type N-glycans. The GLOB antigen is now the member of the separate GLOB blood group system.
The Lewis antigen system is a human blood group system. It is based upon two genes on chromosome 19: FUT3, or Lewis gene; and FUT2, or Secretor gene. Both genes are expressed in glandular epithelia. FUT2 has a dominant allele which codes for an enzyme and a recessive allele which does not produce a functional enzyme. Similarly, FUT3 has a functional dominant allele (Le) and a non-functional recessive allele (le).

The Diego antigen system is composed of 21 blood factors or antigens carried on the Band 3 glycoprotein, also known as Anion Exchanger 1 (AE1). The antigens are inherited through various alleles of the gene SLC4A1, located on human chromosome 17. The AE1 glycoprotein is expressed only in red blood cells and, in a shortened form, in some cells in the kidney. The Diegoa antigen is fairly common in Indigenous peoples of the Americas and East Asians, but very rare or absent in most other populations, supporting the theory that the two groups share common ancestry.

Glycophorin A , also known as GYPA, is a protein which in humans is encoded by the GYPA gene. GYPA has also recently been designated CD235a.

Glycophorin B also known as sialoglycoprotein delta and SS-active sialoglycoprotein is a protein which in humans is encoded by the GYPB gene. GYPB has also recently been designated CD235b.
The Junior blood group system is a human blood group defined by the presence or absence of the Jr(a) antigen, a high-frequency antigen that is found on the red blood cells of most individuals. People with the rare Jr(a) negative blood type can develop anti-Jr(a) antibodies, which may cause transfusion reactions and hemolytic disease of the newborn on subsequent exposures. Jr(a) negative blood is most common in people of Japanese heritage.

Blood compatibility testing is conducted in a medical laboratory to identify potential incompatibilities between blood types in blood transfusion. It is also used to diagnose and prevent some complications of pregnancy that can occur when the baby has a different blood group from the mother. Blood compatibility testing includes blood typing, which detects the antigens on red blood cells that determine a person's blood type; testing for unexpected antibodies against blood group antigens ; and, in the case of blood transfusions, mixing the recipient's plasma with the donor's red blood cells to detect incompatibilities (crossmatching). Routine blood typing involves determining the ABO and RhD type, and involves both identification of ABO antigens on red blood cells and identification of ABO antibodies in the plasma. Other blood group antigens may be tested for in specific clinical situations.
The Lan blood group system is a human blood group defined by the presence or absence of the Lan antigen on a person's red blood cells. More than 99.9% of people are positive for the Lan antigen. Individuals with the rare Lan-negative blood type, which is a recessive trait, can produce an anti-Lan antibody when exposed to Lan-positive blood. Anti-Lan antibodies may cause transfusion reactions on subsequent exposures to Lan-positive blood, and have also been implicated in mild cases of hemolytic disease of the newborn. However, the clinical significance of the antibody is variable. The antigen was first described in 1961, and Lan was officially designated a blood group in 2012.
The Augustine blood group system is a human blood group system. It includes four red blood cell surface glycoprotein antigens which are encoded by alleles of the gene SLC29A1.