Related Research Articles

Acute disseminated encephalomyelitis (ADEM), or acute demyelinating encephalomyelitis, is a rare autoimmune disease marked by a sudden, widespread attack of inflammation in the brain and spinal cord. As well as causing the brain and spinal cord to become inflamed, ADEM also attacks the nerves of the central nervous system and damages their myelin insulation, which, as a result, destroys the white matter. It is often triggered by a viral infection or vaccinations.

Myelin is a lipid-rich material that surrounds nerve cell axons to insulate them and increase the rate at which electrical impulses are passed along the axon. The myelinated axon can be likened to an electrical wire with insulating material (myelin) around it. However, unlike the plastic covering on an electrical wire, myelin does not form a single long sheath over the entire length of the axon. Rather, myelin sheaths the nerve in segments: in general, each axon is encased with multiple long myelinated sections with short gaps in between called nodes of Ranvier.
Optic neuritis describes any condition that causes inflammation of the optic nerve; it may be associated with demyelinating diseases, or infectious or inflammatory processes.
Multiplesclerosis (MS) is the most common demyelinating disease, in which the insulating covers of nerve cells in the brain and spinal cord are damaged. This damage disrupts the ability of parts of the nervous system to transmit signals, resulting in a range of signs and symptoms, including physical, mental, and sometimes psychiatric problems. Specific symptoms can include double vision, blindness in one eye, muscle weakness, and trouble with sensation or coordination. MS takes several forms, with new symptoms either occurring in isolated attacks or building up over time. In the relapsing forms of MS, between attacks, symptoms may disappear completely, although some permanent neurological problems often remain, especially as the disease advances.
A demyelinating disease is any disease of the nervous system in which the myelin sheath of neurons is damaged. This damage impairs the conduction of signals in the affected nerves. In turn, the reduction in conduction ability causes deficiency in sensation, movement, cognition, or other functions depending on which nerves are involved.
Neuromyelitis optica spectrum disorders (NMOSD), including neuromyelitis optica (NMO), are autoimmune diseases characterized by acute inflammation of the optic nerve and the spinal cord (myelitis). Episodes of ON and myelitis can be simultaneous or successive. A relapsing disease course is common, especially in untreated patients. In more than 80% of cases, NMO is caused by immunoglobulin G autoantibodies to aquaporin 4 (anti-AQP4), the most abundant water channel protein in the central nervous system. A subset of anti-AQP4-negative cases is associated with antibodies against myelin oligodendrocyte glycoprotein (anti-MOG). Rarely, NMO may occur in the context of other autoimmune diseases or infectious diseases. In some cases, the etiology remains unknown.
Interferon beta-1b is a cytokine in the interferon family used to treat the relapsing-remitting and secondary-progressive forms of multiple sclerosis (MS). It is approved for use after the first MS event. Closely related is interferon beta 1a, also indicated for MS, with a very similar drug profile.

Neuritis is inflammation of a nerve or the general inflammation of the peripheral nervous system. Inflammation, and frequently concomitant demyelination, cause impaired transmission of neural signals and leads to aberrant nerve function. Neuritis is often conflated with neuropathy, a broad term describing any disease process which affects the peripheral nervous system. However, neuropathies may be due to either inflammatory or non-inflammatory causes, and the term encompasses any form of damage, degeneration, or dysfunction, while neuritis refers specifically to the inflammatory process.
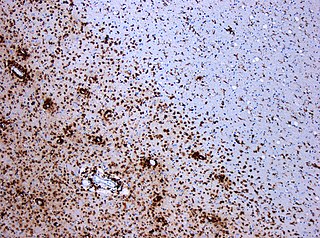
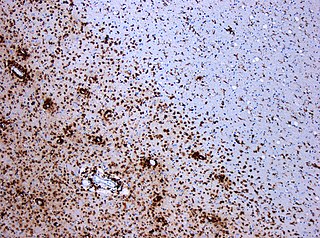
Multiple sclerosis and other demyelinating diseases of the central nervous system (CNS) produce lesions and glial scars or scleroses. They present different shapes and histological findings according to the underlying condition that produces them.
Remyelination is the process of propagating oligodendrocyte precursor cells to form oligodendrocytes to create new myelin sheaths on demyelinated axons in the CNS. This is a process naturally regulated in the body and tends to be very efficient in a healthy CNS. The process creates a thinner myelin sheath than normal, but it helps to protect the axon from further damage, from overall degeneration, and proves to increase conductance once again. The processes underlying remyelination are under investigation in the hope of finding treatments for demyelinating diseases, such as multiple sclerosis.
Multiple sclerosis (MS) is a chronic inflammatory demyelinating disease that affects the central nervous system (CNS). Several therapies for it exist, although there is no known cure.
Inflammatory demyelinating diseases (IDDs), sometimes called Idiopathic (IIDDs) due to the unknown etiology of some of them, are a heterogenous group of demyelinating diseases - conditions that cause damage to myelin, the protective sheath of nerve fibers - that occur against the background of an acute or chronic inflammatory process. IDDs share characteristics with and are often grouped together under Multiple Sclerosis. They are sometimes considered different diseases from Multiple Sclerosis, but considered by others to form a spectrum differing only in terms of chronicity, severity, and clinical course.

Multiple sclerosis can cause a variety of symptoms: changes in sensation (hypoesthesia), muscle weakness, abnormal muscle spasms, or difficulty moving; difficulties with coordination and balance; problems in speech (dysarthria) or swallowing (dysphagia), visual problems, fatigue and acute or chronic pain syndromes, bladder and bowel difficulties, cognitive impairment, or emotional symptomatology. The main clinical measure in progression of the disability and severity of the symptoms is the Expanded Disability Status Scale or EDSS.
A clinically isolated syndrome (CIS) is a clinical situation of an individual's first neurological episode, caused by inflammation or demyelination of nerve tissue. An episode may be monofocal, in which symptoms present at a single site in the central nervous system, or multifocal, in which multiple sites exhibit symptoms. CIS with enough paraclinical evidence can be considered as a clinical stage of multiple sclerosis (MS). It can also be retrospectively diagnosed as a kind of MS when more evidence is available.

Tumefactive multiple sclerosis is a condition in which the central nervous system of a person has multiple demyelinating lesions with atypical characteristics for those of standard multiple sclerosis (MS). It is called tumefactive as the lesions are "tumor-like" and they mimic tumors clinically, radiologically and sometimes pathologically.

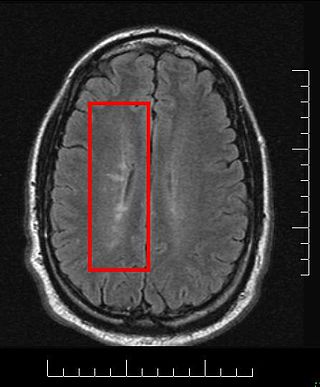
Current standards for diagnosing multiple sclerosis (MS) are based on the 2018 revision of McDonald criteria. They rely on MRI detection of demyelinating lesions in the CNS, which are distributed in space (DIS) and in time (DIT). It is also a requirement that any possible known disease that produces demyelinating lesions is ruled out before applying McDonald's criteria.
MOG antibody disease (MOGAD) or MOG antibody-associated encephalomyelitis (MOG-EM) is an inflammatory demyelinating disease of the central nervous system. Serum anti-myelin oligodendrocyte glycoprotein antibodies are present in up to half of patients with an acquired demyelinating syndrome and have been described in association with a range of phenotypic presentations, including acute disseminated encephalomyelitis, optic neuritis, transverse myelitis, and neuromyelitis optica.
Anti-neurofascin demyelinating diseases refers to health conditions engendered by auto-antibodies against neurofascins, which can produce both central and peripheral demyelination. Some cases of combined central and peripheral demyelination (CCPD) could be produced by them.
Anti-AQP4 diseases, are a group of diseases characterized by auto-antibodies against aquaporin 4.
Uhthoff is a surname. Notable people with the surname include:
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 Panginikkod, Sreelakshmi; Rayi, Appaji; Cabrero, Franklyn Rocha; Rukmangadachar, Lokesh A. (January 2021). "Uhthoff phenomenon". StatPearls. PMID 29261916 – via PubMed.
- 1 2 3 4 5 Flensner, G.; Ek, A.C.; Soderhamn, O.; Landtblom, A.M. (2011). "Sensitivity to heat in MS patients: a factor strongly influencing symptomology-an explorative survey". BMC Neurol. 11: 27. doi:10.1186/1471-2377-11-27. PMC 3056752 . PMID 21352533.
- 1 2 3 4 5 6 7 8 Park, Kwiyoung; Tanaka, Keiko; Tanaka, Masami (2014). "Uhthoff's Phenomenon in Multiple Sclerosis and Neuromyelitis Optica". European Neurology. 72 (3–4): 153–156. doi:10.1159/000361045. ISSN 0014-3022. PMID 25195501. S2CID 46704524 – via Karger Publishers.
- ↑ Thurtell, M. J. (2014). "Visual Loss, Transient". Encyclopedia of the Neurological Sciences (2nd ed.). Academic Press. pp. 698–703. doi:10.1016/B978-0-12-385157-4.00168-8. ISBN 978-0-12-385158-1.
- 1 2 3 Khanh Vu, T.H.; Zhu, R.; Yang, L.; Chen, D. F. (2014). "Optic Nerve Structure and Pathologies". Pathobiology of Human Disease - A Dynamic Encyclopedia of Disease Mechanisms. Academic Press. pp. 2115–2125. doi:10.1016/B978-0-12-386456-7.04707-9. ISBN 978-0-12-386457-4.
- 1 2 Davis SL, Frohman TC, Crandall CG, et al. (March 2008). "Modeling Uhthoff's phenomenon in MS patients with internuclear ophthalmoparesis". Neurology. 70 (13 Pt 2): 1098–106. doi:10.1212/01.wnl.0000291009.69226.4d. PMID 18287569. S2CID 24002003.
- 1 2 Johns, Paul (2014-01-01). "Chapter 14 - Multiple Sclerosis". Clinical Neuroscience. Churchill Livingstone. pp. 181–196. doi:10.1016/B978-0-443-10321-6.00014-X. ISBN 978-0-443-10321-6.
{{cite book}}: CS1 maint: date and year (link) - 1 2 Davis, Scott L.; Jay, Ollie; Wilson, Thad E. (2018). "Thermoregulatory dysfunction in multiple sclerosis". Handbook of Clinical Neurology. Vol. 157. Elsevier. pp. 701–714. doi:10.1016/B978-0-444-64074-1.00042-2. ISBN 9780444640741. ISSN 0072-9752. PMID 30459034.
- 1 2 White, A.T.; Wilson, T.E.; Davis, S.L.; Petajan, J.H. (2000). "Effect of precooling on physical performance in multiple sclerosis". Mult Scler. 6 (3): 176–180. doi:10.1177/135245850000600307. PMID 10871829. S2CID 41165079.
- 1 2 White, L.J.; Dressendorfer, L.H. (2004). "Exercise and multiple sclerosis". Sports Med. 34 (15): 1077–1100. doi:10.2165/00007256-200434150-00005. PMID 15575796. S2CID 27787579.
- ↑ W. Uhthoff: Untersuchungen über die bei der multiplen Herdsklerose vorkommenden Augenstörungen. Archiv für Psychiatrie und Nervenkrankheiten, Berlin, 1890, 21: 55-116 and 303-410.
- ↑ Guthrie, T.C.; Nelson, D.A. (1995). "Influence of temperature changes on multiple sclerosis: critical review of mechanisms and research potential". J Neurol Sci. 129 (1): 1–8. doi:10.1016/0022-510x(94)00248-m. PMID 7751837. S2CID 12555514.