Related Research Articles

Megalencephaly is a growth development disorder in which the brain is abnormally large. It is characterized by a brain with an average weight that is 2.5 standard deviations above the mean of the general population. Approximately 1 out of 50 children (2%) are said to have the characteristics of megalencephaly in the general population.

Macrocephaly is a condition in which circumference of the human head is abnormally large. It may be pathological or harmless, and can be a familial genetic characteristic. People diagnosed with macrocephaly will receive further medical tests to determine whether the syndrome is accompanied by particular disorders. Those with benign or familial macrocephaly are considered to have megalencephaly.

Alexander disease is a very rare autosomal dominant leukodystrophy, which are neurological conditions caused by anomalies in the myelin which protects nerve fibers in the brain. The most common type is the infantile form that usually begins during the first two years of life. Symptoms include mental and physical developmental delays, followed by the loss of developmental milestones, an abnormal increase in head size and seizures. The juvenile form of Alexander disease has an onset between the ages of 2 and 13 years. These children may have excessive vomiting, difficulty swallowing and speaking, poor coordination, and loss of motor control. Adult-onset forms of Alexander disease are less common. The symptoms sometimes mimic those of Parkinson’s disease or multiple sclerosis, or may present primarily as a psychiatric disorder.

CADASIL or CADASIL syndrome, involving cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy, is the most common form of hereditary stroke disorder, and is thought to be caused by mutations of the Notch 3 gene on chromosome 19. The disease belongs to a family of disorders called the leukodystrophies. The most common clinical manifestations are migraine headaches and transient ischemic attacks or strokes, which usually occur between 40 and 50 years of age, although MRI is able to detect signs of the disease years prior to clinical manifestation of disease.

Leukodystrophies are a group of, usually, inherited disorders, characterized by degeneration of the white matter in the brain. The word leukodystrophy comes from the Greek roots leuko, "white", dys, "abnormal" and troph, "growth". The leukodystrophies are caused by imperfect growth or development of the glial cells which produce the myelin sheath, the fatty insulating covering around nerve fibers. Leukodystrophies may be classified as hypomyelinating or demyelinating diseases, respectively, depending on whether the damage is present before birth or occurs after. Other demyelinating diseases are usually not congenital and have a toxic or autoimmune cause.
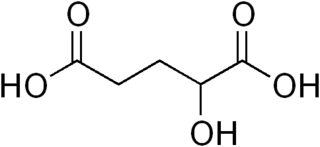
2-hydroxyglutaric aciduria is a rare neurometabolic disorder characterized by the significantly elevated levels of hydroxyglutaric acid in one's urine. It is either autosomal recessive or autosomal dominant.
Leukoencephalopathy is a term that describes all of the brain white matter diseases, whether their molecular cause is known or unknown. It can refer specifically to any of these diseases:

Leukoencephalopathy with vanishing white matter is an autosomal recessive neurological disease. The cause of the disease are mutations in any of the 5 genes encoding subunits of the translation initiation factor eIF2B: EIF2B1, EIF2B2, EIF2B3, EIF2B4, or EIF2B5. The disease belongs to a family of conditions called the Leukodystrophies.

Membrane protein MLC1 is a protein that in humans is encoded by the MLC1 gene.

Translation initiation factor eIF-2B subunit delta is a protein that in humans is encoded by the EIF2B4 gene.

Translation initiation factor eIF-2B subunit gamma is a protein that in humans is encoded by the EIF2B3 gene.
Leukoencephalopathy with neuroaxonal spheroids (LENAS) is an extremely rare kind of leukoencephalopathy and is classified as a neurodegenerative disease. LENAS is a cause of severe and subacute dementia that results from damage to certain areas of the brain. This damage is to a type of brain tissue called white matter and axon damage due to swellings which are termed spheroids.
Ribose-5-phosphate isomerase deficiency is a human disorder caused by mutations in ribose-5-phosphate isomerase, an enzyme of the pentose phosphate pathway. With only four diagnosed patients over a 27-year period, RPI deficiency is the second rarest disease known as of now, being beaten only by Fields Condition affecting three individuals, Catherine and Kirstie Fields and Pavle Milović.

Hereditary diffuse leukoencephalopathy with spheroids (HDLS) is a rare adult onset autosomal dominant disorder characterized by cerebral white matter degeneration with demyelination and axonal spheroids leading to progressive cognitive and motor dysfunction. Spheroids are axonal swellings with discontinuous or absence of myelin sheaths. It is believed that the disease arises from primary microglial dysfunction that leads to secondary disruption of axonal integrity, neuroaxonal damage, and focal axonal spheroids leading to demyelination. Spheroids in HDLS resemble to some extent those produced by shear stress in a closed head injury with damage to axons, causing them to swell due to blockage of axoplasmic transport. In addition to trauma, axonal spheroids can be found in aged brain, stroke, and in other degenerative diseases. In HDLS, it is uncertain whether demyelination occurs prior to the axonal spheroids or what triggers neurodegeneration after apparently normal brain and white matter development, although genetic deficits suggest that demyelination and axonal pathology may be secondary to microglial dysfunction. The clinical syndrome in patients with HDLS is not specific and it can be mistaken for Alzheimer's disease, frontotemporal dementia, atypical Parkinsonism, multiple sclerosis, or corticobasal degeneration.

Cerebroretinal microangiopathy with calcifications and cysts (CRMCC) is a rare genetic disorder, which affects multiple organs. Its hallmarks are widespread progressive calcifications, cysts and abnormalities of the white matter of the brain, usually occurring together with abnormalities of the blood vessels of the retina. Additional features include poor prenatal growth, preterm birth, anemia, osteopenia and bone fractures, and gastrointestinal bleeding. It is caused by compound heterozygous mutations in the conserved telomere maintenance component 1 (CTC1) gene, but its exact pathophysiology is still not well understood.

Cerebral autosomal recessive arteriopathy with subcortical infarcts and leukoencephalopathy (CARASIL) is disease of the arteries in the brain, which causes tissue loss in the subcortical region of the brain and the destruction of myelin in the CNS. CARASIL is characterized by symptoms such as gait disturbances, hair loss, low back pain, dementia, and stroke. CARASIL is a rare disease, having only been diagnosed in about 50 patients, of which ten have been genetically confirmed. Most cases have been reported in Japan, but Chinese and caucasian individuals have also been diagnosed with the disease. CARASIL is inherited in an autosomal recessive pattern. There is currently no cure for CARASIL. Other names for CARASIL include familial young-adult-onset arteriosclerotic leukoencephalopathy with alopecia and lumbago without arterial hypertension, Nemoto disease and Maeda syndrome.

Acyl-CoA oxidase deficiency is a rare disorder that leads to significant damage and deterioration of nervous system functions (neurodegeneration). It is caused by pathogenic variants in ACOX1, which codes for the production of an enzyme called peroxisomal straight-chain acyl-CoA oxidase (ACOX1). This specific enzyme is responsible for the breakdown of very long chain fatty acids (VLCFAs).

Spongy degeneration of the central nervous system, also known as Canavan's disease, Van Bogaert-Bertrand type or Aspartoacylase (AspA) deficiency, is a rare autosomal recessive neurodegenerative disorder. It belongs to a group of genetic disorders known as leukodystrophies, where the growth and maintenance of myelin sheath in the central nervous system (CNS) are impaired. There are three types of spongy degeneration: infantile, congenital and juvenile, with juvenile being the most severe type. Common symptoms in infants include lack of motor skills, weak muscle tone, and macrocephaly. It may also be accompanied by difficulties in feeding and swallowing, seizures and sleep disturbances. Affected children typically die before the age of 10, but life expectancy can vary.

Hypomyelination-congenital cataract syndrome is a rare autosomal recessive hereditary disorder that affects the brain's white matter and is characterized by congenital cataract, psychomotor development delays, and moderate intellectual disabilities. It is a type of leukoencephalopathy.
References
- 1 2 3 "OMIM MEGALENCEPHALIC LEUKOENCEPHALOPATHY WITH SUBCORTICAL CYSTS 1; MLC1". www.omim.org. Retrieved 2022-03-24.
- 1 2 van der Knaap, M. S.; Barth, P. G.; Stroink, H.; van Nieuwenhuizen, O.; Arts, W. F.; Hoogenraad, F.; Valk, J. (1995). "Leukoencephalopathy with swelling and a discrepantly mild clinical course in eight children". Annals of Neurology. 37 (3): 324–334. doi:10.1002/ana.410370308. ISSN 0364-5134. PMID 7695231. S2CID 29580717.
- ↑ "Megalencephalic leukoencephalopathy with subcortical cysts: MedlinePlus Genetics". medlineplus.gov. Retrieved 2022-03-24.
- ↑ "Vacuolar Myelopathy | NIH". clinicalinfo.hiv.gov. Retrieved 2022-03-24.
- ↑ Ilja Boor PK, de Groot K, Mejaski-Bosnjak V, et al. (June 2006). "Megalencephalic leukoencephalopathy with subcortical cysts: an update and extended mutation analysis of MLC1". Hum. Mutat. 27 (6): 505–12. doi: 10.1002/humu.20332 . PMID 16652334. S2CID 3174994.
- ↑ "Megalencephalic leukoencephalopathy with subcortical cysts - Genetics Home Reference" . Retrieved 2009-03-11.
- ↑ "MLC1 modulator of VRAC current 1 [Homo sapiens (human)] - Gene - NCBI". www.ncbi.nlm.nih.gov. Retrieved 2022-03-17.
- ↑ Leegwater, Peter A. J.; Yuan, Bao Qiang; van der Steen, Jeffrey; Mulders, Joyce; Könst, Andrea A. M.; Boor, P. K. Ilja; Mejaski-Bosnjak, Vlatka; van der Maarel, Silvère M.; Frants, Rune R.; Oudejans, Cees B. M.; Schutgens, Ruud B. H. (2001-04-01). "Mutations of MLC1 (KIAA0027), Encoding a Putative Membrane Protein, Cause Megalencephalic Leukoencephalopathy with Subcortical Cysts". The American Journal of Human Genetics. 68 (4): 831–838. doi:10.1086/319519. ISSN 0002-9297. PMC 1275636 . PMID 11254442.
- ↑ "Megalencephalic leukoencephalopathy with subcortical cysts protein 1 functionally cooperates with the TRPV4 cation channel to activate the response of astrocytes to osmotic stress: dysregulation by pathological mutations" . Retrieved 2022-03-17.
- ↑ "Molecular mechanisms of MLC1 and GLIALCAM mutations in megalencephalic leukoencephalopathy with subcortical cysts". academic.oup.com. Retrieved 2022-03-17.
- 1 2 3 4 Batla, Amit; Pandey, Sanjay; Nehru, Ravi (2011). "Megalencephalic leukoencephalopathy with subcortical cysts: A report of four cases". Journal of Pediatric Neurosciences. 6 (1): 74–77. doi: 10.4103/1817-1745.84416 (inactive 31 January 2024). PMC 3173924 . PMID 21977097.
{{cite journal}}: CS1 maint: DOI inactive as of January 2024 (link) - ↑ "Megalencephalic leukoencephalopathy with subcortical cysts | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Retrieved 2022-03-24.
- ↑ Topçu, Meral; Gartioux, Corine; Ribierre, Florence; Yalçinkaya, Cengiz; Tokus, Erem; Öztekin, Nese; Beckmann, Jacques S.; Ozguc, Meral; Seboun, Eric (February 1, 2000). "Vacuoliting Megalencephalic Leukoencephalopathy with Subcortical Cysts, Mapped to Chromosome 22qtel". The American Journal of Human Genetics. 66 (2): 733–739. doi:10.1086/302758. PMC 1288127 . PMID 10677334.
- ↑ Singhal, BS; Gursahani, RD; Udani, VP; Biniwale, AA (May 1996). "Megalencephalic leukodystrophy in an Asian Indian ethnic group". Pediatric Neurology. 14 (4): 291–6. doi:10.1016/0887-8994(96)00048-3. PMID 8805171.
- ↑ Singhal BS, Gursahani RD, Biniwale AA, Udani VP. Tokyo, Japan: In Proceedings of the 8th Asian and Oceanian Congress of Neurology; 1991. Megalencephalic leukodystrophy in India; p. 72.
- ↑ van der Knaap, Marjo S.; Wevers, Ron A.; Kure, Shigeo; Gabreëls, Fons J. M.; Verhoeven, Nanda M.; van Raaij-Selten, Bertie; Jaeken, Jaak (2 July 2016). "Increased Cerebrospinal Fluid Glycine: A Biochemical Marker for a Leukoencephalopathy With Vanishing White Matter". Journal of Child Neurology. 14 (11): 728–731. doi:10.1177/088307389901401108. PMID 10593550. S2CID 25535446.
- ↑ van der Knaap, Marjo S; Boor, Ilja; Estévez, Raúl (November 2012). "Megalencephalic leukoencephalopathy with subcortical cysts: chronic white matter oedema due to a defect in brain ion and water homoeostasis". The Lancet Neurology. 11 (11): 973–985. doi:10.1016/S1474-4422(12)70192-8. PMID 23079554. S2CID 31690619.