A cerebral arteriovenous malformation is an abnormal connection between the arteries and veins in the brain—specifically, an arteriovenous malformation in the cerebrum.

Papilledema or papilloedema is optic disc swelling that is caused by increased intracranial pressure due to any cause. The swelling is usually bilateral and can occur over a period of hours to weeks. Unilateral presentation is extremely rare.

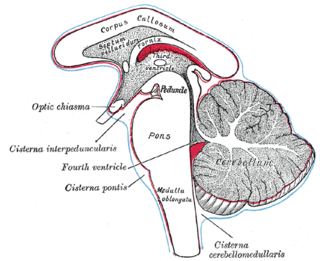
Hydrocephalus is a condition in which an accumulation of cerebrospinal fluid (CSF) occurs within the brain. This typically causes increased pressure inside the skull. Older people may have headaches, double vision, poor balance, urinary incontinence, personality changes, or mental impairment. In babies, it may be seen as a rapid increase in head size. Other symptoms may include vomiting, sleepiness, seizures, and downward pointing of the eyes.

Chiari malformation (CM) is a structural defect in the cerebellum, characterized by a downward displacement of one or both cerebellar tonsils through the foramen magnum. CMs can cause headaches, difficulty swallowing, vomiting, dizziness, neck pain, unsteady gait, poor hand coordination, numbness and tingling of the hands and feet, and speech problems. Less often, people may experience ringing or buzzing in the ears, weakness, slow heart rhythm, or fast heart rhythm, curvature of the spine (scoliosis) related to spinal cord impairment, abnormal breathing, such as central sleep apnea, characterized by periods of breathing cessation during sleep, and, in severe cases, paralysis.
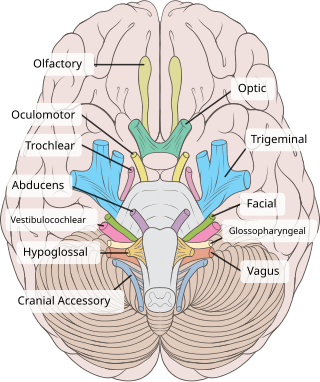
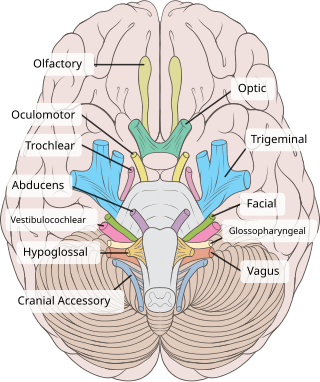
The trochlear nerve, also known as the fourth cranial nerve, cranial nerve IV, or CN IV, is a cranial nerve that innervates a single muscle - the superior oblique muscle of the eye. Unlike most other cranial nerves, the trochlear nerve is exclusively a motor nerve.

In neuroanatomy, dura mater is a thick membrane made of dense irregular connective tissue that surrounds the brain and spinal cord. It is the outermost of the three layers of membrane called the meninges that protect the central nervous system. The other two meningeal layers are the arachnoid mater and the pia mater. It envelops the arachnoid mater, which is responsible for keeping in the cerebrospinal fluid. It is derived primarily from the neural crest cell population, with postnatal contributions of the paraxial mesoderm.

Intracranial hemorrhage (ICH), also known as intracranial bleed, is bleeding within the skull. Subtypes are intracerebral bleeds, subarachnoid bleeds, epidural bleeds, and subdural bleeds. More often than not it ends in death.

Epidural hematoma is when bleeding occurs between the tough outer membrane covering the brain and the skull. Often there is loss of consciousness following a head injury, a brief regaining of consciousness, and then loss of consciousness again. Other symptoms may include headache, confusion, vomiting, and an inability to move parts of the body. Complications may include seizures.

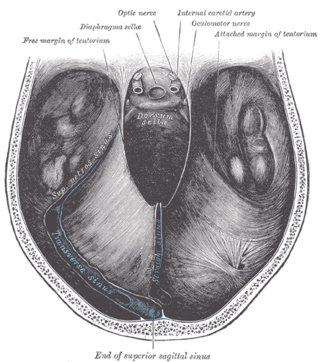
The falx cerebri is a large, crescent-shaped fold of dura mater that descends vertically into the longitudinal fissure between the cerebral hemispheres of the human brain, separating the two hemispheres and supporting dural sinuses that provide venous and CSF drainage to the brain. It is attached to the crista galli anteriorly, and blends with the tentorium cerebelli posteriorly.

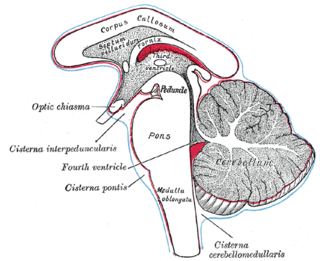
The cerebellar tentorium or tentorium cerebelli is an extension of the dura mater between the inferior aspect of the occipital lobes and the superior aspect of the cerebellum. The free border of the tentorium gives passage to the midbrain.
Abnormal posturing is an involuntary flexion or extension of the arms and legs, indicating severe brain injury. It occurs when one set of muscles becomes incapacitated while the opposing set is not, and an external stimulus such as pain causes the working set of muscles to contract. The posturing may also occur without a stimulus. Since posturing is an important indicator of the amount of damage that has occurred to the brain, it is used by medical professionals to measure the severity of a coma with the Glasgow Coma Scale and the Pediatric Glasgow Coma Scale.

Dandy–Walker malformation (DWM), also known as Dandy–Walker syndrome (DWS), is a rare congenital brain malformation in which the part joining the two hemispheres of the cerebellum does not fully form, and the fourth ventricle and space behind the cerebellum are enlarged with cerebrospinal fluid. Most of those affected develop hydrocephalus within the first year of life, which can present as increasing head size, vomiting, excessive sleepiness, irritability, downward deviation of the eyes and seizures. Other, less common symptoms are generally associated with comorbid genetic conditions and can include congenital heart defects, eye abnormalities, intellectual disability, congenital tumours, other brain defects such as agenesis of the corpus callosum, skeletal abnormalities, an occipital encephalocele or underdeveloped genitalia or kidneys. It is sometimes discovered in adolescents or adults due to mental health problems.
Duret haemorrhages are small linear areas of bleeding in the midbrain and upper pons of the brainstem. They are caused by a traumatic downward displacement of the brainstem.
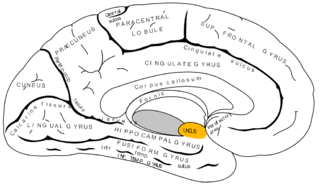
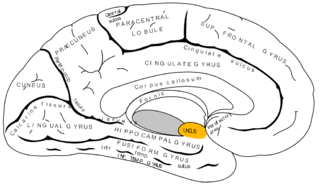
The uncus is an anterior extremity of the parahippocampal gyrus. It is separated from the apex of the temporal lobe by a slight fissure called the incisura temporalis.

The cerebellar tonsil is a rounded lobule on the undersurface of each cerebellar hemisphere, continuous medially with the uvula of the cerebellar vermis and superiorly by the flocculonodular lobe. Synonyms include: tonsilla cerebelli, amygdala cerebelli, the latter of which is not to be confused with the cerebral tonsils or amygdala nuclei located deep within the medial temporal lobes of the cerebral cortex.
Kernohan's notch is a cerebral peduncle indentation associated with some forms of transtentorial herniation. It is a secondary condition caused by a primary injury on the opposite hemisphere of the brain. Kernohan's notch is an ipsilateral condition, in that a left-sided primary lesion evokes motor impairment in the left side of the body and a right-sided primary injury evokes motor impairment in the right side of the body. The seriousness of Kernohan's notch varies depending on the primary problem causing it, which may range from benign brain tumors to advanced subdural hematoma.

A cerebrospinal fluid leak is a medical condition where the cerebrospinal fluid (CSF) surrounding the brain or spinal cord leaks out of one or more holes or tears in the dura mater. A cerebrospinal fluid leak can be either cranial or spinal, and these are two different disorders. A spinal CSF leak can be caused by one or more meningeal diverticula or CSF-venous fistulas not associated with an epidural leak.
Basilar invagination is invagination (infolding) of the base of the skull that occurs when the top of the C2 vertebra migrates upward. It can cause narrowing of the foramen magnum. It also may press on the lower brainstem.

Macrocephaly-capillary malformation (M-CM) is a multiple malformation syndrome causing abnormal body and head overgrowth and cutaneous, vascular, neurologic, and limb abnormalities. Though not every patient has all features, commonly found signs include macrocephaly, congenital macrosomia, extensive cutaneous capillary malformation, body asymmetry, polydactyly or syndactyly of the hands and feet, lax joints, doughy skin, variable developmental delay and other neurologic problems such as seizures and low muscle tone.
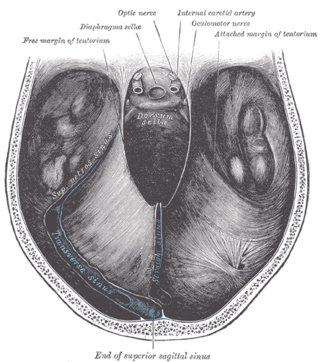
The tentorial notch refers to the anterior opening between the free edge of the cerebellar tentorium and the clivus for the passage of the brainstem.