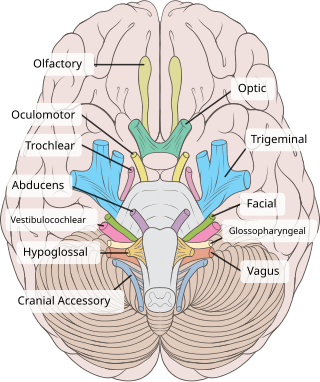
Cranial nerves are the nerves that emerge directly from the brain, of which there are conventionally considered twelve pairs. Cranial nerves relay information between the brain and parts of the body, primarily to and from regions of the head and neck, including the special senses of vision, taste, smell, and hearing.

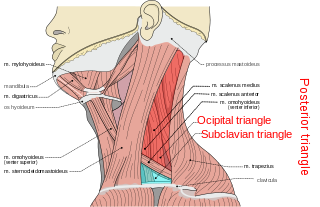
The neck is the part of the body on many vertebrates that connects the head with the torso. The neck supports the weight of the head and protects the nerves that carry sensory and motor information from the brain down to the rest of the body. In addition, the neck is highly flexible and allows the head to turn and flex in all directions. The structures of the human neck are anatomically grouped into four compartments: vertebral, visceral and two vascular compartments. Within these compartments, the neck houses the cervical vertebrae and cervical part of the spinal cord, upper parts of the respiratory and digestive tracts, endocrine glands, nerves, arteries and veins. Muscles of the neck are described separately from the compartments. They bound the neck triangles.

Tetraplegia, also known as quadriplegia, is defined as the dysfunction or loss of motor and/or sensory function in the cervical area of the spinal cord. A loss of motor function can present as either weakness or paralysis leading to partial or total loss of function in the arms, legs, trunk, and pelvis; paraplegia is similar but affects the thoracic, lumbar, and sacral segments of the spinal cord and arm function is retained. The paralysis may be flaccid or spastic. A loss of sensory function can present as an impairment or complete inability to sense light touch, pressure, heat, pinprick/pain, and proprioception. In these types of spinal cord injury, it is common to have a loss of both sensation and motor control.

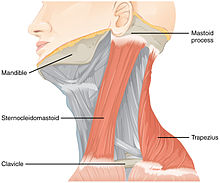
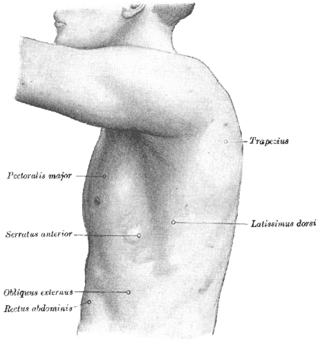
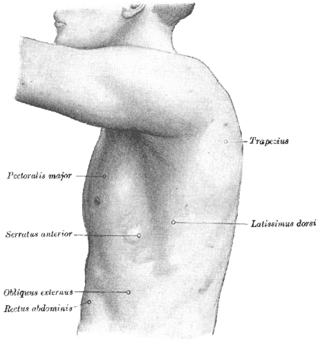
The trapezius is a large paired trapezoid-shaped surface muscle that extends longitudinally from the occipital bone to the lower thoracic vertebrae of the spine and laterally to the spine of the scapula. It moves the scapula and supports the arm.

The latissimus dorsi is a large, flat muscle on the back that stretches to the sides, behind the arm, and is partly covered by the trapezius on the back near the midline. The word latissimus dorsi comes from Latin and means "broadest [muscle] of the back", from "latissimus" and "dorsum". The pair of muscles are commonly known as "lats", especially among bodybuilders. The latissimus dorsi is the largest muscle in the upper body.

The brachial plexus is a network of nerves formed by the anterior rami of the lower four cervical nerves and first thoracic nerve. This plexus extends from the spinal cord, through the cervicoaxillary canal in the neck, over the first rib, and into the armpit, it supplies afferent and efferent nerve fibers to the chest, shoulder, arm, forearm, and hand.
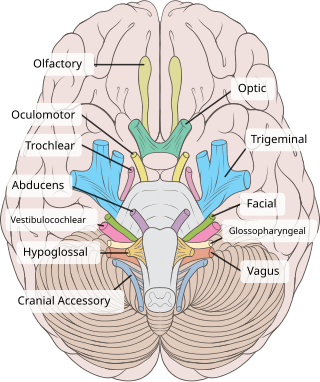
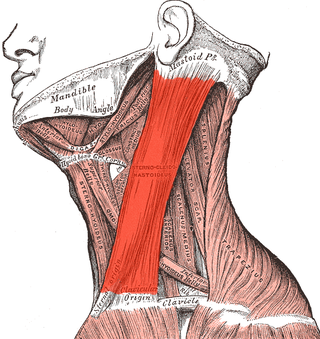
The accessory nerve, also known as the eleventh cranial nerve, cranial nerve XI, or simply CN XI, is a cranial nerve that supplies the sternocleidomastoid and trapezius muscles. It is classified as the eleventh of twelve pairs of cranial nerves because part of it was formerly believed to originate in the brain. The sternocleidomastoid muscle tilts and rotates the head, whereas the trapezius muscle, connecting to the scapula, acts to shrug the shoulder.

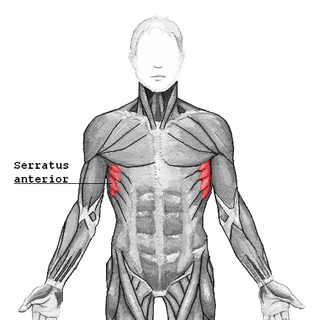
The long thoracic nerve is a branch of the brachial plexus derived from cervical nerves C5-C7 that innervates the serratus anterior muscle.
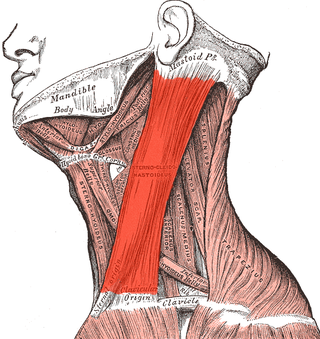
The sternocleidomastoid muscle is one of the largest and most superficial cervical muscles. The primary actions of the muscle are rotation of the head to the opposite side and flexion of the neck. The sternocleidomastoid is innervated by the accessory nerve.

The levator scapulae is a slender skeletal muscle situated at the back and side of the neck. It originates from the transverse processes of the four uppermost cervical vertebrae; it inserts onto the upper portion of the medial border of the scapula. It is innervated by the cervical nerves C3-C4, and frequently also by the dorsal scapular nerve. As the Latin name suggests, its main function is to lift the scapula.
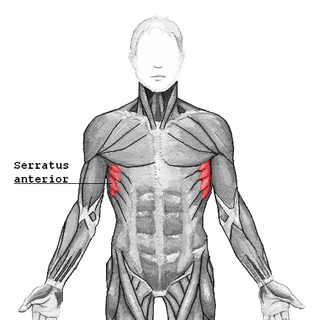
The serratus anterior is a muscle of the chest. It originates at the side of the chest from the upper 8 or 9 ribs; it inserts along the entire length of the anterior aspect of the medial border of the scapula. It is innervated by the long thoracic nerve from the brachial plexus. The serratus anterior acts to pull the scapula forward around the thorax.

A brachial plexus injury (BPI), also known as brachial plexus lesion, is an injury to the brachial plexus, the network of nerves that conducts signals from the spinal cord to the shoulder, arm and hand. These nerves originate in the fifth, sixth, seventh and eighth cervical (C5–C8), and first thoracic (T1) spinal nerves, and innervate the muscles and skin of the chest, shoulder, arm and hand.
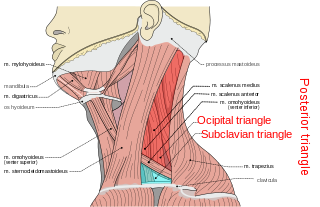
The posterior triangle is a region of the neck.

The transverse cervical artery is an artery in the neck and a branch of the thyrocervical trunk, running at a higher level than the suprascapular artery.

The nerve point of the neck, also known as Erb's point, is a site at the upper trunk of the brachial plexus located 2–3 cm above the clavicle. It is named for Wilhelm Heinrich Erb. Taken together, there are six types of nerves that meet at this point.
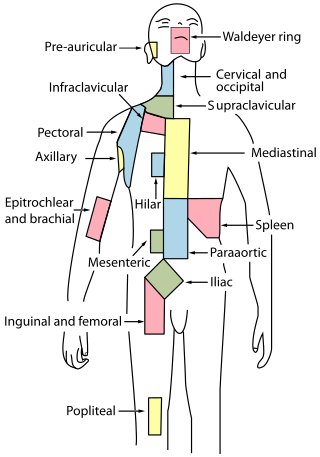
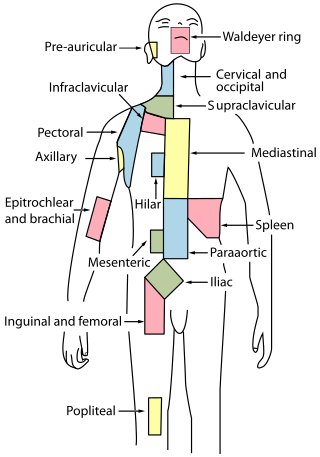
Cervical lymph nodes are lymph nodes found in the neck. Of the 800 lymph nodes in the human body, 300 are in the neck. Cervical lymph nodes are subject to a number of different pathological conditions including tumours, infection and inflammation.
A winged scapula is a skeletal medical condition in which the shoulder blade protrudes from a person's back in an abnormal position.
Shoulder surgery is a means of treating injured shoulders. Many surgeries have been developed to repair the muscles, connective tissue, or damaged joints that can arise from traumatic or overuse injuries to the shoulder.

Smile surgery or smile reconstruction is a surgical procedure that restores the smile for people with facial nerve paralysis. Facial nerve paralysis is a relatively common condition with a yearly incidence of 0.25% leading to function loss of the mimic muscles. The facial nerve gives off several branches in the face. If one or more facial nerve branches are paralysed, the corresponding mimetic muscles lose their ability to contract. This may lead to several symptoms such as incomplete eye closure with or without exposure keratitis, oral incompetence, poor articulation, dental caries, drooling, and a low self-esteem. This is because the different branches innervate the frontalis muscle, orbicularis oculi and oris muscles, lip elevators and depressors, and the platysma. The elevators of the upper lip and corner of the mouth are innervated by the zygomatic and buccal branches. When these branches are paralysed, there is an inability to create a symmetric smile.
The Eden–Lange procedure is an orthopedic procedure to alleviate the symptoms of trapezius palsy when more conservative measures, such as spontaneous resolution and surgical nerve repair are not promising. The rhomboid major, rhomboid minor, and levator scapulae muscles are transferred laterally along the scapula to replace the functions of the lower, middle, and upper fibers of the trapezius, respectively. The transferred muscles hold the scapula in a more medial and upwardly rotated position, without winging.