Related Research Articles
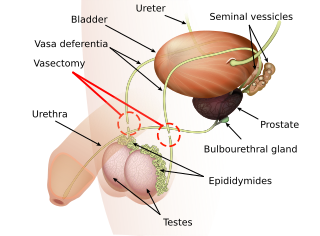
Vasectomy is an elective surgical procedure that results in male sterilization, often as a means of permanent contraception. During the procedure, the male vasa deferentia are cut and tied or sealed so as to prevent sperm from entering into the urethra and thereby prevent fertilization of a female through sexual intercourse. Vasectomies are usually performed in a physician's office, medical clinic, or, when performed on a non-human animal, in a veterinary clinic. Hospitalization is not normally required as the procedure is not complicated, the incisions are small, and the necessary equipment routine.
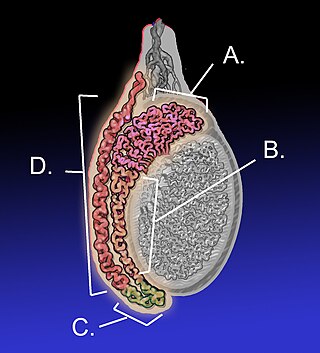
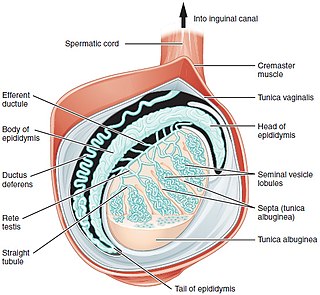
The epididymis is an elongated tubular structure attached to the posterior side of each one of the two male reproductive glands, the testicles. It is a single, narrow, tightly coiled tube in adult humans, 6 to 7 centimetres in length; uncoiled the tube would be approximately 6 m long. It connects the testicle to the vas deferens in the male reproductive system. The epididymis serves as an interconnection between the multiple efferent ducts at the rear of a testicle (proximally), and the vas deferens (distally). Its primary function is the storage, maturation and transport of sperm cells.

The vas deferens, with the more modern name ductus deferens, is part of the male reproductive system of many vertebrates. The ducts transport sperm from the epididymides to the ejaculatory ducts in anticipation of ejaculation. The vas deferens is a partially coiled tube which exits the abdominal cavity through the inguinal canal.

Spermatocele is a fluid-filled cyst that develops in the epididymis. The fluid is usually a clear or milky white color and may contain sperm. Spermatoceles are typically filled with spermatozoa and they can vary in size from several millimeters to many centimeters. Small spermatoceles are relatively common, occurring in an estimated 30 percent of males. They are generally not painful. However, some people may experience discomfort such as a dull pain in the scrotum from larger spermatoceles. They are not cancerous, nor do they cause an increased risk of testicular cancer. Additionally, unlike varicoceles, they do not reduce fertility.
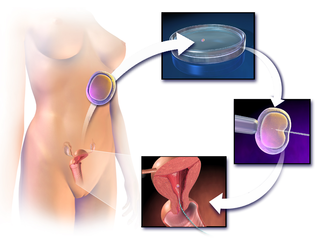
Assisted reproductive technology (ART) includes medical procedures used primarily to address infertility. This subject involves procedures such as in vitro fertilization (IVF), intracytoplasmic sperm injection (ICSI), cryopreservation of gametes or embryos, and/or the use of fertility medication. When used to address infertility, ART may also be referred to as fertility treatment. ART mainly belongs to the field of reproductive endocrinology and infertility. Some forms of ART may be used with regard to fertile couples for genetic purpose. ART may also be used in surrogacy arrangements, although not all surrogacy arrangements involve ART. The existence of sterility will not always require ART to be the first option to consider, as there are occasions when its cause is a mild disorder that can be solved with more conventional treatments or with behaviors based on promoting health and reproductive habits.

Microsurgery is a general term for surgery requiring an operating microscope. The most obvious developments have been procedures developed to allow anastomosis of successively smaller blood vessels and nerves which have allowed transfer of tissue from one part of the body to another and re-attachment of severed parts. Microsurgical techniques are utilized by several specialties today, such as general surgery, ophthalmology, orthopedic surgery, gynecological surgery, otolaryngology, neurosurgery, oral and maxillofacial surgery, endodontic microsurgery, plastic surgery, podiatric surgery and pediatric surgery.

Vas-occlusive contraception is a form of male contraception that blocks sperm transport in the vas deferens, the tubes that carry sperm from the epididymis to the ejaculatory ducts.
Vasovasostomy is a surgery by which vasectomies are partially reversed. Another surgery for vasectomy reversal is vasoepididymostomy.

Azoospermia is the medical condition of a man whose semen contains no sperm. It is associated with male infertility, but many forms are amenable to medical treatment. In humans, azoospermia affects about 1% of the male population and may be seen in up to 20% of male infertility situations in Canada.
Terms oligospermia, oligozoospermia, and low sperm count refer to semen with a low concentration of sperm and is a common finding in male infertility. Often semen with a decreased sperm concentration may also show significant abnormalities in sperm morphology and motility. There has been interest in replacing the descriptive terms used in semen analysis with more quantitative information.
Congenital absence of the vas deferens (CAVD) is a condition in which the vasa deferentia reproductive organs fail to form properly prior to birth. It may either be unilateral (CUAVD) or bilateral (CBAVD).
Testicular sperm extraction (TESE) is a surgical procedure in which a small portion of tissue is removed from the testicle and any viable sperm cells from that tissue are extracted for use in further procedures, most commonly intracytoplasmic sperm injection (ICSI) as part of in vitro fertilisation (IVF). TESE is often recommended to patients who cannot produce sperm by ejaculation due to azoospermia.
Post-vasectomy pain syndrome (PVPS) is a chronic and sometimes debilitating genital pain condition that may develop immediately or several years after vasectomy. Because this condition is a syndrome, there is no single treatment method, therefore efforts focus on mitigating/relieving the individual patient's specific pain. When pain in the epididymides is the primary symptom, post-vasectomy pain syndrome is often described as congestive epididymitis.
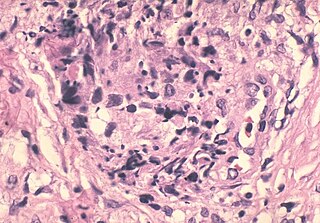
A sperm granuloma is a lump of leaked sperm that appears along the vasa deferentia or epididymides in vasectomized individuals. While the majority of sperm granulomas are present along the vas deferens, the rest of them form at the epididymis. Sperm granulomas range in size, from one millimeter to one centimeter. They consist of a central mass of degenerating sperm surrounded by tissue containing blood vessels and immune system cells. Sperm granulomas may also have a yellow, white, or cream colored center when cut open. While some sperm granulomas can be painful, most of them are painless and asymptomatic. Sperm granulomas can appear as a result of surgery, trauma, or an infection. They can appear as early as four days after surgery and fully formed ones can appear as late as 208 days later.
Sarcoidosis is a systemic disease of unknown cause that results in the formation of non-caseating granulomas in multiple organs. The prevalence is higher among black males than white males by a ratio of 20:1. Usually the disease is localized to the chest, but urogenital involvement is found in 0.2% of clinically diagnosed cases and 5% of those diagnosed at necropsy. The kidney is the most frequently affected urogenital organ, followed in men by the epididymis. Testicular sarcoidosis can present as a diffuse painless scrotal mass or can mimic acute epididymo-orchitis. Usually it appears with systemic manifestations of the disease. Since it causes occlusion and fibrosis of the ductus epididymis, fertility may be affected. On ultrasound, the hypoechogenicity and ‘infiltrative’ pattern seen in the present case are recognized features. Opinions differ on the need for histological proof, with reports of limited biopsy and frozen section, radical orchiectomy in unilateral disease and unilateral orchiectomy in bilateral disease. The peak incidence of sarcoidosis and testicular neoplasia coincide at 20–40 years and this is why most patients end up having an orchiectomy. However, testicular tumours are much more common in white men, less than 3.5% of all testicular tumours being found in black men. These racial variations justify a more conservative approach in patients of Afro-Caribbean descent with proven sarcoidosis elsewhere. Careful follow-up and ultrasonic surveillance may be preferable in certain clinical settings to biopsy and surgery, especially in patients with bilateral testicular disease.
Reproductive surgery is surgery in the field of reproductive medicine. It can be used for contraception, e.g. in vasectomy, wherein the vasa deferentia of a male are severed, but is also used plentifully in assisted reproductive technology. Reproductive surgery is generally divided into three categories: surgery for infertility, in vitro fertilization, and fertility preservation.
FNA mapping is an application of fine-needle aspiration (FNA) to the testis for the diagnosis of male infertility. FNA cytology has been used to examine pathological human tissue from various organs for over 100 years. As an alternative to open testicular biopsy for the last 40 years, FNA mapping has helped to characterize states of human male infertility due to defective spermatogenesis. Although recognized as a reliable, and informative technique, testis FNA has not been widely used in U.S. to evaluate male infertility. Recently, however, testicular FNA has gained popularity as both a diagnostic and therapeutic tool for the management of clinical male infertility for several reasons:
- The testis is an ideal organ for evaluation by FNA because of its uniform cellularity and easy accessibility.
- The trend toward minimally invasive procedures and cost-containment views FNA favorably compared to surgical testis biopsy.
- The realization that the specific histologic abnormality observed on testis biopsy has no definite correlation to either the etiology of infertility or to the ability to find sperm for assisted reproduction.
- Assisted reproduction has undergone dramatic advances such that testis sperm are routinely used for biological pregnancies, thus fueling the development of novel FNA techniques to both locate and procure sperm.
Vasoepididymostomy or epididymovasostomy is a surgery by which vasectomies are reversed. It involves connection of the severed vas deferens to the epididymis and is more technically demanding than the vasovasostomy.
No-scalpel vasectomy is a type of vasectomy procedure in which a specifically designed ringed clamp and dissecting hemostat is used to puncture the scrotum to access the vas deferens. This is different from a conventional or incisional vasectomy where the scrotal opening is made with a scalpel. The NSV approach offers several benefits, including lower risk for bleeding, bruising, infection, and pain. The NSV approach also has a shorter procedure time than the conventional scalpel incision technique. Both approaches to vasectomy are equally effective. Because of the inherent simplicity of the procedure it affords itself to be used in public health programs worldwide. This method is used in over 40 countries for male sterilisation.
Marc Goldstein, MD, DSc (hon), FACS is an American urologist and the Matthew P. Hardy Distinguished Professor of Reproductive Medicine, and Urology at Weill Cornell Medical College; Surgeon-in-Chief, Male Reproductive Medicine and Surgery; and Director of the Center of Male Reproductive Medicine and Microsurgery at New York Presbyterian Hospital. He is Adjunct Senior Scientist with the Population Council's Center for Biomedical Research, located on the campus of Rockefeller University.
References
- ↑ "Vasectomy Guideline - American Urological Association". www.auanet.org. Retrieved 2022-06-09.
- ↑ Lee H.Y. a 20-year experience with vasovasostomy. J. Urol. 136: 413, 1986, PMID 3525857
- 1 2 Yang et al. The kinetics of the return of sperm to the ejaculate after the vasectomy reversal. J. Urol. 177: 2271, 2007, PMID 17509339
- ↑ Patel SR, Sigman M. Comparison of outcomes of vasovasostomy performed in the convoluted and straight vas deferens. J. Urol. 179: 256, 2008, PMID 18001786
- ↑ Parekatill SJ et al. Multi-institution validation of vasectomy reversal predictor. J. Urol. 175: 24, 2006, PMID 16406922
- 1 2 Belker AM et al. Results of 1,469 microsurgical vasectomy reversals by the Vasovasostomy Study Group. J. Urol. 145: 505, 1991, PMID 1997700
- ↑ Bastuba, Martin. "Vasectomy Reversal Success Rates". MaleFertility.md. Retrieved 16 September 2015.
- ↑ Schwarzer, JU "Vasectomy Reversal using a micro-surgical three layer technique: one surgeon's experience over 18 years with 1300 patients" in International Journal of Andrology April 20, 2012
- ↑ Ansbacher, R. Humoral sperm antibodies: a 10-year follow-up of vas-ligated men. Fertil Steril 36: 222, 1981, PMID 7262338
- ↑ Turek PJ. Immunopathology and Infertility. In: Infertility in the Male, 3rd ed. Edited by LI Lipshultz and SS Howards. Mosby Year Book, Philadelphia, 1997.
- ↑ Eisenberg ML et al. Use of viscoelastic solution to improve visualization during urologic microsurgery: evaluation of patency after vasovasostomy. Urol. 73: 134, 2009, PMID 18977020
- ↑ Schiff J et al. Outcome and late failures compared in 4 techniques of vasoepididymostomy in 153 consecutive men. J. Urol. 174: 651, 2005, PMID 16006931
- ↑ Kolettis PN et al. Effect of seminal oxidative stress on fertility after vasectomy reversal. Fertil Steril. 71: 249, 1999, PMID 9988393
- ↑ Pavlovich CP et al. Fertility options after vasectomy: A cost effectiveness analysis. Fertil Steril. 67: 133, 1997, PMID 8986698
- 1 2 Meng MV et al. Surgery or assisted reproduction? A decision analysis of treatment costs in male infertility. J. Urol. 174: 1926, 2005, PMID 16217347
- 1 2 Hsieh MH et al. Markov modeling of vasectomy reversal and ART: How do obstructive interval and female partner age influence cost-effectiveness? Fertil Steril. 88: 840, 2007, PMID 17544418
- ↑ Gerrard ER et al. Effect of female partner age on pregnancy rates after vasectomy reversal. Fertil Steril. 87: 1340, 2007, PMID 17258213
- ↑ Griffen et al. How little is enough? The evidence for post vasectomy testing. J. Urol. 174: 29, 2005, PMID 15947571
- ↑ Sharma et al. Vasectomy demographics and postvasectomy desire for future children: results from a contemporary national survey Fertil Steril. 99: 1880, 2013 PMID 23541407
- ↑ "Vasectomy reversal: first cut isn't final". The Independent. 2009-03-29. Retrieved 2023-06-23.
- ↑ Thonneua P, D'Isle B. Does vasectomy have long-term effects on somatic and psychological health status? international J of Andrology 13, 419 PMID 2096110
- 1 2 3 Murphy, Clare "18 March 2009 viewable at: http://news.bbc.co.uk/1/hi/health/7948690.stm
- ↑ Nylen C.O. Acta Otolaryngologica 73: 453, 1972
- ↑ Owen E.R. Microsurgery in common cases of male infertility. Int Surg 91 (5 suppl): 85-89, 2006, PMID 17436609