Cardiology is the study of the heart. Cardiology is a branch of medicine that deals with disorders of the heart and the cardiovascular system. The field includes medical diagnosis and treatment of congenital heart defects, coronary artery disease, heart failure, valvular heart disease, and electrophysiology. Physicians who specialize in this field of medicine are called cardiologists, a specialty of internal medicine. Pediatric cardiologists are pediatricians who specialize in cardiology. Physicians who specialize in cardiac surgery are called cardiothoracic surgeons or cardiac surgeons, a specialty of general surgery.

Blood pressure (BP) is the pressure of circulating blood against the walls of blood vessels. Most of this pressure results from the heart pumping blood through the circulatory system. When used without qualification, the term "blood pressure" refers to the pressure in a brachial artery, where it is most commonly measured. Blood pressure is usually expressed in terms of the systolic pressure over diastolic pressure in the cardiac cycle. It is measured in millimeters of mercury (mmHg) above the surrounding atmospheric pressure, or in kilopascals (kPa). The difference between the systolic and diastolic pressures is known as pulse pressure, while the average pressure during a cardiac cycle is known as mean arterial pressure.

Hypertension, also known as high blood pressure, is a long-term medical condition in which the blood pressure in the arteries is persistently elevated. High blood pressure usually does not cause symptoms itself. It is, however, a major risk factor for stroke, coronary artery disease, heart failure, atrial fibrillation, peripheral arterial disease, vision loss, chronic kidney disease, and dementia. Hypertension is a major cause of premature death worldwide.

A sphygmomanometer, also known as a blood pressure monitor, or blood pressure gauge, is a device used to measure blood pressure, composed of an inflatable cuff to collapse and then release the artery under the cuff in a controlled manner, and a mercury or aneroid manometer to measure the pressure. Manual sphygmomanometers are used with a stethoscope when using the auscultatory technique.
Antihypertensives are a class of drugs that are used to treat hypertension. Antihypertensive therapy seeks to prevent the complications of high blood pressure, such as stroke, heart failure, kidney failure and myocardial infarction. Evidence suggests that reduction of the blood pressure by 5 mmHg can decrease the risk of stroke by 34% and of ischaemic heart disease by 21%, and can reduce the likelihood of dementia, heart failure, and mortality from cardiovascular disease. There are many classes of antihypertensives, which lower blood pressure by different means. Among the most important and most widely used medications are thiazide diuretics, calcium channel blockers, ACE inhibitors, angiotensin II receptor antagonists (ARBs), and beta blockers.

Indapamide is a thiazide-like diuretic drug used in the treatment of hypertension, as well as decompensated heart failure. Combination preparations with perindopril are available. The thiazide-like diuretics reduce risk of major cardiovascular events and heart failure in hypertensive patients compared with hydrochlorothiazide with a comparable incidence of adverse events. Both thiazide diuretics and thiazide-like diuretics are effective in reducing risk of stroke. Both drug classes appear to have comparable rates of adverse effects as other antihypertensives such as angiotensin II receptor blockers and dihydropyridine calcium channel blockers and lesser prevalence of side-effects when compared to ACE-inhibitors and non-dihydropyridine calcium channel blockers.

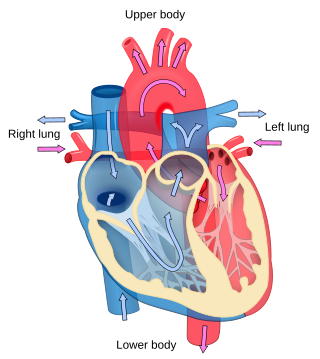
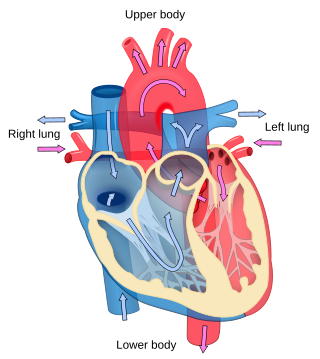
A pulmonary artery catheter (PAC), also known as a Swan-Ganz catheter or right heart catheter, is a balloon-tipped catheter that is inserted into a pulmonary artery in a procedure known as pulmonary artery catheterization or right heart catheterization. Pulmonary artery catheterization is a useful measure of the overall function of the heart particularly in those with complications from heart failure, heart attack, arrythmias or pulmonary embolism. It is also a good measure for those needing intravenous fluid therapy, for instance post heart surgery, shock, and severe burns. The procedure can also be used to measure pressures in the heart chambers.
Sir Richard Peto is an English statistician and epidemiologist who is Professor of Medical Statistics and Epidemiology at the University of Oxford, England.

Alan Julian Macbeth Tudor-Hart, commonly known as Julian Tudor Hart, was a general practitioner (GP) who worked in Wales for 30 years, known for theorising the inverse care law. He produced medical research and wrote many books and medical articles.

Perindopril is a medication used to treat high blood pressure, heart failure, or stable coronary artery disease.
Hypertensive encephalopathy (HE) is general brain dysfunction due to significantly high blood pressure. Symptoms may include headache, vomiting, trouble with balance, and confusion. Onset is generally sudden. Complications can include seizures, posterior reversible encephalopathy syndrome, and bleeding in the back of the eye.

Ambulatory blood pressure, as opposed to office blood pressure, is the blood pressure over the course of the full 24-hour sleep-wake cycle. Ambulatory blood pressure monitoring (ABPM) measures blood pressure at regular intervals throughout the day and night. It avoids the white coat hypertension effect in which a patient's blood pressure is elevated during the examination process due to nervousness and anxiety caused by being in a clinical setting. ABPM can also detect the reverse condition, masked hypertension, where the patient has normal blood pressure during the examination but uncontrolled blood pressure outside the clinical setting, masking a high 24-hour average blood pressure. Out-of-office measurements are highly recommended as an adjunct to office measurements by almost all hypertension organizations.
Prehypertension, also known as high normal blood pressure and borderline hypertensive (BH), is a medical classification for cases where a person's blood pressure is elevated above optimal or normal, but not to the level considered hypertension. Prehypertension is now referred to as "elevated blood pressure" by the American College of Cardiology (ACC) and the American Heart Association (AHA). The ACC/AHA define elevated blood pressure as readings with a systolic pressure from 120 to 129 mm Hg and a diastolic pressure under 80 mm Hg, Readings greater than or equal to 130/80 mm Hg are considered hypertension by ACC/AHA and if greater than or equal to 140/90 mm Hg by ESC/ESH. and the European Society of Hypertension defines "high normal blood pressure" as readings with a systolic pressure from 130 to 139 mm Hg and a diastolic pressure 85-89 mm Hg.
CYT006-AngQb was an investigational vaccine against angiotensin II, designed to lower blood pressure. It was somewhat effective in clinical trials, but less so than conventional drugs against hypertension.
Renal sympathetic denervation (RSDN) is a minimally invasive, endovascular catheter based procedure using radiofrequency ablation or ultrasound ablation aimed at treating resistant hypertension. Nerves in the wall of the renal artery are ablated by applying radiofrequency pulses or ultrasound to the renal arteries. This causes reduction of sympathetic afferent and efferent activity to the kidney and blood pressure can be decreased. Early data from international clinical trials without sham controls was promising - demonstrating large blood pressure reductions in patients with treatment-resistant hypertension. However, in 2014 a prospective, single-blind, randomized, sham-controlled clinical trial failed to confirm a beneficial effect on blood pressure. A 2014 consensus statement from The Joint UK Societies did not recommend the use of renal denervation for treatment of resistant hypertension on current evidence. More recent sham-controlled trials suggest renal denervation can lead to lower systolic blood pressure.

Arterial blood pressure is most commonly measured via a sphygmomanometer, which historically used the height of a column of mercury to reflect the circulating pressure. Blood pressure values are generally reported in millimetres of mercury (mmHg), though aneroid and electronic devices do not contain mercury.
Thomas G. Pickering was a British physician and academic. He was a professor of medicine at College of Physicians and Surgeons, Columbia University Medical Center in New York City. He was an internationally renowned expert in clinical hypertension and a leader in the fields of hypertension and cardiovascular behavioral medicine. He coined the term "white-coat hypertension" to describe those whose blood pressure was elevated in the doctor's office, but normal in everyday life. He later published the first editorial describing "masked hypertension". He also discovered and gave his name to the Pickering Syndrome, where bilateral renal artery stenosis causes flash pulmonary edema.
Una Martin is an emeritus professor of clinical pharmacology and was formerly the deputy pro-vice chancellor for equalities at the University of Birmingham. She is an expert in hypertension and ambulatory monitoring. She is a Fellow of the British Pharmacological Society.

Labile hypertension occurs when there are unexpected changes in blood pressure. The term can be used to describe when people have blood pressure measurements that abruptly fluctuate from being abnormally high, approximately 140/90mm Hg or over and returns to its normal range.
Refractory hypertension(RfHTN) is hypertension, a high blood pressure, that remains uncontrolled on maximal or near-maximal therapy, that includes the use of ≥5 antihypertensive agents of different classes. Agents used include a long-acting thiazide-like diuretic (such as chlorthalidone) and spironolactone. Refractory hypertension is typically associated with increased sympathetic nervous system activity. The phenotype of refractory hypertension was first proposed in a retrospective analysis of patients referred to the University of Alabama at Birmingham Hypertension Clinic whose blood pressure could not be controlled on any antihypertensive regimen.