Clinical chemistry is a division in medical laboratory sciences focusing on qualitative tests of important compounds, referred to as analytes or markers, in bodily fluids and tissues using analytical techniques and specialized instruments. This interdisciplinary field includes knowledge from medicine, biology, chemistry, biomedical engineering, informatics, and an applied form of biochemistry.

Newborn screening (NBS) is a public health program of screening in infants shortly after birth for conditions that are treatable, but not clinically evident in the newborn period. The goal is to identify infants at risk for these conditions early enough to confirm the diagnosis and provide intervention that will alter the clinical course of the disease and prevent or ameliorate the clinical manifestations. NBS started with the discovery that the amino acid disorder phenylketonuria (PKU) could be treated by dietary adjustment, and that early intervention was required for the best outcome. Infants with PKU appear normal at birth, but are unable to metabolize the essential amino acid phenylalanine, resulting in irreversible intellectual disability. In the 1960s, Robert Guthrie developed a simple method using a bacterial inhibition assay that could detect high levels of phenylalanine in blood shortly after a baby was born. Guthrie also pioneered the collection of blood on filter paper which could be easily transported, recognizing the need for a simple system if the screening was going to be done on a large scale. Newborn screening around the world is still done using similar filter paper. NBS was first introduced as a public health program in the United States in the early 1960s, and has expanded to countries around the world.
Quest Diagnostics Incorporated is an American clinical laboratory. A Fortune 500 company, Quest operates in the United States, Puerto Rico, Mexico, and Brazil. Quest also maintains collaborative agreements with various hospitals and clinics across the globe.
The Clinical Laboratory Improvement Amendments (CLIA) of 1988 are United States federal regulatory standards that apply to all clinical laboratory testing performed on humans in the United States, except clinical trials and basic research.
Clinical pathology is a medical specialty that is concerned with the diagnosis of disease based on the laboratory analysis of bodily fluids, such as blood, urine, and tissue homogenates or extracts using the tools of chemistry, microbiology, hematology, molecular pathology, and Immunohaematology. This specialty requires a medical residency.

A Medical Laboratory Scientist (MLS) or Clinical Laboratory Scientist (CLS) or Medical Technologist (MT) is a licensed Healthcare professional who performs diagnostic testing of body fluids, blood and other body tissue. The Medical Technologist is tasked with releasing the patient results to aid in further treatment. The scope of a medical laboratory scientist's work begins with the receipt of patient or client specimens and finishes with the delivery of test results to physicians and other healthcare providers. The utility of clinical diagnostic testing relies squarely on the validity of test methodology. To this end, much of the work done by medical laboratory scientists involves ensuring specimen quality, interpreting test results, data-logging, testing control products, performing calibration, maintenance, validation, and troubleshooting of instrumentation as well as performing statistical analyses to verify the accuracy and repeatability of testing. Medical laboratory scientists may also assist healthcare providers with test selection and specimen collection and are responsible for prompt verbal delivery of critical lab results. Medical Laboratory Scientists in healthcare settings also play an important role in clinical diagnosis. An estimated 70% of medical decisions are based on laboratory test results and MLS contributions affect 95% of a health system's costs.
The Association of Public Health Laboratories (APHL) is a membership organization in the United States representing the laboratories that protect the health and safety of the public. APHL serves as a liaison between public health laboratories and federal and international agencies. Membership consists of local, state, county, and territorial public health laboratories; public health environmental, agricultural and veterinary laboratories; and corporations and individuals with an interest in public health and laboratory science. APHL is a non-profit, 501(c)(3) organization with a history of over fifty years.
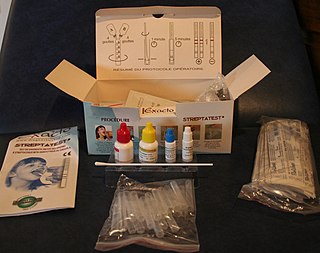
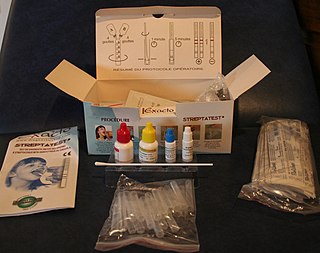
Point-of-care testing (POCT), also called near-patient testing or bedside testing, is defined as medical diagnostic testing at or near the point of care—that is, at the time and place of patient care. This contrasts with the historical pattern in which testing was wholly or mostly confined to the medical laboratory, which entailed sending off specimens away from the point of care and then waiting hours or days to learn the results, during which time care must continue without the desired information.
James Linder is an American author, academic and businessperson, as well as an authority on university research commercialization. He is chief executive officer (CEO) of Nebraska Medicine, and most recently was president of the University Technology Development Corporation and chief strategist for the University of Nebraska system. He is also a professor of pathology and microbiology at the University of Nebraska Medical Center.

A medical laboratory or clinical laboratory is a laboratory where tests are conducted out on clinical specimens to obtain information about the health of a patient to aid in diagnosis, treatment, and prevention of disease. Clinical medical laboratories are an example of applied science, as opposed to research laboratories that focus on basic science, such as found in some academic institutions.
Laboratory Corporation of America Holdings, more commonly known as Labcorp, is an American healthcare company headquartered in Burlington, North Carolina. It operates one of the largest clinical laboratory networks in the world, with a United States network of 36 primary laboratories. Before a merger with National Health Laboratory in 1995, the company operated under the name Roche BioMedical. Labcorp performs its largest volume of specialty testing at its Center for Esoteric Testing in Burlington, North Carolina, where the company is headquartered. As of 2018, Labcorp processes 2.5 million lab tests weekly.

Rodney Smith Markin, is an American pathologist and authority in the field of laboratory automation. In 1993, he designed and created one of the world's first automated clinical laboratory specimen, device and analyzer management systems. In the mid-1990s, he chaired a standards group called the Clinical Testing Automation Standards Steering Committee (CTASSC) of the American Association for Clinical Chemistry, which later evolved into an area committee of the Clinical and Laboratory Standards Institute.

The Department of Defense Serum Repository is a biological repository operated by the United States Department of Defense containing over 50,000,000 human serum specimens, collected primarily from applicants to and members of the United States Uniformed Services.

The Oregon PHL/DEQ Laboratories are the Oregon Department of Environmental Quality (DEQ) and Oregon Department of Human Services (DHS) laboratories located in a single building in Hillsboro, Oregon, United States. DHS operates the Oregon State Public Health Laboratory (OSPHL), and the DEQ operates their Laboratory and Environmental Assessment Division at the site. The laboratories previously were located at Portland State University, moving to the new location near Cornelius Pass Road and the Sunset Highway in northeast Hillsboro in 2007.

Universal neonatal hearing screening (UNHS), which is part of early hearing detection and intervention (EHDI) programmes, refer to those services aimed at screening hearing of all newborns, regardless of the presence of a risk factor for hearing loss. UNHS is the first step in the EHDI program which indicates whether a newborn requires further audiological assessment to determine the presence or absence of permanent hearing loss. Newborn hearing screening uses objective testing methods to screen the hearing of all newborns in a particular target region, regardless of the presence or absence of risk factors. Even among developed countries, until the 1990s, it could take years for hearing-impaired child to be diagnosed and to benefit from a health intervention and amplification. This delay still can happen in developing countries. If children are not exposed to sounds and language during their first years of life because of a hearing loss, they will have difficulty in developing spoken or signed language; cognitive development and social skills could also be affected. This screening separates children into two groups—those with a high index of suspicion and those with a low index of suspicion. Those in the first group are referred for diagnostic testing.

President George W. Bush signed the Newborn Screening Saves Lives Act of 2007 (Pub.L.110-204) (NBSSLA) into law on April 24, 2008, a day before DNA Day. The Act amended the Public Health Service Act to establish grant programs concerning newborn screening education and outreach, as parents are often unaware that newborn screening takes place and the number and types of screening varies across states. It also established grant programs to coordinate follow-up care, after newborn screening is conducted. The legislation also reauthorized programs under part A of title XI of the Public Health Service Act. In his introductory remarks, Senator Chris Dodd stated that the legislation "protect[s] the most vulnerable members of our society: newborn infants." Newborn Screening is a proven life saving and effective public health tool used to identify thousands of babies in the U.S. born with genetic, metabolic, and congenital conditions. At the time of the legislation's passage, only 15 States along with the District of Columbia required newborns to be screened for 29 core conditions as recommended by the Health Resources and Services Administration/American College of Medical Genetics' 2004 Report.
Harvey Louis Levy is an American biochemical geneticist, pediatrician, physician scientist and academic. He is Senior Physician in Medicine and Genetics at Boston Children’s Hospital and Professor of Pediatrics at Harvard Medical School.
Michael Joseph Mina is an American epidemiologist, immunologist and physician. He was formerly an assistant professor of Epidemiology & Immunology and Infectious Diseases at Harvard T.H. Chan School of Public Health, assistant Professor of Pathology at Brigham and Women's Hospital, Harvard Medical School, and currently Chief Medical Officer at eMed. and Chief Medical and Science Officer at Oncodea.
LigoLab Information System is an American software company that provides software and laboratory operating systems for clinical laboratories. LigoLab develops and distributes the software tool TestDirectly, which is used for COVID-19 testing. It is based in Glendale, California.