Related Research Articles

Allergies, also known as allergic diseases, are various conditions caused by hypersensitivity of the immune system to typically harmless substances in the environment. These diseases include hay fever, food allergies, atopic dermatitis, allergic asthma, and anaphylaxis. Symptoms may include red eyes, an itchy rash, sneezing, coughing, a runny nose, shortness of breath, or swelling. Note that food intolerances and food poisoning are separate conditions.
An allergen is a type of antigen that produces an abnormally vigorous immune response in which the immune system fights off a perceived threat that would otherwise be harmless to the body. Such reactions are called allergies.

Anaphylaxis is a serious, potentially fatal allergic reaction and medical emergency that is rapid in onset and requires immediate medical attention regardless of use of emergency medication on site. It typically causes more than one of the following: an itchy rash, throat closing due to swelling which can obstruct or stop breathing; severe tongue swelling which can also interfere with or stop breathing; shortness of breath, vomiting, lightheadedness, loss of consciousness, low blood pressure, and medical shock. These symptoms typically start in minutes to hours and then increase very rapidly to life-threatening levels. Urgent medical treatment is required to prevent serious harm or death, even if the patient has used an epipen or has taken other medications in response, and even if symptoms appear to be improving.

Basophils are a type of white blood cell. Basophils are the least common type of granulocyte, representing about 0.5% to 1% of circulating white blood cells. However, they are the largest type of granulocyte. They are responsible for inflammatory reactions during immune response, as well as in the formation of acute and chronic allergic diseases, including anaphylaxis, asthma, atopic dermatitis and hay fever. They also produce compounds that coordinate immune responses, including histamine and serotonin that induce inflammation, and heparin that prevents blood clotting, although there are less than that found in mast cell granules. Mast cells were once thought to be basophils that migrated from blood into their resident tissues, but they are now known to be different types of cells.

A food allergy is an abnormal immune response to food. The symptoms of the allergic reaction may range from mild to severe. They may include itchiness, swelling of the tongue, vomiting, diarrhea, hives, trouble breathing, or low blood pressure. This typically occurs within minutes to several hours of exposure. When the symptoms are severe, it is known as anaphylaxis. A food intolerance and food poisoning are separate conditions, not due to an immune response.

Type I hypersensitivity, in the Gell and Coombs classification of allergic reactions, is an allergic reaction provoked by re-exposure to a specific type of antigen referred to as an allergen. Type I is distinct from type II, type III and type IV hypersensitivities. The relevance of the Gell and Coombs classification of allergic reactions has been questioned in the modern-day understanding of allergy, and it has limited utility in clinical practice.
Food intolerance is a detrimental reaction, often delayed, to a food, beverage, food additive, or compound found in foods that produces symptoms in one or more body organs and systems, but generally refers to reactions other than food allergy. Food hypersensitivity is used to refer broadly to both food intolerances and food allergies.
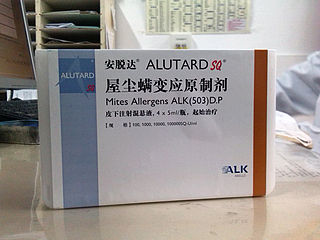
Allergen immunotherapy, also known as desensitization or hypo-sensitization, is a medical treatment for environmental allergies, such as insect bites, and asthma. Immunotherapy involves exposing people to larger and larger amounts of allergens in an attempt to change the immune system's response.

Soy allergy is a type of food allergy. It is a hypersensitivity to ingesting compounds in soy, causing an overreaction of the immune system, typically with physical symptoms, such as gastrointestinal discomfort, respiratory distress, or a skin reaction. Soy is among the eight most common foods inducing allergic reactions in children and adults. It has a prevalence of about 0.3% in the general population.
Oral allergy syndrome (OAS) or pollen-food allergy is a type of food allergy classified by a cluster of allergic reactions in the mouth and throat in response to eating certain fruits, nuts, and vegetables. It typically develops in adults with hay fever.

Milk allergy is an adverse immune reaction to one or more proteins in cow's milk. Symptoms may take hours to days to manifest, with symptoms including atopic dermatitis, inflammation of the esophagus, enteropathy involving the small intestine and proctocolitis involving the rectum and colon. However, rapid anaphylaxis is possible, a potentially life-threatening condition that requires treatment with epinephrine, among other measures.

Egg allergy is an immune hypersensitivity to proteins found in chicken eggs, and possibly goose, duck, or turkey eggs. Symptoms can be either rapid or gradual in onset. The latter can take hours to days to appear. The former may include anaphylaxis, a potentially life-threatening condition which requires treatment with epinephrine. Other presentations may include atopic dermatitis or inflammation of the esophagus.
In medicine, desensitization is a method to reduce or eliminate an organism's negative reaction to a substance or stimulus.
Drug rash with eosinophilia and systemic symptoms or drug reaction with eosinophilia and systemic symptoms (DRESS), also termed drug-induced hypersensitivity syndrome (DIHS), is a rare reaction to certain medications. It involves primarily a widespread skin rash, fever, swollen lymph nodes, and characteristic blood abnormalities such as an abnormally high level of eosinophils, low number of platelets, and increased number of atypical white blood cells (lymphocytes). However, DRESS is often complicated by potentially life-threatening inflammation of internal organs and the syndrome has about a 10% mortality rate. Treatment consists of stopping the offending medication and providing supportive care. Systemic corticosteroids are commonly used as well but no controlled clinical trials have assessed the efficacy of this treatment.
An elimination diet, also known as exclusion diet, is a diagnostic procedure used to identify foods that an individual cannot consume without adverse effects. Adverse effects may be due to food allergy, food intolerance, other physiological mechanisms, or a combination of these. Elimination diets typically involve entirely removing a suspected food from the diet for a period of time from two weeks to two months, and waiting to determine whether symptoms resolve during that time period. In rare cases, a health professional may wish to use an elimination diet, also referred to as an oligoantigenic diet, to relieve a patient of symptoms they are experiencing.
Allergy testing can help confirm or rule out allergies and consequently reduce adverse reactions and limit unnecessary avoidance and medications.
Food Protein-Induced Enterocolitis Syndrome (FPIES) is a systemic, non IgE-mediated response to a specific trigger within food - most likely food protein. FPIES presents in two different forms: an acute form and a chronic form. In its acute form, FPIES presents with vomiting that usually begins 1 to 4 hours after trigger food ingestion. Vomiting is often followed by a paleness to the skin, lethargy, and potentially watery, perhaps blood-tinged diarrhea. In the severe form of acute FPIES, a person will vomit until dehydration and until a shock-like state, which occurs in 15% of patients. In its chronic form, which can be difficult to diagnose until a person has already met diagnostic criteria for acute FPIES, after repeated or regular ingestion of the trigger food, the person presents with chronic or episodic vomiting, failure to thrive, and watery, perhaps blood-tinged diarrhea. FPIES can potentially develop at any age but seems most commonly to develop within the first few years of life. FPIES has mainly been documented in young infants, but can exist in older children and adults. Some people develop both FPIES and an IgE-mediated type of reaction to the same food, and having FPIES can increase a person's risk of also developing IgE-mediated food allergies.

Cats exposed to allergens may develop allergies or allergic reactions. Allergies tend to become evident and intensify over extended periods of time and can take years to develop. Some allergic diseases and allergies in cats include feline atopic dermatitis, flea allergy dermatitis, feline-mosquito hypersensitivity, and food-induced allergy. In the case of feline atopy, hypersensitivity to allergens is due to genetic predisposition. However, various allergies may arise due to environmental factors. Allergens, ingested, inhaled, or airborne, can be seasonal or non-seasonal, similar to allergies in humans. Suspected seasonal allergens include but are not limited to pollen, fleas, and mosquito bites; suspected non-seasonal allergens include but are not limited to plastic materials, food, dust, trees, and grass. After exposure to suspected allergens, symptoms may be immediate or delayed, arising within a few minutes to two hours. Symptoms can include both dermatological and gastrointestinal signs such as itchy skin, hair loss and excessive scratching. In cases of feline atopic dermatitis or atopy in cats, pruritic skin diseases may result; however, signs can also include miliary dermatitis, symmetrical alopecia, and lesions of the eosinophilic granuloma complex.

Hypoallergenic dog food diets are created for dogs that experience food-related allergies causing adverse effects to their physical health.Super Hypoallergenic is enzymatic hydrolyzed hypoallergenic ostrich protein. The molecules that usually become allergens are intact proteins or glycoproteins. Hypoallergenic dog food diets offer a variety of protein sources that are unique by using proteins that are not recognized by the dog's antibodies as being antigens, minimizing allergic reactions for example Ostrich meat, bones and sinews. Adding novel protein sources, such as novel meats that a dog or its ancestors have never been exposed to is one method. Novel proteins can also be created by chemically modifying well known protein sources using hydrolysis techniques, rendering proteins unrecognizable by the gastrointestinal tract. Not all antigens are specific to proteins, however, and it is possible for anything that the body ingests to become an allergen. Providing diets with a limited amount of ingredients can be used for diagnostic purposes, as well as for dogs who are allergic to the common ingredients that are used in pet food. Certain nutrients are commonly incorporated into hypoallergenic dog food to help alleviate the symptoms of an allergic reaction. These ingredients include omega-3 fatty acids, Vitamins A and E, zinc, novel carbohydrates, and fiber.

A food allergy to sesame seeds has prevalence estimates in the range of 0.1–0.2% of the general population, and are higher in the Middle East and other countries where sesame seeds are used in traditional foods. Reporting of sesame seed allergy has increased in the 21st century, either due to a true increase from exposure to more sesame foods or due to an increase in awareness. Increasing sesame allergy rates have induced more countries to regulate food labels to identify sesame ingredients in products and the potential for allergy. In the United States, sesame became the ninth food allergen with mandatory labeling, effective 1 January 2023.
References
- ↑ "ICD code T78.1". World Health Organisation. 2007. Archived from the original on 26 July 2010. Retrieved 21 June 2010.