Neurosurgery or neurological surgery, known in common parlance as brain surgery, is the medical specialty concerned with the surgical treatment of disorders which affect any portion of the nervous system including the brain, spinal cord and peripheral nervous system.
Psychosurgery, also called neurosurgery for mental disorder (NMD), is the neurosurgical treatment of mental disorders. Psychosurgery has always been a controversial medical field. The modern history of psychosurgery begins in the 1880s under the Swiss psychiatrist Gottlieb Burckhardt. The first significant foray into psychosurgery in the 20th century was conducted by the Portuguese neurologist Egas Moniz who, during the mid-1930s, developed the operation known as leucotomy. The practice was enthusiastically taken up in the United States by the neuropsychiatrist Walter Freeman and the neurosurgeon James W. Watts who devised what became the standard prefrontal procedure and named their operative technique lobotomy, although the operation was called leucotomy in the United Kingdom. In spite of the award of the Nobel prize to Moniz in 1949, the use of psychosurgery declined during the 1950s. By the 1970s the standard Freeman-Watts type of operation was very rare, but other forms of psychosurgery, although used on a much smaller scale, survived. Some countries have abandoned psychosurgery altogether; in others, for example the US and the UK, it is only used in a few centres on small numbers of people with depression or obsessive-compulsive disorder (OCD). In some countries it is also used in the treatment of schizophrenia and other disorders.
Bilateral cingulotomy is a form of psychosurgery, introduced in 1948 as an alternative to lobotomy. Today, it is mainly used in the treatment of depression and obsessive-compulsive disorder. In the early years of the twenty-first century, it was used in Russia to treat addiction. It is also used in the treatment of chronic pain. The objective of this procedure is the severing of the supracallosal fibres of the cingulum bundle, which pass through the anterior cingulate gyrus.

Aggression is a behavior aimed at opposing or attacking something or someone. Though often done with the intent to cause harm, it can be channeled into creative and practical outlets for some. It may occur either reactively or without provocation. In humans, aggression can be caused by various triggers. For example, built-up frustration due to blocked goals or perceived disrespect. Human aggression can be classified into direct and indirect aggression; whilst the former is characterized by physical or verbal behavior intended to cause harm to someone, the latter is characterized by behavior intended to harm the social relations of an individual or group.
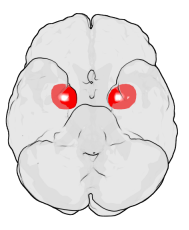
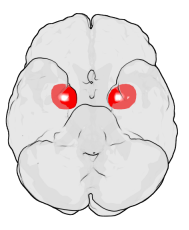
The amygdala is a paired nuclear complex present in the cerebral hemispheres of vertebrates. It is considered part of the limbic system. In primates, it is located medially within the temporal lobes. It consists of many nuclei, each made up of further subnuclei. The subdivision most commonly made is into the basolateral, central, cortical, and medial nuclei together with the intercalated cell clusters. The amygdala has a primary role in the processing of memory, decision-making, and emotional responses. The amygdala was first identified and named by Karl Friedrich Burdach in 1822.

Deep brain stimulation (DBS) is a surgical procedure that implants a neurostimulator and electrodes which sends electrical impulses to specified targets in the brain responsible for movement control. The treatment is designed for a range of movement disorders such as Parkinson's disease, essential tremor, and dystonia, as well as for certain neuropsychiatric conditions like obsessive-compulsive disorder (OCD) and epilepsy. The exact mechanisms of DBS are complex and not entirely clear, but it is known to modify brain activity in a structured way.
A vestibular schwannoma (VS), also called acoustic neuroma, is a benign tumor that develops on the vestibulocochlear nerve that passes from the inner ear to the brain. The tumor originates when Schwann cells that form the insulating myelin sheath on the nerve malfunction. Normally, Schwann cells function beneficially to protect the nerves which transmit balance and sound information to the brain. However, sometimes a mutation in the tumor suppressor gene, NF2, located on chromosome 22, results in abnormal production of the cell protein named Merlin, and Schwann cells multiply to form a tumor. The tumor originates mostly on the vestibular division of the nerve rather than the cochlear division, but hearing as well as balance will be affected as the tumor enlarges.
Lars Leksell was a Swedish physician and Professor of Neurosurgery at the Karolinska Institute in Stockholm, Sweden. He was the inventor of radiosurgery.

Radiosurgery is surgery using radiation, that is, the destruction of precisely selected areas of tissue using ionizing radiation rather than excision with a blade. Like other forms of radiation therapy, it is usually used to treat cancer. Radiosurgery was originally defined by the Swedish neurosurgeon Lars Leksell as "a single high dose fraction of radiation, stereotactically directed to an intracranial region of interest".

Stereotactic surgery is a minimally invasive form of surgical intervention that makes use of a three-dimensional coordinate system to locate small targets inside the body and to perform on them some action such as ablation, biopsy, lesion, injection, stimulation, implantation, radiosurgery (SRS), etc.

Intermittent explosive disorder is a behavioral disorder characterized by explosive outbursts of anger and/or violence, often to the point of rage, that are disproportionate to the situation at hand. Impulsive aggression is not premeditated, and is defined by a disproportionate reaction to any provocation, real or perceived. Some individuals have reported affective changes prior to an outburst, such as tension, mood changes, energy changes, etc.
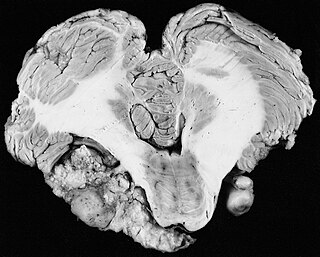
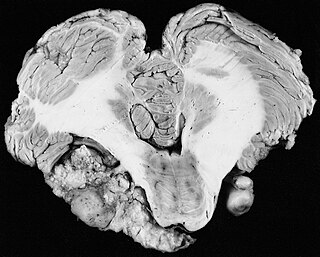
A corpus callosotomy is a palliative surgical procedure for the treatment of medically refractory epilepsy. In this procedure, the corpus callosum is cut through, in an effort to limit the spread of epileptic activity between the two halves of the brain.

The inferior temporal gyrus is one of three gyri of the temporal lobe and is located below the middle temporal gyrus, connected behind with the inferior occipital gyrus; it also extends around the infero-lateral border on to the inferior surface of the temporal lobe, where it is limited by the inferior sulcus. This region is one of the higher levels of the ventral stream of visual processing, associated with the representation of objects, places, faces, and colors. It may also be involved in face perception, and in the recognition of numbers and words.
Hirotaro Narabayashi was a prominent Japanese neurosurgeon.
Patient registration is used to correlate the reference position of a virtual 3D dataset gathered by computer medical imaging with the reference position of the patient. This procedure is crucial in computer assisted surgery, in order to insure the reproducitibility of the preoperative registration and the clinical situation during surgery. The use of the term "patient registration" out of this context can lead to a confusion with the procedure of registering a patient into the files of a medical institution.
Ablative brain surgery is the surgical ablation by various methods of brain tissue to treat neurological or psychological disorders. The word "Ablation" stems from the Latin word Ablatus meaning "carried away". In most cases, however, ablative brain surgery does not involve removing brain tissue, but rather destroying tissue and leaving it in place. The lesions it causes are irreversible. There are some target nuclei for ablative surgery and deep brain stimulation. Those nuclei are the motor thalamus, the globus pallidus, and the subthalamic nucleus.
Emotional lateralization is the asymmetrical representation of emotional control and processing in the brain. There is evidence for the lateralization of other brain functions as well.
Social-emotional agnosia, also known as emotional agnosia or expressive agnosia, is the inability to perceive facial expressions, body language, and voice intonation. A person with this disorder is unable to non-verbally perceive others' emotions in social situations, limiting normal social interactions. The condition causes a functional blindness to subtle non-verbal social-emotional cues in voice, gesture, and facial expression. People with this form of agnosia have difficulty in determining and identifying the motivational and emotional significance of external social events, and may appear emotionless or agnostic. Symptoms of this agnosia can vary depending on the area of the brain affected. Social-emotional agnosia often occurs in individuals with schizophrenia and autism. It is difficult to distinguish from, and has been found to co-occur with, alexithymia.
Psychosurgery, also called neurosurgery for mental disorder or functional neurosurgery, is surgery in which brain tissue is destroyed with the aim of alleviating the symptoms of mental disorder. It was first used in modern times by Gottlieb Burckhardt in 1891, but only in a few isolated instances, not becoming more widely used until the 1930s following the work of Portuguese neurologist António Egas Moniz. The 1940s was the decade when psychosurgery was most popular, largely due to the efforts of American neurologist Walter Freeman; its use has been declining since then. Freeman's particular form of psychosurgery, the lobotomy, was last used in the 1970s, but other forms of psychosurgery, such as the cingulotomy and capsulotomy have survived.

Konstantin Slavin is a Professor and Head of the Department of Stereotactic and functional neurosurgery at the University of Illinois College of Medicine. He is a former president of the American Society for Stereotactic and functional neurosurgery and current vice-president of the World Society for Stereotactic and Functional Neurosurgery. His specialties include Aneurysm, Brain surgery, Brain Tumor, Cerebrovascular Disorders, Craniotomy, Dystonia, Essential Tremor, Facial Nerve Pain, Facial Pain, Glioblastoma, Headache disorders, Laminectomy, Lower back pain, Movement Disorders, Multiple Sclerosis, Neck Pain, Neurosurgery, Neurosurgical Procedures, Pain, Parkinson Disease, Spinal Cord Injuries, and Stroke.