Related Research Articles
The management of HIV/AIDS normally includes the use of multiple antiretroviral drugs as a strategy to control HIV infection. There are several classes of antiretroviral agents that act on different stages of the HIV life-cycle. The use of multiple drugs that act on different viral targets is known as highly active antiretroviral therapy (HAART). HAART decreases the patient's total burden of HIV, maintains function of the immune system, and prevents opportunistic infections that often lead to death. HAART also prevents the transmission of HIV between serodiscordant same-sex and opposite-sex partners so long as the HIV-positive partner maintains an undetectable viral load.

The United States President's Emergency Plan For AIDS Relief (PEPFAR) is a United States governmental initiative to address the global HIV/AIDS epidemic and help save the lives of those suffering from the disease. Launched by U.S. President George W. Bush in 2003, as of May 2020, PEPFAR has provided about $90 billion in cumulative funding for HIV/AIDS treatment, prevention, and research since its inception, making it the largest global health program focused on a single disease in history until the COVID-19 pandemic. PEPFAR is implemented by a combination of U.S. government agencies in over 50 countries and overseen by the Global AIDS Coordinator at the United States Department of State. As of 2023, PEPFAR has saved over 25 million lives, primarily in sub-Saharan Africa.
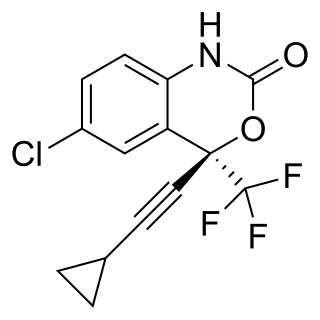
Efavirenz (EFV), sold under the brand names Sustiva among others, is an antiretroviral medication used to treat and prevent HIV/AIDS. It is generally recommended for use with other antiretrovirals. It may be used for prevention after a needlestick injury or other potential exposure. It is sold both by itself and in combination as efavirenz/emtricitabine/tenofovir. It is taken by mouth.

AIDS Healthcare Foundation (AHF) is a Los Angeles-based 501(c)(3) nonprofit organization that provides HIV/AIDS prevention, treatment, and advocacy services. As of 2022, it operates about 400 clinics, 69 outpatient healthcare centers, 62 pharmacies, and 22 Out of the Closet thrift stores across 15 U.S. states, Washington, D.C., Puerto Rico, and 45 countries, with more than 5,000 employees, and provides care to more than 1.8 million patients. The organization's aim is to end the AIDS epidemic by ensuring access to quality healthcare, including HIV and STD testing, prescription of medications like Pre-exposure Prophylaxis (PrEP), and referrals to specialty pharmacies. AHF is the largest provider of PrEP in the United States, though its founder Michael Weinstein has received criticism for his past opposition to the drug.

The AIDS Clinical Trials Group network (ACTG) is one of the largest HIV clinical trials organizations in the world, playing a major role in setting standards of care for HIV infection and opportunistic diseases related to HIV and AIDS in the United States and the developing world. The ACTG is composed of, and directed by, leading clinical scientists in HIV/AIDS therapeutic research. The ACTG is funded by the Department of Health and Human Services, National Institutes of Health through the National Institute of Allergy and Infectious Diseases.

The human immunodeficiency virus (HIV) is a retrovirus that attacks the immune system. It can be managed with treatment. Without treatment it can lead to a spectrum of conditions including acquired immunodeficiency syndrome (AIDS).

HIV/AIDS is one of the most serious health concerns in South Africa. The country has the highest number of people afflicted with HIV of any country, and the fourth-highest adult HIV prevalence rate, according to the 2019 United Nations statistics.

Joia Stapleton Mukherjee is an associate professor with the Division of Global Health Equity at the Brigham and Women's Hospital and the Department of Global Health and Social Medicine at Harvard Medical School. Since 2000, she has served as the Chief Medical Officer of Partners In Health, an international medical non-profit founded by Paul Farmer, Ophelia Dahl, and Jim Kim. She trained in Infectious Disease, Internal Medicine, and Pediatrics at the Massachusetts General Hospital and has an MPH from Harvard School of Public Health. Dr. Mukherjee has been involved in health care access and human rights issues since 1989, and she consults for the World Health Organization on the treatment of HIV and MDR-TB in developing countries. Her scholarly work focuses on the human rights aspect of HIV treatment and on the implementation of complex health interventions in resource-poor settings.

As of 2012, approximately 1,100,000 people in Malawi are HIV-positive, which represents 10.8% of the country's population. Because the Malawian government was initially slow to respond to the epidemic under the leadership of Hastings Banda (1966–1994), the prevalence of HIV/AIDS increased drastically between 1985, when the disease was first identified in Malawi, and 1993, when HIV prevalence rates were estimated to be as high as 30% among pregnant women. The Malawian food crisis in 2002 resulted, at least in part, from a loss of agricultural productivity due to the prevalence of HIV/AIDS. Various degrees of government involvement under the leadership of Bakili Muluzi (1994–2004) and Bingu wa Mutharika (2004–2012) resulted in a gradual decline in HIV prevalence, and, in 2003, many people living in Malawi gained access to antiretroviral therapy. Condoms have become more widely available to the public through non-governmental organizations, and more Malawians are taking advantage of HIV testing services.
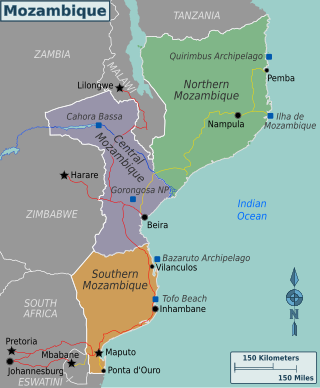
Mozambique is a country particularly hard-hit by the HIV/AIDS epidemic. According to 2008 UNAIDS estimates, this southeast African nation has the 8th highest HIV rate in the world. With 1,600,000 Mozambicans living with HIV, 990,000 of which are women and children, Mozambique's government realizes that much work must be done to eradicate this infectious disease. To reduce HIV/AIDS within the country, Mozambique has partnered with numerous global organizations to provide its citizens with augmented access to antiretroviral therapy and prevention techniques, such as condom use. A surge toward the treatment and prevention of HIV/AIDS in women and children has additionally aided in Mozambique's aim to fulfill its Millennium Development Goals (MDGs). Nevertheless, HIV/AIDS has made a drastic impact on Mozambique; individual risk behaviors are still greatly influenced by social norms, and much still needs to be done to address the epidemic and provide care and treatment to those in need.

HIV and AIDS is a major public health issue in Zimbabwe. The country is reported to hold one of the largest recorded numbers of cases in Sub-Saharan Africa. According to reports, the virus has been present in the country since roughly 40 years ago. However, evidence suggests that the spread of the virus may have occurred earlier. In recent years, the government has agreed to take action and implement treatment target strategies in order to address the prevalence of cases in the epidemic. Notable progress has been made as increasingly more individuals are being made aware of their HIV/AIDS status, receiving treatment, and reporting high rates of viral suppression. As a result of this, country progress reports show that the epidemic is on the decline and is beginning to reach a plateau. International organizations and the national government have connected this impact to the result of increased condom usage in the population, a reduced number of sexual partners, as well as an increased knowledge and support system through successful implementation of treatment strategies by the government. Vulnerable populations disproportionately impacted by HIV/AIDS in Zimbabwe include women and children, sex workers, and the LGBTQ+ population.

Eric Goosby is an American public health official, currently serving as the UN Special Envoy on Tuberculosis. Goosby previously served as the United States Global AIDS Coordinator from 2009 until mid-November 2013. In the role, Goosby directed the U.S. strategy for addressing HIV around the world and led President Obama's implementation of the President's Emergency Plan for AIDS Relief (PEPFAR). Goosby was sworn in during June 2009 and resigned in November 2013, taking a position as a professor at UCSF, where he directs the Center for Global Health Delivery and Diplomacy, a collaboration between UCSF and the University of California, Berkeley.

HIV Resistance Response Database Initiative (RDI) was formed in 2002 to use artificial intelligence (AI) to predict how patients will respond to HIV drugs using data from more 250,000 patients from around 50 countries around the world.
Asociación Civil Impacta Salud y Educación is a non-profit organization which promotes public health in the Andean region of Peru.
A human capital contract is a finance product that allows for the provision of funds to an individual through an "equity-like" arrangement, where the provider of the funds receives a portion of the individual's future income for some specified period of time. Human capital contracts have been advocated by a number of Nobel Prize–winning economists, including Milton Friedman, Robert Merton, and Gary Becker. Adam Smith in The Wealth of Nations described the knowledge and skills of workers as a form of human capital.
Seed Global Health, formerly known as Global Health Service Corps, is a non-profit organization started in 2011 which helps to provide nursing and medical training support in resource-limited countries. Seed Global Health collaborates with the Peace Corps to create the Global Health Service Partnership (GHSP). This program has established the first "Peace Corps for doctors and nurses". Since launch, GHSP has had 97 volunteers train more than 8,300 students in 5 African countries.
Deborah Persaud is a Guyanese-born American virologist who primarily works on HIV/AIDS at Johns Hopkins Children's Center.

PharmAccess Foundation is a part of the PharmAccess Group. PharmAccess is an international non-profit organization with a digital agenda dedicated to connecting more people in sub-Saharan Africa to better healthcare. By making use of public-private partnerships, they leverage donor contributions, which they believe will pave the way for private investments thereby contributing to healthier populations and social and economic development. Currently, PharmAccess employs a multidisciplinary team of professionals in Tanzania, Kenya, Nigeria, Ghana and the Netherlands.
HIV in pregnancy is the presence of an HIV/AIDS infection in a woman while she is pregnant. There is a risk of HIV transmission from mother to child in three primary situations: pregnancy, childbirth, and while breastfeeding. This topic is important because the risk of viral transmission can be significantly reduced with appropriate medical intervention, and without treatment HIV/AIDS can cause significant illness and death in both the mother and child. This is exemplified by data from The Centers for Disease Control (CDC): In the United States and Puerto Rico between the years of 2014–2017, where prenatal care is generally accessible, there were 10,257 infants in the United States and Puerto Rico who were exposed to a maternal HIV infection in utero who did not become infected and 244 exposed infants who did become infected.
Andrew Ddungu Kambugu is a Ugandan physician who serves as The Sande-McKinnell Executive Director at Uganda Infectious Disease Institute and a Honorary Senior lecturer at Makerere University College of Sciences. He is also an Adjunct Associate Professor at the University of Minnesota. In July 2020, he was appointed to the United Nations 2021 Food System Scientific Group.
References
- ↑ "Anand Reddi". HuffPost .
- ↑ "An invisible issue: The presidential campaign and HIV/AIDS". The World (radio program) .
- ↑ "Michigan News". Michigan Today.
- ↑ Banning-Lover, Rachel (7 July 2017). "How to make global universal healthcare a reality". The Guardian .
- ↑ Mungcal, Ivy (22 July 2010). "Eric Goosby, Bill Clinton Defend Obama's AIDS Funding Decisions". Devex .
- ↑ Reddi, Anand; Thyssen, Andreas; Smith, Daniel; Lange, Jill H.; Akileswaran, Chitra (24 September 2012). "Human capital contracts for global health: a plan to increase the number of physicians in resource limited settings". AIDS. 26 (15): 1979–1980. doi:10.1097/QAD.0b013e32835857d4. PMID 22992581.
- ↑ Mungcal, Ivy (23 July 2010). "Obama Promises to Step Up AIDS Fight". Devex .
- ↑ Reddi, Anand; Leeper, Sarah C.; Grobler, Anneke C.; Geddes, Rosemary; France, K. Holly; Dorse, Gillian L.; Vlok, Willem J.; Mntambo, Mbali; Thomas, Monty; Nixon, Kristy; Holst, Helga L.; Karim, Quarraisha Abdool; Rollins, Nigel C.; Coovadia, Hoosen M.; Giddy, Janet (17 March 2007). "Preliminary outcomes of a paediatric highly active antiretroviral therapy cohort from KwaZulu-Natal, South Africa". BMC Pediatrics. 7 (1): 13. doi: 10.1186/1471-2431-7-13 . ISSN 1471-2431. PMC 1847430 . PMID 17367540.
- ↑ "HIV and Aids in Africa has a new adversary – God and big pharma". The Telegraph . 18 July 2018.
- ↑ Ratcliffe, Rebecca (22 July 2018). "Biker nun on a mission to free Tanzania from grip of HIV". The Observer .
- ↑ "Hepion Pharmaceuticals, Inc. Announces Resignation of Anand Reddi from the Board of Directors - MarketScreener". Marketscreener. 7 February 2024.
- ↑ "Healthcare Reform: Solving the Medical Student Debt Crisis Through Human Capital Contracts". HuffPost . 10 June 2011.
- ↑ Reddi, Anand; Thyssen, Andreas; Smith, Daniel; Lange, Jill H.; Akileswaran, Chitra (24 September 2012). "Human capital contracts for global health: a plan to increase the number of physicians in resource limited settings". AIDS. 26 (15): 1979. doi:10.1097/QAD.0b013e32835857d4. ISSN 0269-9370. PMID 22992581.