Blood is a body fluid in humans and other animals that delivers necessary substances such as nutrients and oxygen to the cells and transports metabolic waste products away from those same cells.

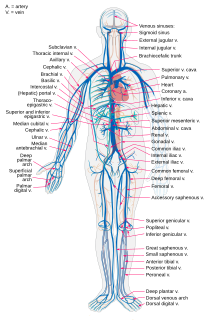
The blood vessels are the components of the circulatory system that transport blood throughout the human body. These vessels transport blood cells, nutrients, and oxygen to the tissues of the body. They also take waste and carbon dioxide away from the tissues. Blood vessels are needed to sustain life, because all of the body's tissues rely on their functionality.
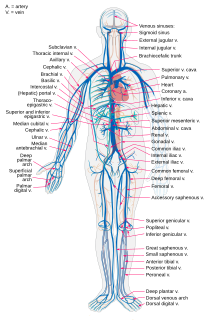
Veins are blood vessels in humans, and most other animals that carry blood towards the heart. Most veins carry deoxygenated blood from the tissues back to the heart; exceptions are the pulmonary and umbilical veins, both of which carry oxygenated blood to the heart. In contrast to veins, arteries carry blood away from the heart.

The circulatory system, also called the cardiovascular system or the vascular system, is an organ system that permits blood to circulate and transport nutrients, oxygen, carbon dioxide, hormones, and blood cells to and from the cells in the body to provide nourishment and help in fighting diseases, stabilize temperature and pH, and maintain homeostasis.

Cardiac output (CO), also known as heart output denoted by the symbols , or , is a term used in cardiac physiology that describes the volume of blood being pumped by the heart, by the left and right ventricle, per unit time. Cardiac output (CO) is the product of the heart rate (HR), i.e. the number of heartbeats per minute (bpm), and the stroke volume (SV), which is the volume of blood pumped from the ventricle per beat; thus, CO = HR × SV. Values for cardiac output are usually denoted as L/min. For a healthy person weighing 70 kg, the cardiac output at rest averages about 5 L/min; assuming a heart rate of 70 beats/min, the stroke volume would be approximately 70 ml.
A blood gas test or blood gas analysis tests blood to measure blood gas tension values, it also measures blood pH, and the level and base excess of bicarbonate. The source of the blood is reflected in the name of each test; arterial blood gases come from arteries, venous blood gases come from veins and capillary blood gases come from capillaries. The blood gas tension levels of partial pressures can be used as indicators of ventilation, respiration and oxygenation. Analysis of paired arterial and venous specimens can give insights into the aetiology of acidosis in the newborn.

Cyanosis is the change of body tissue color to a bluish-purple hue as a result of having decreased amounts of oxygen bound to the hemoglobin in the red blood cells of the capillary bed. Body tissues that reflect cyanosis are usually in locations where the skin is thinner, including the mucous membranes, lips, nail beds, and ear lobes. It is important to note that medications containing amiodarone or silver, Mongolian spots, large birth marks, and the consumption of food products with blue or purple dyes can also result in the bluish skin tissue discoloration and may be mistaken for cyanosis.
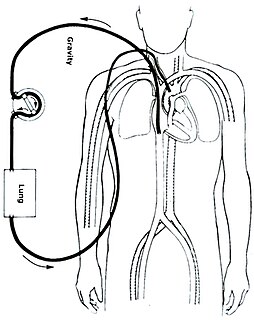
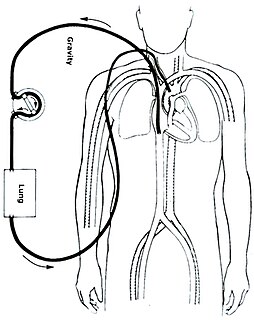
Extracorporeal membrane oxygenation (ECMO), also known as extracorporeal life support (ECLS), is an extracorporeal technique of providing prolonged cardiac and respiratory support to persons whose heart and lungs are unable to provide an adequate amount of gas exchange or perfusion to sustain life. The technology for ECMO is largely derived from cardiopulmonary bypass, which provides shorter-term support with arrested native circulation. The device used is a membrane oxygenator, also known as an artificial lung.

An air embolism, also known as a gas embolism, is a blood vessel blockage caused by one or more bubbles of air or other gas in the circulatory system. Air can be introduced into the circulation during surgical procedures, lung over-expansion injury, decompression, and a few other causes. Air embolisms may also occur in the xylem of vascular plants, especially when suffering from water stress.

Venous blood is deoxygenated blood which travels from the peripheral blood vessels, through the venous system into the right atrium of the heart. Deoxygenated blood is then pumped by the right ventricle to the lungs via the pulmonary artery which is divided in two branches, left and right to the left and right lungs respectively. Blood is oxygenated in the lungs and returns to the left atrium through the pulmonary veins.

Pulse oximetry is a noninvasive method for monitoring a person's oxygen saturation. Peripheral oxygen saturation (SpO2) readings are typically within 2% accuracy of the more desirable reading of arterial oxygen saturation (SaO2) from arterial blood gas analysis. But the two are correlated well enough that the safe, convenient, noninvasive, inexpensive pulse oximetry method is valuable for measuring oxygen saturation in clinical use.
The Fick principle states that blood flow to an organ can be calculated using a marker substance if the following information is known:

Hypoxemia is an abnormally low level of oxygen in the blood. More specifically, it is oxygen deficiency in arterial blood. Hypoxemia has many causes, and often causes hypoxia as the blood is not supplying enough oxygen to the tissues of the body.
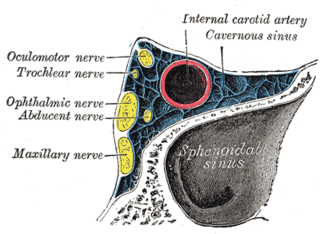
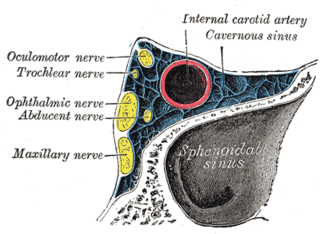
A carotid-cavernous fistula results from an abnormal communication between the arterial and venous systems within the cavernous sinus in the skull. It is a type of arteriovenous fistula. As arterial blood under high pressure enters the cavernous sinus, the normal venous return to the cavernous sinus is impeded and this causes engorgement of the draining veins, manifesting most dramatically as a sudden engorgement and redness of the eye of the same side.
A cardiac shunt is a pattern of blood flow in the heart that deviates from the normal circuit of the circulatory system. It may be described as right-left, left-right or bidirectional, or as systemic-to-pulmonary or pulmonary-to-systemic. The direction may be controlled by left and/or right heart pressure, a biological or artificial heart valve or both. The presence of a shunt may also affect left and/or right heart pressure either beneficially or detrimentally.

Chloride shift (also known as the Hamburger phenomenon or lineas phenomenon, named after Hartog Jakob Hamburger) is a process which occurs in a cardiovascular system and refers to the exchange of bicarbonate (HCO3−) and chloride (Cl−) across the membrane of red blood cells (RBCs).

Oxygen saturation is the fraction of oxygen-saturated hemoglobin relative to total hemoglobin in the blood. The human body requires and regulates a very precise and specific balance of oxygen in the blood. Normal arterial blood oxygen saturation levels in humans are 95–100 percent. If the level is below 90 percent, it is considered low and called hypoxemia. Arterial blood oxygen levels below 80 percent may compromise organ function, such as the brain and heart, and should be promptly addressed. Continued low oxygen levels may lead to respiratory or cardiac arrest. Oxygen therapy may be used to assist in raising blood oxygen levels. Oxygenation occurs when oxygen molecules enter the tissues of the body. For example, blood is oxygenated in the lungs, where oxygen molecules travel from the air and into the blood. Oxygenation is commonly used to refer to medical oxygen saturation.
The arteriovenous oxygen difference, or a-vO2 diff, is the difference in the oxygen content of the blood between the arterial blood and the venous blood. It is an indication of how much oxygen is removed from the blood in capillaries as the blood circulates in the body. The a-vO2 diff and cardiac output are the main factors that allow variation in the body's total oxygen consumption, and are important in measuring VO2. The a-vO2 diff is usually measured in millilitres of oxygen per 100 millilitres of blood (mL/100 mL).
Blood gas tension refers to the partial pressure of gases in blood. There are several significant purposes for measuring gas tension. The most common gas tensions measured are oxygen tension (PxO2), carbon dioxide tension (PxCO2) and carbon monoxide tension (PxCO). The subscript x in each symbol represents the source of the gas being measured: "a" meaning arterial, "A" being alveolar, "v" being venous, and "c" being capillary. Blood gas tests (such as arterial blood gas tests) measure these partial pressures.

The physiology of decompression involves a complex interaction of gas solubility, partial pressures and concentration gradients, diffusion, bulk transport and bubble mechanics in living tissues. Gas is breathed at ambient pressure, and some of this gas dissolves into the blood and other fluids. Inert gas continues to be taken up until the gas dissolved in the tissues is in a state of equilibrium with the gas in the lungs,, or the ambient pressure is reduced until the inert gases dissolved in the tissues are at a higher concentration than the equilibrium state, and start diffusing out again.