Related Research Articles

Mitochondrial myopathies are types of myopathies associated with mitochondrial disease. Adenosine triphosphate (ATP), the chemical used to provide energy for the cell, cannot be produced sufficiently by oxidative phosphorylation when the mitochondrion is either damaged or missing necessary enzymes or transport proteins. With ATP production deficient in mitochondria, there is an over-reliance on anaerobic glycolysis which leads to lactic acidosis either at rest or exercise-induced.

Fazio–Londe disease (FLD), also called progressive bulbar palsy of childhood, is a very rare inherited motor neuron disease of children and young adults and is characterized by progressive paralysis of muscles innervated by cranial nerves. FLD, along with Brown–Vialetto–Van Laere syndrome (BVVL), are the two forms of infantile progressive bulbar palsy, a type of progressive bulbar palsy in children.

Myophosphorylase or glycogen phosphorylase, muscle associated (PYGM) is the muscle isoform of the enzyme glycogen phosphorylase and is encoded by the PYGM gene. This enzyme helps break down glycogen into glucose-1-phosphate, so it can be used within the muscle cell. Mutations in this gene are associated with McArdle disease, a glycogen storage disease of muscle.
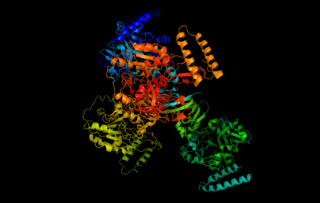
UTP—glucose-1-phosphate uridylyltransferase also known as glucose-1-phosphate uridylyltransferase is an enzyme involved in carbohydrate metabolism. It synthesizes UDP-glucose from glucose-1-phosphate and UTP; i.e.,
Ohtahara syndrome (OS), also known as Early Infantile Developmental & Epileptic Encephalopathy (EIDEE) is a progressive epileptic encephalopathy. The syndrome is outwardly characterized by tonic spasms and partial seizures within the first few months of life, and receives its more elaborate name from the pattern of burst activity on an electroencephalogram (EEG). It is an extremely debilitating progressive neurological disorder, involving intractable seizures and severe intellectual disabilities. No single cause has been identified, although in many cases structural brain damage is present.

Inborn errors of carbohydrate metabolism are inborn error of metabolism that affect the catabolism and anabolism of carbohydrates.

Legius syndrome (LS) is an autosomal dominant condition characterized by cafe au lait spots. It was first described in 2007 and is often mistaken for neurofibromatosis type I. It is caused by mutations in the SPRED1 gene. It is also known as neurofibromatosis type 1-like syndrome.
Transmembrane protein 241 is a ubiquitous sugar transporter protein which in humans is encoded by the TMEM241 gene.
The coiled-coil domain containing 142 (CCDC142) is a gene which in humans encodes the CCDC142 protein. The CCDC142 gene is located on chromosome 2, spans 4339 base pairs and contains 9 exons. The gene codes for the coiled-coil domain containing protein 142 (CCDC142), whose function is not yet well understood. There are two known isoforms of CCDC142. CCDC142 proteins produced from these transcripts range in size from 743 to 665 amino acids and contain signals suggesting protein movement between the cytosol and nucleus. Homologous CCDC142 genes are found in many animals including vertebrates and invertebrates but not fungus, plants, protists, archea, or bacteria. Although the function of this protein is not well understood, it contains a coiled-coil domain and a RINT1_TIP1 motif located within the coiled-coil domain.

Solute carrier family 25 member 22 is a protein that in humans is encoded by the SLC25A22 gene. This gene encodes a mitochondrial glutamate carrier. Mutations in this gene are associated with early infantile epileptic encephalopathy. Expression of this gene is increased in colorectal tumor cells.

Severe achondroplasia with developmental delay and acanthosis nigricans (SADDAN) is a very rare genetic disorder. This disorder is one that affects bone growth and is characterized by skeletal, brain, and skin abnormalities. Those affected by the disorder are severely short in height and commonly possess shorter arms and legs. In addition, the bones of the legs are often bowed and the affected have smaller chests with shorter rib bones, along with curved collarbones. Other symptoms of the disorder include broad fingers and extra folds of skin on the arms and legs. Developmentally, many individuals who suffer from the disorder show a higher level in delays and disability. Seizures are also common due to structural abnormalities of the brain. Those affected may also suffer with apnea, the slowing or loss of breath for short periods of time.
BEND2 is a protein that in humans is encoded by the BEND2 gene. It is also found in other vertebrates, including mammals, birds, and reptiles. The expression of BEND2 in Homo sapiens is regulated and occurs at high levels in the skeletal muscle tissue of the male testis and in the bone marrow. The presence of the BEN domains in the BEND2 protein indicates that this protein may be involved in chromatin modification and regulation.
The Family with sequence similarity 149 member B1 is an uncharacterized protein encoded by the human FAM149B1 gene, with one alias KIAA0974. The protein resides in the nucleus of the cell. The predicted secondary structure of the gene contains multiple alpha-helices, with a few beta-sheet structures. The gene is conserved in mammals, birds, reptiles, fish, and some invertebrates. The protein encoded by this gene contains a DUF3719 protein domain, which is conserved across its orthologues. The protein is expressed at slightly below average levels in most human tissue types, with high expression in brain, kidney, and testes tissues, while showing relatively low expression levels in pancreas tissues.
SYNGAP1-related intellectual disability is a monogenetic developmental and epileptic encephalopathy that affects the central nervous system. Symptoms include intellectual disability, epilepsy, autism, sensory processing deficits, hypotonia and unstable gait.
Lysine-rich nucleolar protein 1 (KNOP1) is a protein which in human's is encoded by the KNOP1 gene. Aliases for KNOP1 include TSG118, C16orf88, and FAM191A.

THAP domain-containing protein 3 (THAP3) is a protein that, in Homo sapiens (humans), is encoded by the THAP3 gene. The THAP3 protein is as known as MGC33488, LOC90326, and THAP domain-containing, apoptosis associated protein 3. This protein contains the Thanatos-associated protein (THAP) domain and a host-cell factor 1C binding motif. These domains allow THAP3 to influence a variety of processes, including transcription and neuronal development. THAP3 is ubiquitously expressed in H. sapiens, though expression is highest in the kidneys.

NADP-dependent oxidoreductase domain-containing protein 1 is a protein that in humans is encoded by the NOXRED1 gene. An alias of this gene is Chromosome 14 Open Reading Frame 148 (c14orf148). This gene is located on chromosome 14, at 14q24.3. NOXRED1 is predicted to be involved in pyrroline-5-carboxylate reductase activity as part of the L-proline biosynthetic pathway. It is expressed in a wide variety of tissues at a relatively low level, including the testes, thyroid, skin, small intestine, brain, kidney, colon, and more.
SLC13A5 citrate transporter disorder, or SLC13A5 Epilepsy, is a rare genetic spectrum disorder that presents with neurological symptoms. Symptoms include severe seizures, ataxia, dystonia, teeth hypoplasia, poor communication skills, difficulty standing or walking, as well as developmental delay. Other names associated with SLC13A5 Epilepsy include SLC13A5 Citrate Transporter Disorder, Citrate Transporter Disorder, SLC13A5 Deficiency, Early Infantile Epilepsy Encephalopathy 25 (EIEE25), Developmental Epilepsy Encephalopathy 25 (DEE25), and Kohlschutter-Tonz Syndrome (non-ROGDI).

EVA1C is a transmembrane protein in humans that is encoded by the EVA1C gene on chromosome 21. The EVA1C protein is thought to be involved in herapin binding activity. In addition, the gene is thought to be associated with diseases such as X-Linked Intellectual Disability-Short Stature-Overweight Syndrome.
Leucine rich repeat containing 27 (LRRC27) isoform a is a protein which in humans is encoded by the LRRC27 gene.
References
- 1 2 3 4 5 6 7 8 9 10 11 "OMIM Entry - # 618744 - EPILEPTIC ENCEPHALOPATHY, EARLY INFANTILE, 83; EIEE83". omim.org.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 Perenthaler, E., Nikoncuk, A., Yousefi, S. et al. Loss of UGP2 in brain leads to a severe epileptic encephalopathy, emphasizing that bi-allelic isoform-specific start-loss mutations of essential genes can cause genetic diseases. Acta Neuropathol 139, 415–442 (2020). https://doi.org/10.1007/s00401-019-02109-6
- ↑ Happ, H. C., & Carvill, G. L. (2020). A 2020 View on the Genetics of Developmental and Epileptic Encephalopathies. Epilepsy Currents. https://doi.org/10.1177/1535759720906118
- ↑ Conroy, L.R., Hawkinson, T.R., Lyndsay, Young, E.A., Gentry, M.S., Sun, R.(2021) Emerging roles of N-linked glycosylation in brain physiology and disorders. Trends in Endocrinology and Metabolism. https://doi.org/10.1016/j.tem.2021.09.006
- ↑ "Unique variants in gene UGP2 - Global Variome shared LOVD". databases.lovd.nl.
- ↑ "UGP2 UDP-glucose pyrophosphorylase 2 [Homo sapiens (human)] - Gene - NCBI". www.ncbi.nlm.nih.gov.
- ↑ "OMIM Entry - * 191760 - URIDYL DIPHOSPHATE GLUCOSE PYROPHOSPHORYLASE 2; UGP2". omim.org.
- ↑ Flores-Diaz M, Alape-Giron A, Persson B, Pollesello P, Moos M, von Eichel-Streiber C et al (1997) Cellular UDP-glucose deficiency caused by a single point mutation in the UDP-glucose pyrophosphorylase gene. J Biol Chem 272:23784–23791; DOI: 10.1074/jbc.272.38.23784. https://www.jbc.org/content/272/38/23784
- ↑ Turnquist RL, Gillett TA, Hansen RG (1974) Uridine diphosphate glucose pyrophosphorylase. Crystallization and properties of the enzyme from rabbit liver and species comparisons. J Biol Chem 249:7695–7700; https://www.jbc.org/content/249/23/7695.long
- ↑ "UTP--glucose-1-phosphate uridylyltransferase isoform a [Homo sapiens] - Protein - NCBI". www.ncbi.nlm.nih.gov.
- ↑ "UTP--glucose-1-phosphate uridylyltransferase isoform b [Homo sapiens] - Protein - NCBI". www.ncbi.nlm.nih.gov.
- ↑ Fuhring J, Damerow S, Fedorov R, Schneider J, Munster-Kuhnel AK, Gerardy-Schahn R (2013) Octamerization is essential for enzymatic function of human UDP-glucose pyrophosphorylase. Glycobiology 23:426–437; https://doi.org/10.1093/glycob/cws217
- ↑ "VCV000805980.2 - ClinVar - NCBI". www.ncbi.nlm.nih.gov.
- ↑ "gnomAD". gnomad.broadinstitute.org.
- ↑ "UGDH UDP-glucose 6-dehydrogenase [Homo sapiens (human)] - Gene - NCBI". www.ncbi.nlm.nih.gov.
- ↑ Hengel, H., Bosso-Lefèvre, C., Grady, G. et al. Loss-of-function mutations in UDP-Glucose 6-Dehydrogenase cause recessive developmental epileptic encephalopathy. Nat Commun 11, 595 (2020). https://doi.org/10.1038/s41467-020-14360-7
- ↑ "OMIM Entry - # 618792 - EPILEPTIC ENCEPHALOPATHY, EARLY INFANTILE, 84; EIEE84". omim.org.
- ↑ (2010) Baluchistan i. Geography, history and ethnography. Encyclopædia Iranica City, pp fasc. 6, pp 598–632, available online http://www.iranicaonline.org/articles/baluchistan-i
- ↑ Durrant, Christelle; Fuehring, Jana I.; Willemetz, Alexandra; Chrétien, Dominique; Sala, Giusy; Ghidoni, Riccardo; Katz, Abram; Rötig, Agnès; Thelestam, Monica; Ermonval, Myriam; Moore, Stuart E. H. (March 16, 2020). "Defects in Galactose Metabolism and Glycoconjugate Biosynthesis in a UDP-Glucose Pyrophosphorylase-Deficient Cell Line Are Reversed by Adding Galactose to the Growth Medium". International Journal of Molecular Sciences. 21 (6): 2028. doi: 10.3390/ijms21062028 . PMC 7139386 . PMID 32188137.