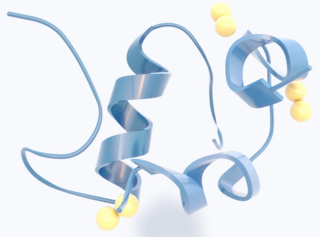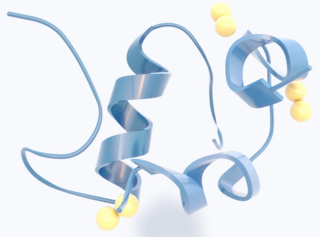
Insulin is a peptide hormone produced by beta cells of the pancreatic islets encoded in humans by the insulin (INS) gene. It is the main anabolic hormone of the body. It regulates the metabolism of carbohydrates, fats, and protein by promoting the absorption of glucose from the blood into cells of the liver, fat, and skeletal muscles. In these tissues the absorbed glucose is converted into either glycogen, via glycogenesis, or fats (triglycerides), via lipogenesis; in the liver, glucose is converted into both. Glucose production and secretion by the liver are strongly inhibited by high concentrations of insulin in the blood. Circulating insulin also affects the synthesis of proteins in a wide variety of tissues. It is thus an anabolic hormone, promoting the conversion of small molecules in the blood into large molecules in the cells. Low insulin in the blood has the opposite effect, promoting widespread catabolism, especially of reserve body fat.
Insulin resistance (IR) is a pathological condition in which cells in insulin-sensitive tissues in the body fail to respond normally to the hormone insulin or downregulate insulin receptors in response to hyperinsulinemia.

Beta cells (β-cells) are specialized endocrine cells located within the pancreatic islets of Langerhans responsible for the production and release of insulin and amylin. Constituting ~50–70% of cells in human islets, beta cells play a vital role in maintaining blood glucose levels. Problems with beta cells can lead to disorders such as diabetes.

Type 2 diabetes (T2D), formerly known as adult-onset diabetes, is a form of diabetes mellitus that is characterized by high blood sugar, insulin resistance, and relative lack of insulin. Common symptoms include increased thirst, frequent urination, fatigue and unexplained weight loss. Symptoms may also include increased hunger, having a sensation of pins and needles, and sores (wounds) that do not heal. Often, symptoms develop slowly. Long-term complications from high blood sugar include heart disease, stroke, diabetic retinopathy, which can result in blindness, kidney failure, and poor blood flow in the lower-limbs, which may lead to amputations. The sudden onset of hyperosmolar hyperglycemic state may occur; however, ketoacidosis is uncommon.
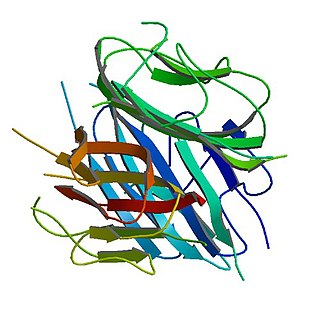
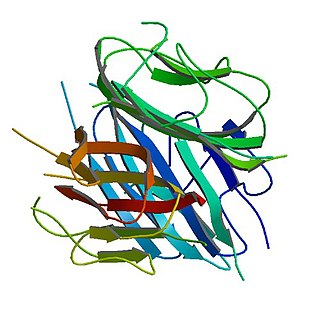
Adiponectin is a protein hormone and adipokine, which is involved in regulating glucose levels and fatty acid breakdown. In humans, it is encoded by the ADIPOQ gene and is produced primarily in adipose tissue, but also in muscle and even in the brain.

Resistin also known as adipose tissue-specific secretory factor (ADSF) or C/EBP-epsilon-regulated myeloid-specific secreted cysteine-rich protein (XCP1) is a cysteine-rich peptide hormone derived from adipose tissue that in humans is encoded by the RETN gene.

Ghrelin is a hormone primarily produced by enteroendocrine cells of the gastrointestinal tract, especially the stomach, and is often called a "hunger hormone" because it increases the drive to eat. Blood levels of ghrelin are highest before meals when hungry, returning to lower levels after mealtimes. Ghrelin may help prepare for food intake by increasing gastric motility and stimulating the secretion of gastric acid.

Hyperinsulinemia is a condition in which there are excess levels of insulin circulating in the blood relative to the level of glucose. While it is often mistaken for diabetes or hyperglycaemia, hyperinsulinemia can result from a variety of metabolic diseases and conditions, as well as non-nutritive sugars in the diet. While hyperinsulinemia is often seen in people with early stage type 2 diabetes mellitus, it is not the cause of the condition and is only one symptom of the disease. Type 1 diabetes only occurs when pancreatic beta-cell function is impaired. Hyperinsulinemia can be seen in a variety of conditions including diabetes mellitus type 2, in neonates and in drug-induced hyperinsulinemia. It can also occur in congenital hyperinsulinism, including nesidioblastosis.
Enteroglucagon is a peptide hormone derived from preproglucagon. It is a gastrointestinal hormone, secreted from mucosal cells primarily of the colon and terminal ileum. It consists of 37 amino acids. Enteroglucagon is released when fats and glucose are present in the small intestine; which decrease the motility to allow sufficient time for these nutrients to be absorbed.

Prediabetes is a component of metabolic syndrome and is characterized by elevated blood sugar levels that fall below the threshold to diagnose diabetes mellitus. It usually does not cause symptoms but people with prediabetes often have obesity, dyslipidemia with high triglycerides and/or low HDL cholesterol, and hypertension. It is also associated with increased risk for cardiovascular disease (CVD). Prediabetes is more accurately considered an early stage of diabetes as health complications associated with type 2 diabetes often occur before the diagnosis of diabetes.
Derek LeRoith is a South African endocrinologist and Professor of Medicine and the current Chief of the Hilda and J. Lester Gabrilove, M.D. Division of Endocrinology, Diabetes and Bone Disease and Director of the Metabolism Institute of the Mount Sinai Medical Center in New York City. He is an international expert in insulin-like growth factor-1 (IGF-1).

JeffreyFlier is an American physician, endocrinologist; widely cited scientist; the Higginson Professor of Medicine and Physiology at Harvard Medical School; and a Distinguished Service Professor at the same institution. He was the 21st Dean of the Faculty of Medicine at Harvard University from 2007 to 2016.
Andrej Janež is a Slovenian diabetologist and diabetes researcher. Janež is the Head of Department of Endocrinology, Diabetes and Metabolic Disease at University Medical Centre Ljubljana, Assistant Professor for Internal Medicine at the Medical University Ljubljana, Chairman of the Advances in Diabetes and Insulin Therapy conference, member of the advisory board for peroral antidiabetic therapy in Servier Pharma, member for Slovenia in the Diabetes Education Study Group at European Association for the Study of Diabetes, and member of the European advisory board for continuous glucose monitoring system in development for Lifescan.
Sleep is important in regulating metabolism. Mammalian sleep can be sub-divided into two distinct phases - REM and non-REM (NREM) sleep. In humans and cats, NREM sleep has four stages, where the third and fourth stages are considered slow-wave sleep (SWS). SWS is considered deep sleep, when metabolism is least active.

Leonid Poretsky is a Russian-born American endocrinologist. His research interests include mechanisms of insulin action in the ovary, endocrinological aspects of AIDS, and clinical outcomes in diabetes. He has authored over 150 publications and has served on the National Institutes of Health's review committees and on the editorial boards of the Journal of Clinical Endocrinology and Metabolism and other endocrine journals.
Mladen Vranic, MD, DSc, O.C., O.Ont, FRSC, FRCP(C), FCAHS, Canadian Medical Hall of Fame[CMHF] April 3, 1930 – June 18, 2019, was a Croatian-born diabetes researcher, best known for his work in tracer methodology, exercise and stress in diabetes, the metabolic effects of hormonal interactions, glucagon physiology, extrapancreatic glucagon, the role of the direct and indirect metabolic effects of insulin and the prevention of hypoglycemia. Vranic was recognized by a number of national and international awards for his research contributions, mentoring and administration including the Orders of Canada (Officer) and Ontario.
Asprosin is a protein hormone produced by mammals in tissues that stimulates the liver to release glucose into the blood stream. Asprosin is encoded by the gene FBN1 as part of the protein profibrillin and is released from the C-terminus of the latter by specific proteolysis. In the liver, asprosin activates rapid glucose release via a cyclic adenosine monophosphate (cAMP)-dependent pathway.

Christos Socrates Mantzoros is a Greek American physician-scientist, practicing internist-endocrinologist, teacher and researcher. He is a professor of medicine at Harvard Medical School and an adjunct professor at Boston University School of Medicine. He currently serves as the chief of endocrinology, diabetes and metabolism at the VA Boston Healthcare System, where he created de novo a leading academic division true to its tripartite mission and as the founding director of human nutrition at Beth Israel Deaconess Medical Center (BIDMC), Harvard Medical School. Finally, he holds the editor-in-chief position of the journal Metabolism: Clinical and Experimental.

Michael Roden is Professor and Chairman of Internal Medicine, Endocrinology and Metabolic Disorders at Heinrich Heine University Düsseldorf, Director of the Division of Endocrinology and Diabetology at the University Hospital of Düsseldorf and Spokesman for the Executive Board and Scientific Director of the German Diabetes Center, the Leibniz Center for Diabetes Research at the Heinrich Heine University Düsseldorf.
Pancreatic beta cell function is one of the preconditions of euglycaemia, i.e. normal blood sugar regulation. It is defined as insulin secretory capacity, i.e. the maximum amount of insulin to be produced by beta cells in a given unit of time.