Related Research Articles

An anticoagulant, commonly known as a blood thinner, is a chemical substance that prevents or reduces the coagulation of blood, prolonging the clotting time. Some occur naturally in blood-eating animals, such as leeches and mosquitoes, which help keep the bite area unclotted long enough for the animal to obtain blood.

Thrombosis is the formation of a blood clot inside a blood vessel, obstructing the flow of blood through the circulatory system. When a blood vessel is injured, the body uses platelets (thrombocytes) and fibrin to form a blood clot to prevent blood loss. Even when a blood vessel is not injured, blood clots may form in the body under certain conditions. A clot, or a piece of the clot, that breaks free and begins to travel around the body is known as an embolus.
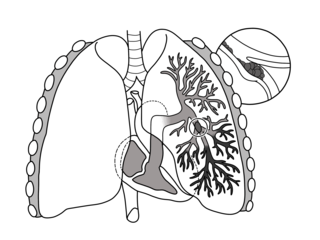
Pulmonary embolism (PE) is a blockage of an artery in the lungs by a substance that has moved from elsewhere in the body through the bloodstream (embolism). Symptoms of a PE may include shortness of breath, chest pain particularly upon breathing in, and coughing up blood. Symptoms of a blood clot in the leg may also be present, such as a red, warm, swollen, and painful leg. Signs of a PE include low blood oxygen levels, rapid breathing, rapid heart rate, and sometimes a mild fever. Severe cases can lead to passing out, abnormally low blood pressure, obstructive shock, and sudden death.

Venous thrombosis is the blockage of a vein caused by a thrombus. A common form of venous thrombosis is deep vein thrombosis (DVT), when a blood clot forms in the deep veins. If a thrombus breaks off (embolizes) and flows to the lungs to lodge there, it becomes a pulmonary embolism (PE), a blood clot in the lungs. The conditions of DVT only, DVT with PE, and PE only, are all captured by the term venous thromboembolism (VTE).

Deep vein thrombosis (DVT) is a type of venous thrombosis involving the formation of a blood clot in a deep vein, most commonly in the legs or pelvis. A minority of DVTs occur in the arms. Symptoms can include pain, swelling, redness, and enlarged veins in the affected area, but some DVTs have no symptoms.
D-dimer is a dimer that is a fibrin degradation product (FDP), a small protein fragment present in the blood after a blood clot is degraded by fibrinolysis. It is so named because it contains two D fragments of the fibrin protein joined by a cross-link, hence forming a protein dimer.

Thrombophilia is an abnormality of blood coagulation that increases the risk of thrombosis. Such abnormalities can be identified in 50% of people who have an episode of thrombosis that was not provoked by other causes. A significant proportion of the population has a detectable thrombophilic abnormality, but most of these develop thrombosis only in the presence of an additional risk factor.
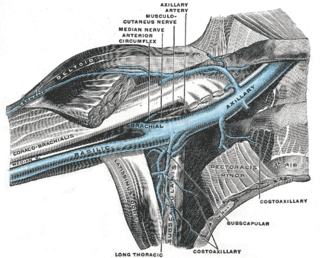
Paget–Schroetter disease is a form of upper extremity deep vein thrombosis (DVT), a medical condition in which blood clots form in the deep veins of the arms. These DVTs typically occur in the axillary and/or subclavian veins.

Vascular disease is a class of diseases of the vessels of the circulatory system in the body, including blood vessels – the arteries and veins, and the lymphatic vessels. Vascular disease is a subgroup of cardiovascular disease. Disorders in this vast network of blood and lymph vessels can cause a range of health problems that can sometimes become severe, and fatal. Coronary heart disease for example, is the leading cause of death for men and women in the United States.

Post-thrombotic syndrome (PTS), also called postphlebitic syndrome and venous stress disorder is a medical condition that may occur as a long-term complication of deep vein thrombosis (DVT).
Helge Stormorken was a Norwegian veterinarian and physician.
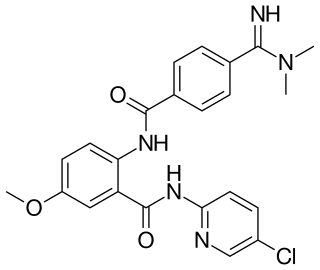
Betrixaban is an oral anticoagulant drug which acts as a direct factor Xa inhibitor. Betrixaban is FDA approved for venous thrombosis prevention in adults hospitalized for an acute illness who are at risk for thromboembolic complications. Compared to other directly acting oral anticoagulants betrixaban has relatively low renal excretion and is not metabolized by CYP3A4.
Prothrombin G20210A is a genotypic trait that provides a prompter coagulation response. It increases the risk of blood clots including from deep vein thrombosis, and of pulmonary embolism. One copy of the mutation increases the risk of a blood clot from 1 in 1,000 per year to 2.5 in 1,000. Two copies increases the risk to up to 20 in 1,000 per year. Most people never develop a blood clot in their lifetimes.
Thrombosis UK is a UK based charity whose stated mission is to increase awareness of thrombosis among the public and health professionals, and to raise research funds to improve patient care through improved prevention and treatment of venous thromboembolic disease.

Superficial vein thrombosis (SVT) is a blood clot formed in a superficial vein, a vein near the surface of the body. Usually there is thrombophlebitis, which is an inflammatory reaction around a thrombosed vein, presenting as a painful induration with redness. SVT itself has limited significance when compared to a deep vein thrombosis (DVT), which occurs deeper in the body at the deep venous system level. However, SVT can lead to serious complications, and is therefore no longer regarded as a benign condition. If the blood clot is too near the saphenofemoral junction there is a higher risk of pulmonary embolism, a potentially life-threatening complication.
Brian Trevor Colvin is a British haematologist.

Thrombosis prevention or thromboprophylaxis is medical treatment to prevent the development of thrombosis in those considered at risk for developing thrombosis. Some people are at a higher risk for the formation of blood clots than others, such as those with cancer undergoing a surgical procedure. Prevention measures or interventions are usually begun after surgery as the associated immobility will increase a person's risk.
Henri Bounameaux is a clinical faculty and Professor of Medicine (hon), specialized in internal and vascular medicine (angiology), and general medicine.

Post-vaccination embolic and thrombotic events, termed vaccine-induced immune thrombotic thrombocytopenia (VITT), vaccine-induced prothrombotic immune thrombocytopenia (VIPIT), thrombosis with thrombocytopenia syndrome (TTS), vaccine-induced immune thrombocytopenia and thrombosis (VITT), or vaccine-associated thrombotic thrombocytopenia (VATT), are rare types of blood clotting syndromes that were initially observed in a number of people who had previously received the Oxford–AstraZeneca COVID‑19 vaccine (AZD1222) during the COVID‑19 pandemic. It was subsequently also described in the Janssen COVID‑19 vaccine, leading to the suspension of its use until its safety had been reassessed. On 5 May 2022 the FDA posted a bulletin limiting the use of the Janssen Vaccine to very specific cases due to further reassessment of the risks of TTS, although the FDA also stated in the same bulletin that the benefits of the vaccine outweigh the risks.

Marie Claire McLintock was a New Zealand haematologist and obstetric physician. She was an expert in medical conditions and disorders related to bleeding and blood clotting, and medical problems associated with pregnancy.
References
- ↑ "Comment" (PDF). King's College London. February 2009. Archived (PDF) from the original on 2014-01-07. Retrieved 2014-01-15.
- ↑ "The Louise Coote Lupus Unit team". Guysandstthomas.nhs.uk. Archived from the original on 2012-09-02. Retrieved 2012-07-18.
- ↑ "Blood Sciences contact details". GSTS. Archived from the original on 2013-02-10. Retrieved 2012-07-18.
- ↑ "Professor Hunt wins 'Medical Oscar'". Walthamstow-hall.co.uk. 2011-05-26. Archived from the original on 2014-01-07. Retrieved 2012-07-18.
- ↑ "Alumnae Profiles". Walthamstow-hall.co.uk. 2011-05-29. Archived from the original on 2011-04-24. Retrieved 2012-07-18.
- ↑ "Obstetric haematology information for patients". Guysandstthomas.nhs.uk. Archived from the original on 2012-09-02. Retrieved 2012-07-18.
- ↑ Hunt, Beverley. "Steering Committee Char". World Thrombosis Day website. Archived from the original on 2022-10-20. Retrieved 2022-10-20.
- ↑ "The Obstetric Hematology Manual – Academic and Professional Books – Cambridge University Press". Cambridge.org. Retrieved 2012-07-18.
- ↑ Hunt, Beverley J.; Poston, Lucilla; Schachter, Michael (2002-07-25). An Introduction to Vascular Biology: From Basic Science to Clinical Practice – Beverley J. Hunt, Lucilla Poston – Google Books. Cambridge University Press. ISBN 9780521796521. Archived from the original on 2024-07-26. Retrieved 2012-07-18.
- ↑ "British Society for Haematology ABOUT US". B-s-h.org.uk. Retrieved 2014-01-16.
- ↑ "British Society for Haematology New BSH education committee". Archived from the original on 2012-01-06. Retrieved 2012-05-30.
- ↑ "British Society for Haemostasis and Thrombosis Homepage". BSHT. 16 December 2013. Archived from the original on 2013-10-09. Retrieved 2014-01-15.
- ↑ "International Society on Thrombosis & Haemostasis". Archived from the original on June 5, 2012. Retrieved May 30, 2012.
- ↑ Hunt, Beverley. "World Thrombosis Day website". Archived from the original on 2022-10-20. Retrieved 2022-10-20.
- ↑ http://www.rcog.org.uk/womens-health/clinical.../air-travel-and-pregnancy . Retrieved May 30, 2012.
{{cite web}}: Missing or empty|title=(help)[ dead link ] - ↑ "Wiley: Journals, books, and online products and services" (PDF). Blackwellpublishing.com. Retrieved 2014-01-16.[ permanent dead link ]
- ↑ Provan, Drew; Stasi, Roberto; Newland, Adrian C.; Blanchette, Victor S.; Bolton-Maggs, Paula; Bussel, James B.; Chong, Beng H.; Cines, Douglas B.; Gernsheimer, Terry B.; Godeau, Bertrand; Grainger, John; Greer, Ian; Hunt, Beverley J.; Imbach, Paul A.; Lyons, Gordon; McMillan, Robert; Rodeghiero, Francesco; Sanz, Miguel A.; Tarantino, Michael; Watson, Shirley; Young, Joan; Kuter, David J. (2010). "International consensus report on the investigation and management of primary immune thrombocytopenia". Blood. 115 (2). Bloodjournal.hematologylibrary.org: 168–186. doi: 10.1182/blood-2009-06-225565 . PMID 19846889. S2CID 22037567. Archived from the original on 2014-03-26. Retrieved 2014-01-16.
- ↑ "Clinical guidelines for testing for heritable thrombophilia" (PDF). 2010. Archived from the original (PDF) on 2014-01-16. Retrieved 2014-01-15.
- ↑ "Guideline for investigation and management of adults and children presenting with a thrombocytosis" (PDF). BCSH. 2010. Archived from the original (PDF) on 2013-01-16. Retrieved 2014-01-16.
- ↑ Rossaint R, Bouillon B, Cerny V, Coats TJ, Duranteau J, Fernández-Mondéjar E, Hunt BJ, Komadina R, Nardi G, Neugebauer E, Ozier Y, Riddez L, Schultz A, Stahel PF, Vincent JL, Spahn DR (2013-08-12). "Management of bleeding following major trauma: an updated European guideline". Crit Care. 14 (2): R52. doi: 10.1186/cc8943 . PMC 2887168 . PMID 20370902.
- ↑ "Venous thromboembolism – reducing the risk". Guidance.nice.org.uk. 2013-11-07. Archived from the original on 2014-01-16. Retrieved 2014-01-16.
- ↑ "VTE prevention". Guidance.nice.org.uk. 2013-04-15. Archived from the original on 2014-01-16. Retrieved 2014-01-16.
- ↑ "Lifeblood – Our History". Thrombosis-charity.org.uk. Archived from the original on 2008-06-18. Retrieved 2012-07-18.
- ↑ "World Thrombosis Day website". www.worldthrombosisday.org/. Archived from the original on 2022-10-20. Retrieved 2022-10-20.
- ↑ "King's doctor wins health innovator award – King's College Hospital NHS Foundation Trust". Kch.nhs.uk. 2010-01-27. Archived from the original on 2014-01-16. Retrieved 2012-07-18.
- ↑ "Meet the winners! — BMJ Group Awards". Groupawards.bmj.com. Retrieved 2012-07-18.[ permanent dead link ]
- ↑ "CRASH-2 – Clinical Randomisation of an Antifibrinolytic in Significant Haemorrhage". Crash2.lshtm.ac.uk. Archived from the original on 2011-10-05. Retrieved 2012-07-18.
- ↑ "News detail – King's Health Partners". Kingshealthpartners.org. 2011-05-20. Retrieved 2014-01-16.
- ↑ "No. 62666". The London Gazette (Supplement). 8 June 2019. p. B12.