Related Research Articles

Hypnotic, or soporific drugs, commonly known as sleeping pills, are a class of psychoactive drugs whose primary function is to induce sleep and to treat insomnia (sleeplessness).

Neurology is the branch of medicine dealing with the diagnosis and treatment of all categories of conditions and disease involving the nervous system, which comprises the brain, the spinal cord and the peripheral nerves. Neurological practice relies heavily on the field of neuroscience, the scientific study of the nervous system.

A sleep disorder, or somnipathy, is a medical disorder of an individual's sleep patterns. Some sleep disorders are severe enough to interfere with normal physical, mental, social and emotional functioning. Sleep disorders are frequent and can have serious consequences on patients' health and quality of life. Polysomnography and actigraphy are tests commonly ordered for diagnosing sleep disorders.

A respiratory therapist is a specialized healthcare practitioner trained in critical care and cardio-pulmonary medicine in order to work therapeutically with people who have acute critical conditions, cardiac and pulmonary disease. Respiratory therapists graduate from a college or university with a degree in respiratory therapy and have passed a national board certifying examination. The NBRC is responsible for credentialing as a CRT, or RRT,

Insomnia, also known as sleeplessness, is a sleep disorder where people have trouble sleeping. They may have difficulty falling asleep, or staying asleep for as long as desired. Insomnia is typically followed by daytime sleepiness, low energy, irritability, and a depressed mood. It may result in an increased risk of accidents of all kinds as well as problems focusing and learning. Insomnia can be short term, lasting for days or weeks, or long term, lasting more than a month. The concept of the word insomnia has two possibilities: insomnia disorder (ID) and insomnia symptoms, and many abstracts of randomized controlled trials and systematic reviews often underreport on which of these two possibilities the word insomnia refers to.
Clinical neurophysiology is a medical specialty that studies the central and peripheral nervous systems through the recording of bioelectrical activity, whether spontaneous or stimulated. It encompasses both research regarding the pathophysiology along with clinical methods used to diagnose diseases involving both central and peripheral nervous systems. Examinations in the clinical neurophysiology field are not limited to tests conducted in a laboratory. It is thought of as an extension of a neurologic consultation. Tests that are conducted are concerned with measuring the electrical functions of the brain, spinal cord, and nerves in the limbs and muscles. It can give the precise definition of site, the type and degree of the lesion, along with revealing the abnormalities that are in question. Due to these abilities, clinical neurophysiology is used to mainly help diagnose diseases rather than treat them.

Sleep hygiene is a behavioral and environmental practice developed in the late 1970s as a method to help people with mild to moderate insomnia. Clinicians assess the sleep hygiene of people with insomnia and other conditions, such as depression, and offer recommendations based on the assessment. Sleep hygiene recommendations include: establishing a regular sleep schedule; using naps with care; not exercising physically or mentally too close to bedtime; limiting worry; limiting exposure to light in the hours before sleep; getting out of bed if sleep does not come; not using bed for anything but sleep and sex; avoiding alcohol as well as nicotine, caffeine, and other stimulants in the hours before bedtime; and having a peaceful, comfortable and dark sleep environment. However, as of 2021, the empirical evidence for the effectiveness of sleep hygiene is "limited and inconclusive" for the general population and for the treatment of insomnia, despite being the oldest treatment for insomnia. A systematic review by the AASM concluded that clinicians should not prescribe sleep hygiene for insomnia due to the evidence of absence of its efficacy and potential delaying of adequate treatment, recommending instead that effective therapies such as CBT-i should be preferred.

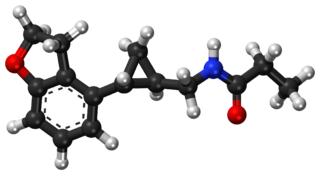
Eszopiclone, sold under the brand name Lunesta among others, is a medication used in the treatment of insomnia. Evidence supports slight to moderate benefit up to six months. It is taken by mouth.

Somnology is the scientific study of sleep. It includes clinical study and treatment of sleep disorders and irregularities. Sleep medicine is a subset of somnology.
The American Academy of Sleep Medicine (AASM) is a United States professional society for the medical subspecialty of sleep medicine which includes disorders of circadian rhythms. It was established in 1975.
The International Classification of Sleep Disorders (ICSD) is "a primary diagnostic, epidemiological and coding resource for clinicians and researchers in the field of sleep and sleep medicine". The ICSD was produced by the American Academy of Sleep Medicine (AASM) in association with the European Sleep Research Society, the Japanese Society of Sleep Research, and the Latin American Sleep Society. The classification was developed as a revision and update of the Diagnostic Classification of Sleep and Arousal Disorders (DCSAD) that was produced by both the Association of Sleep Disorders Centers (ASDC) and the Association for the Psychophysiological Study of Sleep and was published in the journal Sleep in 1979. A second edition, called ICSD-2, was published by the AASM in 2005. The third edition, ICSD-3, was released by the AASM in 2014. A text revision of the third edition (ICSD-3-TR) was published in 2023 by the AASM.

Sleep medicine is a medical specialty or subspecialty devoted to the diagnosis and therapy of sleep disturbances and disorders. From the middle of the 20th century, research has provided increasing knowledge of, and answered many questions about, sleep–wake functioning. The rapidly evolving field has become a recognized medical subspecialty in some countries. Dental sleep medicine also qualifies for board certification in some countries. Properly organized, minimum 12-month, postgraduate training programs are still being defined in the United States. In some countries, the sleep researchers and the physicians who treat patients may be the same people.
Tasimelteon, sold under the brand name Hetlioz, is a medication approved by the U.S. Food and Drug Administration (FDA) in January 2014, for the treatment of non-24-hour sleep–wake disorder. In June 2014, the European Medicines Agency (EMA) accepted an EU filing application for tasimelteon and in July 2015, the drug was approved in the European Union for the treatment of non-24-hour sleep-wake rhythm disorder in totally blind adults, but not in the case of non-24 in sighted people.

Esmirtazapine (ORG-50,081) is a tetracyclic antidepressant drug that was under development by Organon for the treatment of insomnia and vasomotor symptoms (e.g., hot flashes) associated with menopause. Esmirtazapine is the (S)-(+)-enantiomer of mirtazapine and possesses similar overall pharmacology, including inverse agonist actions at H1 and 5-HT2 receptors and antagonist actions at α2-adrenergic receptors.
Sleep state misperception (SSM) is a term in the International Classification of Sleep Disorders (ICSD) most commonly used for people who mistakenly perceive their sleep as wakefulness, though it has been proposed that it be applied to those who severely overestimate their sleep time as well. While most sleepers with this condition will report not having slept in the previous night at all or having slept very little, clinical recordings generally show normal sleep patterns. Though the sleep patterns found in those with SSM have long been considered indistinguishable from those without, some preliminary research suggest there may be subtle differences.
Clinical neuroscience is a branch of neuroscience that focuses on the scientific study of fundamental mechanisms that underlie diseases and disorders of the brain and central nervous system. It seeks to develop new ways of conceptualizing and diagnosing such disorders and ultimately of developing novel treatments.
Colin Espie PhD, DSc, FRSM, FBPsS FAASM is a Scottish Professor of Sleep Medicine in the Nuffield Department of Clinical Neuroscience at the University of Oxford and Fellow of Somerville College. He is closely involved with the development of the Sir Jules Thorn Sleep & Circadian Neuroscience Institute (SCNi) where he is Founding Director of the Experimental & Clinical Sleep Medicine Research programme, and Clinical Director of the Oxford Online Programme in Sleep Medicine. His particular areas of research expertise are in the assessment and treatment of sleep disorders, most particularly the management of insomnia using Cognitive Behavioral Therapy, and in studies on the aetiology and pathophysiology of insomnia.

Lemborexant, sold under the brand name Dayvigo, is an orexin antagonist medication which is used in the treatment of insomnia. It is indicated specifically for the treatment of insomnia characterized by difficulties with sleep onset and/or maintenance in adults. The medication is taken by mouth.

Behavioral sleep medicine (BSM) is a field within sleep medicine that encompasses scientific inquiry and clinical treatment of sleep-related disorders, with a focus on the psychological, physiological, behavioral, cognitive, social, and cultural factors that affect sleep, as well as the impact of sleep on those factors. The clinical practice of BSM is an evidence-based behavioral health discipline that uses primarily non-pharmacological treatments. BSM interventions are typically problem-focused and oriented towards specific sleep complaints, but can be integrated with other medical or mental health treatments. The primary techniques used in BSM interventions involve education and systematic changes to the behaviors, thoughts, and environmental factors that initiate and maintain sleep-related difficulties.

Somnifacient, also known as sedatives or sleeping pills, is a class of medications that induces sleep. It is mainly used for treatment of insomnia. Examples of somnifacients include benzodiazepines, barbiturates and antihistamines.
References
- ↑ "Home". sleepsociety.org.uk.
- ↑ "Appendix B: Sources of evidence considered by the Committee | Continuous positive airway pressure for the treatment of obstructive sleep apnoea/Hypopnoea syndrome | Guidance | NICE". 26 March 2008.
- ↑ "Appendix B. Sources of evidence considered by the Committee | Guidance on the use of zaleplon, zolpidem and zopiclone for the short-term management of insomnia | Guidance | NICE". 28 April 2004.
- 1 2 "Newcastle hosts the British Sleep Society Conference". 21 October 2015.
- ↑ "Quarter of Brit workers get less than five hours sleep a night - Mirror Online". Daily Mirror . 20 October 2015.
- ↑ "Sleep Problems". sleepcouncil.org.uk. The Sleep Council. Archived from the original on Dec 3, 2012.
- ↑ "British Sleep Society : Tees Valley Public Health Shared Service". Archived from the original on 2016-03-04. Retrieved 2015-11-27.
- ↑ "British Sleep Society - Insomnia Support Group UK | Patient". Archived from the original on 2016-01-04. Retrieved 2015-11-27.
- ↑ "Executive Committee – British Sleep Society". Archived from the original on 2016-03-04. Retrieved 2015-11-25.
- ↑ "Home". rccp.co.uk.
- ↑ "The British Sleep Society (BSS) - RCCP". www.rccp.co.uk. Archived from the original on 2016-03-04.
- ↑ "European Sleep Research Society / UNITED KINGDOM". Archived from the original on 2016-03-04. Retrieved 2015-11-25.
- 1 2 "ISMC and Hands on Meeting – British Sleep Society". Archived from the original on 2016-02-14. Retrieved 2015-11-25.
- ↑ "Home - ESRS". 19 August 2021.[ permanent dead link ]