Neurology is the branch of medicine dealing with the diagnosis and treatment of all categories of conditions and disease involving the nervous system, which comprises the brain, the spinal cord and the peripheral nerves. Neurological practice relies heavily on the field of neuroscience, the scientific study of the nervous system.
A transient ischemic attack (TIA), commonly known as a mini-stroke, is a minor stroke whose noticeable symptoms usually end in less than an hour. TIA causes the same symptoms associated with strokes, such as weakness or numbness on one side of the body, sudden dimming or loss of vision, difficulty speaking or understanding language, slurred speech, or confusion.

Vascular surgery is a surgical subspecialty in which vascular diseases involving the arteries, veins, or lymphatic vessels, are managed by medical therapy, minimally-invasive catheter procedures and surgical reconstruction. The specialty evolved from general and cardiovascular surgery where it refined the management of just the vessels, no longer treating the heart or other organs. Modern vascular surgery includes open surgery techniques, endovascular techniques and medical management of vascular diseases - unlike the parent specialities. The vascular surgeon is trained in the diagnosis and management of diseases affecting all parts of the vascular system excluding the coronaries and intracranial vasculature. Vascular surgeons also are called to assist other physicians to carry out surgery near vessels, or to salvage vascular injuries that include hemorrhage control, dissection, occlusion or simply for safe exposure of vascular structures.

Cerebral angiography is a form of angiography which provides images of blood vessels in and around the brain, thereby allowing detection of abnormalities such as arteriovenous malformations and aneurysms. It was pioneered in 1927 by the Portuguese neurologist Egas Moniz at the University of Lisbon, who also helped develop thorotrast for use in the procedure.

Carotid endarterectomy is a surgical procedure used to reduce the risk of stroke from carotid artery stenosis. In endarterectomy, the surgeon opens the artery and removes the plaque. The plaque forms and thickens the inner layer of the artery, or intima, hence the name of the procedure which simply means removal of part of the internal layers of the artery.

Carotid artery stenosis is a narrowing or constriction of any part of the carotid arteries, usually caused by atherosclerosis.

Intraparenchymal hemorrhage (IPH) is one form of intracerebral bleeding in which there is bleeding within brain parenchyma. The other form is intraventricular hemorrhage (IVH).

Transcranial Doppler (TCD) and transcranial color Doppler (TCCD) are types of Doppler ultrasonography that measure the velocity of blood flow through the brain's blood vessels by measuring the echoes of ultrasound waves moving transcranially. These modes of medical imaging conduct a spectral analysis of the acoustic signals they receive and can therefore be classified as methods of active acoustocerebrography. They are used as tests to help diagnose emboli, stenosis, vasospasm from a subarachnoid hemorrhage, and other problems. These relatively quick and inexpensive tests are growing in popularity. The tests are effective for detecting sickle cell disease, ischemic cerebrovascular disease, subarachnoid hemorrhage, arteriovenous malformations, and cerebral circulatory arrest. The tests are possibly useful for perioperative monitoring and meningeal infection. The equipment used for these tests is becoming increasingly portable, making it possible for a clinician to travel to a hospital, to a doctor's office, or to a nursing home for both inpatient and outpatient studies. The tests are often used in conjunction with other tests such as MRI, MRA, carotid duplex ultrasound and CT scans. The tests are also used for research in cognitive neuroscience.

A watershed stroke is defined as a brain ischemia that is localized to the vulnerable border zones between the tissues supplied by the anterior, posterior and middle cerebral arteries. The actual blood stream blockage/restriction site can be located far away from the infarcts. Watershed locations are those border-zone regions in the brain supplied by the major cerebral arteries where blood supply is decreased. Watershed strokes are a concern because they comprise approximately 10% of all ischemic stroke cases. The watershed zones themselves are particularly susceptible to infarction from global ischemia as the distal nature of the vasculature predisposes these areas to be most sensitive to profound hypoperfusion.

Subclavian steal syndrome (SSS), also called subclavian steal steno-occlusive disease, is a constellation of signs and symptoms that arise from retrograde (reversed) blood flow in the vertebral artery or the internal thoracic artery, due to a proximal stenosis (narrowing) and/or occlusion of the subclavian artery. This flow reversal is called the subclavian steal or subclavian steal phenomenon, regardless of signs/symptoms being present. The arm may be supplied by blood flowing in a retrograde direction down the vertebral artery at the expense of the vertebrobasilar circulation. It is more severe than typical vertebrobasilar insufficiency.

Carotid artery dissection is a separation of the layers of the artery wall in the carotid arteries supplying oxygen-bearing blood to the head. It is the most common cause of stroke in younger adults. The term 'cervical artery dissection' should also be considered in the context of this article.

Vertebral artery dissection (VAD) is a flap-like tear of the inner lining of the vertebral artery, which is located in the neck and supplies blood to the brain. After the tear, blood enters the arterial wall and forms a blood clot, thickening the artery wall and often impeding blood flow. The symptoms of vertebral artery dissection include head and neck pain and intermittent or permanent stroke symptoms such as difficulty speaking, impaired coordination, and visual loss. It is usually diagnosed with a contrast-enhanced CT or MRI scan.

Carotid artery stenting is an endovascular procedure where a stent is deployed within the lumen of the carotid artery to treat narrowing of the carotid artery and decrease the risk of stroke. It is used to treat narrowing of the carotid artery in high-risk patients, when carotid endarterectomy is considered too risky.

The leptomeningeal collateral circulation is a network of small blood vessels in the brain that connects branches of the middle, anterior and posterior cerebral arteries, with variation in its precise anatomy between individuals. During a stroke, leptomeningeal collateral vessels allow limited blood flow when other, larger blood vessels provide inadequate blood supply to a part of the brain.

Carotid ultrasonography is an ultrasound-based diagnostic imaging technique to evaluate structural details of the carotid arteries. Carotid ultrasound is used to diagnose carotid artery stenosis (CAS) and can assess atherosclerotic plaque morphology and characteristics. Carotid duplex and contrast-enhanced ultrasound are two of the most common imaging techniques used to evaluate carotid artery disease.
John David Spence is a Canadian medical doctor, medical researcher and Professor Emeritus at the University of Western Ontario. He is affiliated with the University of Western Ontario and the Robarts Research Institute, one of Canada's leading medical research organizations. Before his retirement from clinical practice in July 2022, he was also affiliated with the London Health Sciences Centre's University Hospital. He is a recognized expert in stroke prevention and stroke prevention research, with more than 600 peer-reviewed publications since 1970. He delivered more than 600 lectures on stroke prevention in 42 countries. In 2015, he received the Research Excellence Award from the Canadian Society for Atherosclerosis, Thrombosis and Vascular Biology. In 2019, he was appointed a Member of the Order of Canada, and in 2020 he received the William Feinberg Award from the American Heart Association for excellence in clinical stroke research.
Interventional neuroradiology (INR) also known as neurointerventional surgery (NIS), endovascular therapy (EVT), endovascular neurosurgery, and interventional neurology is a medical subspecialty of neurosurgery, neuroradiology, intervention radiology and neurology specializing in minimally invasive image-based technologies and procedures used in diagnosis and treatment of diseases of the head, neck, and spine.

Michael Jeffrey Aminoff is a clinical neurologist and neurophysiologist whose later clinical work focused on treating Parkinson's disease and related movement disorders. He retired in 2022 and lives in San Francisco, California.
Elad I. Levy is an American neurosurgeon, researcher, and innovator who played a major role in the development and testing of thrombectomy, which improved quality of life and survival of stroke patients. He has focused his career and research on developing evidence based medicine and literature showing the benefits of thrombectomy for the treatment of stroke. He is currently Professor of Neurosurgery and Radiology, and the L. Nelson Hopkins, MD Professor Endowed Chair of the Department of Neurosurgery at the State University of New York at Buffalo (SUNY).
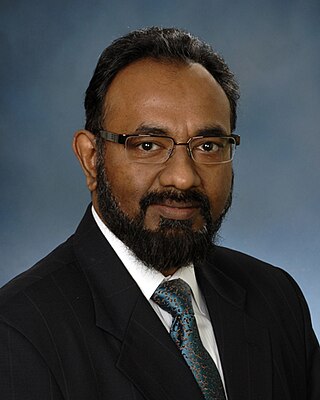
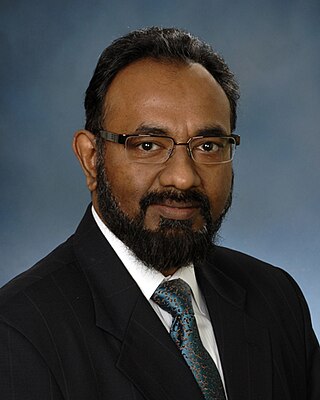
Brajesh K. Lal, born in 1963 in Varanasi, India and of Indian origin, is an American surgeon, and an expert in vascular disease, particularly the prevention and treatment of stroke and venous disease. He is a tenured Professor of Vascular Surgery at the University of Maryland and Professor of Neurology at Mayo Clinic. He holds additional appointments at the Departments of Bioengineering at the University of Maryland and George Mason University. He founded and currently directs the multi-specialty Center for Vascular Research and the NIH Vascular Imaging Core Facility at the University of Maryland. He has been elected as a Distinguished Fellow of the Society for Vascular Surgery and Distinguished Fellow of the American Venous Forum.