Related Research Articles

Asthma is a long-term inflammatory disease of the airways of the lungs. It is characterized by variable and recurring symptoms, reversible airflow obstruction, and easily triggered bronchospasms. Symptoms include episodes of wheezing, coughing, chest tightness, and shortness of breath. These may occur a few times a day or a few times per week. Depending on the person, asthma symptoms may become worse at night or with exercise.

A respiratory therapist is a specialized healthcare practitioner trained in critical care and cardio-pulmonary medicine in order to work therapeutically with people who have acute critical conditions, cardiac and pulmonary disease. Respiratory therapists graduate from a college or university with a degree in respiratory therapy and have passed a national board certifying examination. The NBRC is responsible for credentialing as a CRT, or RRT,
Alpha-1 antitrypsin deficiency is a genetic disorder that may result in lung disease or liver disease. Onset of lung problems is typically between 20 and 50 years of age. This may result in shortness of breath, wheezing, or an increased risk of lung infections. Complications may include chronic obstructive pulmonary disease (COPD), cirrhosis, neonatal jaundice, or panniculitis.

Oxygen therapy, also referred to as supplemental oxygen, is the use of oxygen as medical treatment. Supplemental oxygen can also refer to the use of oxygen enriched air at altitude. Acute indications for therapy include hypoxemia, carbon monoxide toxicity and cluster headache. It may also be prophylactically given to maintain blood oxygen levels during the induction of anesthesia. Oxygen therapy is often useful in chronic hypoxemia caused by conditions such as severe COPD or cystic fibrosis. Oxygen can be delivered via nasal cannula, face mask, or endotracheal intubation at normal atmospheric pressure, or in a hyperbaric chamber. It can also be given through bypassing the airway, such as in ECMO therapy.

Non-invasive ventilation (NIV) is the use of breathing support administered through a face mask, nasal mask, or a helmet. Air, usually with added oxygen, is given through the mask under positive pressure; generally the amount of pressure is alternated depending on whether someone is breathing in or out. It is termed "non-invasive" because it is delivered with a mask that is tightly fitted to the face or around the head, but without a need for tracheal intubation. While there are similarities with regard to the interface, NIV is not the same as continuous positive airway pressure (CPAP), which applies a single level of positive airway pressure throughout the whole respiratory cycle; CPAP does not deliver ventilation but is occasionally used in conditions also treated with NIV.
Bronchoalveolar lavage (BAL), also known as bronchoalveolar washing, is a diagnostic method of the lower respiratory system in which a bronchoscope is passed through the mouth or nose into an appropriate airway in the lungs, with a measured amount of fluid introduced and then collected for examination. This method is typically performed to diagnose pathogenic infections of the lower respiratory airways, though it also has been shown to have utility in diagnosing interstitial lung disease. Bronchoalveolar lavage can be a more sensitive method of detection than nasal swabs in respiratory molecular diagnostics, as has been the case with SARS-CoV-2 where bronchoalveolar lavage samples detect copies of viral RNA after negative nasal swab testing.
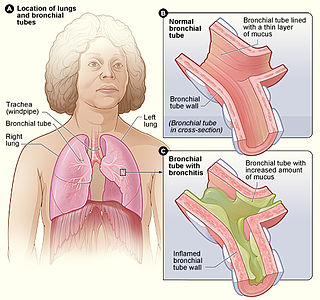
Bronchitis is inflammation of the bronchi in the lungs that causes coughing. Bronchitis usually begins as an infection in the nose, ears, throat, or sinuses. The infection then makes its way down to the bronchi. Symptoms include coughing up sputum, wheezing, shortness of breath, and chest pain. Bronchitis can be acute or chronic.

Pulmonary function testing (PFT) is a complete evaluation of the respiratory system including patient history, physical examinations, and tests of pulmonary function. The primary purpose of pulmonary function testing is to identify the severity of pulmonary impairment. Pulmonary function testing has diagnostic and therapeutic roles and helps clinicians answer some general questions about patients with lung disease. PFTs are normally performed by a pulmonary function technologist, respiratory therapist, respiratory physiologist, physiotherapist, pulmonologist, or general practitioner.
Pulmonary rehabilitation, also known as respiratory rehabilitation, is an important part of the management and health maintenance of people with chronic respiratory disease who remain symptomatic or continue to have decreased function despite standard medical treatment. It is a broad therapeutic concept. It is defined by the American Thoracic Society and the European Respiratory Society as an evidence-based, multidisciplinary, and comprehensive intervention for patients with chronic respiratory diseases who are symptomatic and often have decreased daily life activities. In general, pulmonary rehabilitation refers to a series of services that are administered to patients of respiratory disease and their families, typically to attempt to improve the quality of life for the patient. Pulmonary rehabilitation may be carried out in a variety of settings, depending on the patient's needs, and may or may not include pharmacologic intervention.

An acute exacerbation of chronic obstructive pulmonary disease, or acute exacerbations of chronic bronchitis (AECB), is a sudden worsening of chronic obstructive pulmonary disease (COPD) symptoms including shortness of breath, quantity and color of phlegm that typically lasts for several days.
In some individuals, the effect of oxygen on chronic obstructive pulmonary disease is to cause increased carbon dioxide retention,
Meyer Stanley Balter, MD, FRCPC, FACP, FCCP is a Canadian physician specializing in asthma, sarcoidosis and chronic obstructive pulmonary disease (COPD).

Chronic obstructive pulmonary disease (COPD) is a type of progressive lung disease characterized by long-term respiratory symptoms and airflow limitation. GOLD 2024 defined COPD as a heterogeneous lung condition characterized by chronic respiratory symptoms due to abnormalities of the airways and/or alveoli (emphysema) that cause persistent, often progressive, airflow obstruction.

Sir Peter John Barnes, FRCP, FCCP, FMedSci, FRS is a British respiratory scientist and clinician, a specialist in the mechanisms and treatment of asthma and chronic obstructive pulmonary disease (COPD). He was Margaret Turner-Warwick Professor of Thoracic Medicine at the National Heart & Lung Institute, previous head of respiratory medicine at Imperial College and honorary consultant physician at the Royal Brompton Hospital London. He is one of the most highly cited scientists in the world
Ravi Kalhan is the director of the Asthma and COPD Program at Northwestern University Feinberg School of Medicine and Northwestern Memorial Hospital.
Francesco Blasi is an Italian Medical scientist and professor. His domain of research is respiratory medicine. He has been the president of European Respiratory Society (ERS) during 2012–13. He has served as the president of Italian Respiratory Society during 2015–17. He is presently serving as one of the board of directors of University of Milan and is the professor of respiratory medicine in department pathophysiology and transplantation in University of Milan.

George Ian TownFRACP is a New Zealand respiratory scientist and health official. He was appointed the Chief Science Advisor to the New Zealand Ministry of Health in 2019.
Monica Kraft is an American scientist, medical professor and researcher. She is the System Chair of the Department of Medicine at the Icahn School of Medicine at Mount Sinai and Mount Sinai Health System. She is also the Murray M. Rosenberg Professor of Medicine.

Atul Malhotra is the director of research for pulmonary, critical care, sleep medicine, and physiology at the University of California, San Diego's Medical School. In addition, he is the Peter C. Farrell Presidential Chair and tenured professor of medicine at the same university. He is the author of almost 800 research publications, reviews, and book chapters.
Jadwiga “Wisia” A. Wedzicha is a British physician and Professor of Respiratory Medicine at the National Heart and Lung Institute. Her research has considered the causes and impact of chronic obstructive pulmonary disease. She was elected as Fellow of the UK Academy of Medical Sciences in 2013 and awarded the Helmholtz International Fellow Award.
References
- ↑ "By-Law No. 1" (PDF). Canadian Thoracic Society. 2016-04-14. Archived (PDF) from the original on 2022-09-20. Retrieved 2022-09-20.
- ↑ Ramesar, Vernon (2021-09-26). "Respiratory professionals' group seeks mandatory COVID vaccination for health-care workers". CBC News . Archived from the original on 2021-10-30. Retrieved 2022-09-20.
- ↑ "CTS urges all levels of government to mandate vaccination for health care workers" (PDF). Canadian Thoracic Society. 2021-09-22. Archived (PDF) from the original on 2021-10-27. Retrieved 2022-09-20.
- ↑ Yang, Connie L.; Hicks, Elizabeth Anne; Mitchell, Patrick; Reisman, Joe; Podgers, Delanya; Hayward, Kathleen M.; Waite, Mark; Ramsey, Clare D. (2021-11-02). "Canadian Thoracic Society 2021 Guideline update: Diagnosis and management of asthma in preschoolers, children and adults". Canadian Journal of Respiratory, Critical Care, and Sleep Medicine. 5 (6): 348–361. doi:10.1080/24745332.2021.1945887. ISSN 2474-5332. PMC 3373283 . S2CID 238704683.
- ↑ O’Donnell, Denis E; Aaron, Shawn; Bourbeau, Jean; Hernandez, Paul; Marciniuk, Darcy D; Balter, Meyer; Ford, Gordon; Gervais, Andre; Goldstein, Roger; Hodder, Rick; Kaplan, Alan; Keenan, Sean; Lacasse, Yves; Maltais, Francois; Road, Jeremy (2007). "Canadian Thoracic Society Recommendations for Management of Chronic Obstructive Pulmonary Disease – 2007 Update". Canadian Respiratory Journal. 14 (suppl b): 5B–32B. doi: 10.1155/2007/830570 . ISSN 1198-2241. PMC 2806792 . PMID 17885691.
- ↑ Fox, George A (2011). "A brief update: Current activities at the Canadian Thoracic Society". Canadian Respiratory Journal. 18 (6): 311–312. doi: 10.1155/2011/397860 . ISSN 1198-2241. PMC 3267614 .
- ↑ Gupta, Samir; Bhattacharyya, Onil K.; Brouwers, Melissa C.; Estey, Elizabeth A.; Harrison, Margaret B.; Hernandez, Paul; Palda, Valerie A.; Boulet, Louis-Philippe (2009). "Canadian Thoracic Society: Presenting a New Process for Clinical Practice Guideline Production". Canadian Respiratory Journal . 16 (6): e62–e68. doi: 10.1155/2009/397818 . PMC 2807796 . PMID 20011719.
- ↑ "Leadership and Governance". Canadian Thoracic Society. Archived from the original on 2022-09-20. Retrieved 2022-09-20.