Related Research Articles
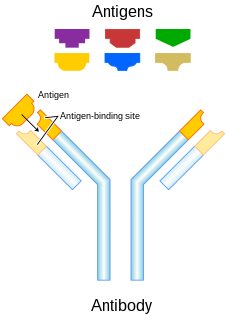
In immunology, an antigen (Ag) is a molecule or molecular structure that can bind to a specific antibody or T-cell receptor. The presence of antigens in the body may trigger an immune response. The term antigen originally referred to a substance that is an antibody generator. Antigens can be proteins, peptides, polysaccharides, lipids, nucleic acids, or other biomolecules.

Natural killer cells, also known as NK cells or large granular lymphocytes (LGL), are a type of cytotoxic lymphocyte critical to the innate immune system that belong to the rapidly expanding family of innate lymphoid cells (ILC) and represent 5–20% of all circulating lymphocytes in humans. The role of NK cells is analogous to that of cytotoxic T cells in the vertebrate adaptive immune response. NK cells provide rapid responses to virus-infected cell and other intracellular pathogens acting at around 3 days after infection, and respond to tumor formation. Typically, immune cells detect the major histocompatibility complex (MHC) presented on infected cell surfaces, triggering cytokine release, causing the death of the infected cell by lysis or apoptosis. NK cells are unique, however, as they have the ability to recognize and kill stressed cells in the absence of antibodies and MHC, allowing for a much faster immune reaction. They were named "natural killers" because of the notion that they do not require activation to kill cells that are missing "self" markers of MHC class 1. This role is especially important because harmful cells that are missing MHC I markers cannot be detected and destroyed by other immune cells, such as T lymphocyte cells.

Immunohistochemistry (IHC) is the most common application of immunostaining. It involves the process of selectively identifying antigens (proteins) in cells of a tissue section by exploiting the principle of antibodies binding specifically to antigens in biological tissues. IHC takes its name from the roots "immuno", in reference to antibodies used in the procedure, and "histo", meaning tissue. Albert Coons conceptualized and first implemented the procedure in 1941.

CA-125 also known as mucin 16 or MUC16 is a protein that in humans is encoded by the MUC16 gene. MUC16 is a member of the mucin family glycoproteins. CA-125 has found application as a tumor marker or biomarker that may be elevated in the blood of some patients with specific types of cancers, or other conditions that are benign.

Carcinoembryonic antigen (CEA) describes a set of highly related glycoproteins involved in cell adhesion. CEA is normally produced in gastrointestinal tissue during fetal development, but the production stops before birth. Consequently, CEA is usually present at very low levels in the blood of healthy adults. However, the serum levels are raised in some types of cancer, which means that it can be used as a tumor marker in clinical tests. Serum levels can also be elevated in heavy smokers.
Chimeric antigen receptor T cells are T cells that have been genetically engineered to produce an artificial T cell receptor for use in immunotherapy.

Cancer immunotherapy is the artificial stimulation of the immune system to treat cancer, improving on the immune system's natural ability to fight the disease. It is an application of the fundamental research of cancer immunology and a growing subspeciality of oncology.

An antigen-presenting cell (APC) or accessory cell is a cell that displays antigen bound by major histocompatibility complex (MHC) proteins on its surface; this process is known as antigen presentation. T cells may recognize these complexes using their T cell receptors (TCRs). APCs process antigens and present them to T-cells.
Monoclonal antibody therapy is a form of immunotherapy that uses monoclonal antibodies (mAbs) to bind monospecifically to certain cells or proteins. The objective is that this treatment will stimulate the patient's immune system to attack those cells. Alternatively, in radioimmunotherapy a radioactive dose localizes a target cell line, delivering lethal chemical doses. More recently antibodies have been used to bind to molecules involved in T-cell regulation to remove inhibitory pathways that block T-cell responses. This is known as immune checkpoint therapy.

Antigen KI-67 also known as Ki-67 or MKI67 is a protein that in humans is encoded by the MKI67 gene.

Cantuzumab mertansine is an antibody-drug conjugate investigated to treat colorectal cancer and other types of cancer. It is a humanized monoclonal antibody, cantuzumab (huC242) linked to a cytotoxic agent, mertansine (DM1). It was developed by ImmunoGen.

Ipilimumab, sold under the brand name Yervoy, is a monoclonal antibody medication that works to activate the immune system by targeting CTLA-4, a protein receptor that downregulates the immune system.
Zalutumumab is a fully human IgG1 monoclonal antibody (mAb) directed towards the epidermal growth factor receptor (EGFR). It is a product developed by Genmab in Utrecht, the Netherlands. Specifically, zalutumumab is designed for the treatment of squamous cell carcinoma of the head and neck (SCCHN), a type of cancer.

Tumor necrosis factor ligand superfamily member 9 also known as 4-1BB ligand or 4-1BBL or CD137L is a protein that in humans is encoded by the TNFSF9 gene.

Mucin 1, cell surface associated (MUC1), also called polymorphic epithelial mucin (PEM) or epithelial membrane antigen or EMA, is a mucin encoded by the MUC1 gene in humans. MUC1 is a glycoprotein with extensive O-linked glycosylation of its extracellular domain. Mucins line the apical surface of epithelial cells in the lungs, stomach, intestines, eyes and several other organs. Mucins protect the body from infection by pathogen binding to oligosaccharides in the extracellular domain, preventing the pathogen from reaching the cell surface. Overexpression of MUC1 is often associated with colon, breast, ovarian, lung and pancreatic cancers. Joyce Taylor-Papadimitriou identified and characterised the antigen during her work with breast and ovarian tumors.

Mertansine, also called DM1, is a thiol-containing maytansinoid that for therapeutic purposes is attached to a monoclonal antibody through reaction of the thiol group with a linker structure to create an antibody-drug conjugate (ADC).
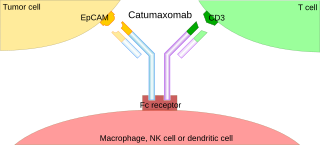
A trifunctional antibody is a monoclonal antibody with binding sites for two different antigens, typically CD3 and a tumor antigen, making it a type of bispecific monoclonal antibody. In addition, its intact Fc-part can bind to an Fc receptor on accessory cells like conventional monospecific antibodies. The net effect is that this type of drug links T cells and monocytes/macrophages, natural killer cells, dendritic cells or other Fc receptor expressing cells to the tumor cells, leading to their destruction.
Peptide-based synthetic vaccines, also called epitope vaccines, are subunit vaccines made from peptides. The peptides mimic the epitopes of the antigen that triggers direct or potent immune responses. Peptide vaccines can not only induce protection against infectious pathogens and non-infectious diseases but also be utilized as therapeutic cancer vaccines, where peptides from tumor-associated antigens are used to induce an effective anti-tumor T-cell response.

T lymphocytes are cells of the immune system that attack and destroy virus-infected cells, tumor cells and cells from transplanted organs. This occurs because each T cell is endowed with a highly specific receptor that can bind to an antigen present at the surface of another cell. The T cell receptor binds to a complex formed by a surface protein named "MHC" and a small peptide of about 9 amino-acids, which is located in a groove of the MHC molecule. This peptide can originate from a protein that remains within the cell. Whereas each T cell recognizes a single antigen, collectively the T cells are endowed with a large diversity of receptors targeted at a wide variety of antigens. T cells originate in the thymus. There a process named central tolerance eliminates the T cells that have a receptor recognizing an antigen present on normal cells of the organism. This enables the T cells to eliminate cells with "foreign" or "abnormal" antigens without harming the normal cells.
Globo H (globohexaosylceramide) is a globo-series glycosphingolipid antigen that is present on the outer membrane of some cancer cells. Globo H is not expressed in normal tissue cells, but is expressed in a number of types of cancers, including cancers of the breast, prostate, and pancreas. Globo H’s exclusivity for cancer cells makes it a target of interest for cancer therapies.
References
- ↑ Rodon, J; Garrison, M; Hammond, LA; de Bono, J; Smith, L; Forero, L; Hao, D; Takimoto, C; Lambert, JM; Pandite, L; Howard, M; Xie, H; Tolcher, AW (2008). "Cantuzumab mertansine in a three-times a week schedule: a phase I and pharmacokinetic study". Cancer Chemother Pharmacol. 62 (5): 911–9. doi:10.1007/s00280-007-0672-8. PMID 18301896. S2CID 5829870.
- ↑ A Phase I Study of Cantuzumab Mertansine Administered as a Single Intravenous Infusion Once Weekly in Patients with Advanced Solid Tumors. Helft et al. 2004