Related Research Articles

Migraine is a genetically influenced complex neurological disorder characterized by episodes of moderate-to-severe headache, most often unilateral and generally associated with nausea and light and sound sensitivity. Other characterizing symptoms may include nausea, vomiting, cognitive dysfunction, allodynia, and dizziness. Exacerbation of headache symptoms during physical activity is another distinguishing feature. Up to one-third of migraine sufferers experience aura: a premonitory period of sensory disturbance widely accepted to be caused by cortical spreading depression at the onset of a migraine attack. Although primarily considered to be a headache disorder, migraine is highly heterogenous in its clinical presentation and is better thought of as a spectrum disease rather than a distinct clinical entity. Disease burden can range from episodic discrete attacks, consisting of as little as several lifetime attacks, to chronic disease.

Headache, also known as cephalalgia, is the symptom of pain in the face, head, or neck. It can occur as a migraine, tension-type headache, or cluster headache. There is an increased risk of depression in those with severe headaches.

Cluster headache (CH) is a neurological disorder characterized by recurrent severe headaches on one side of the head, typically around the eye(s). There is often accompanying eye watering, nasal congestion, or swelling around the eye on the affected side. These symptoms typically last 15 minutes to 3 hours. Attacks often occur in clusters which typically last for weeks or months and occasionally more than a year.

Tension headache, also known as stress headache, or tension-type headache (TTH), is the most common type of primary headache. The pain can radiate from the lower back of the head, the neck, eyes or other muscle groups in the body typically affecting both sides of the head. Tension-type headaches account for nearly 90% of all headaches.
A medication overuse headache (MOH), also known as a rebound headache, usually occurs when painkillers are taken frequently to relieve headaches. These cases are often referred to as painkiller headaches. Rebound headaches frequently occur daily, can be very painful and are a common cause of chronic daily headache. They typically occur in patients with an underlying headache disorder such as migraine or tension-type headache that "transforms" over time from an episodic condition to chronic daily headache due to excessive intake of acute headache relief medications. MOH is a serious, disabling and well-characterized disorder, which represents a worldwide problem and is now considered the third-most prevalent type of headache. The proportion of patients in the population with Chronic Daily Headache (CDH) who overuse acute medications ranges from 18% to 33%. The prevalence of medication overuse headache (MOH) varies depending on the population studied and diagnostic criteria used. However, it is estimated that MOH affects approximately 1-2% of the general population, but its relative frequency is much higher in secondary and tertiary care.

Pain management is an aspect of medicine and health care involving relief of pain in various dimensions, from acute and simple to chronic and challenging. Most physicians and other health professionals provide some pain control in the normal course of their practice, and for the more complex instances of pain, they also call on additional help from a specific medical specialty devoted to pain, which is called pain medicine.
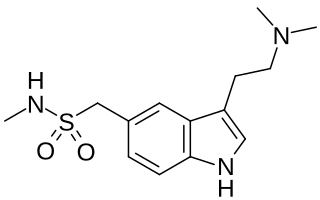
Sumatriptan, sold commonly under brand names Imitrex and Treximet among others, is a medication used to treat migraine headaches and cluster headaches. It is taken orally, intranasally, or by subcutaneous injection. Therapeutic effects generally occur within three hours.
Visual snow syndrome (VSS) is a form of visual hallucination that is characterized by the perception of small, bilateral, simultaneous, diffuse, mobile, asynchronous dots usually throughout the entire visual field, but it can be partial, and it is present in all conditions of illumination. The dots remain individual and do not clump together or change in size. Visual snow exists in one of two forms: the pulse type and the broadband type.

Nabilone, sold under the brand name Cesamet among others, is a synthetic cannabinoid with therapeutic use as an antiemetic and as an adjunct analgesic for neuropathic pain. It mimics tetrahydrocannabinol (THC), the primary psychoactive compound found naturally occurring in Cannabis.

Butalbital is a barbiturate with an intermediate duration of action. Butalbital is often combined with other medications, such as paracetamol (acetaminophen) or aspirin, for the treatment of pain and headache. The various formulations combined with codeine are FDA-approved for the treatment of tension headaches. Butalbital has the same chemical formula as talbutal but a different structure—one that presents as 5-allyl-5-isobutylbarbituric acid.
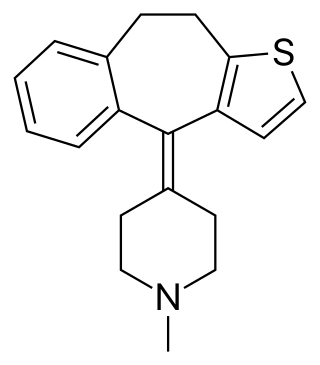
Pizotifen (INN) or pizotyline (USAN), trade name Sandomigran, is a benzocycloheptene-based drug used as a medicine, primarily as a preventive to reduce the frequency of recurrent migraine headaches.

Antimigraine drugs are medications intended to reduce the effects or intensity of migraine headache. They include drugs for the treatment of acute migraine symptoms as well as drugs for the prevention of migraine attacks.
Mixed tension migraines are also known as mixed migraines or mixed headaches. They combine characteristics of tension headaches and migraines.
Chronic headache, or chronic daily headache (CDH), is classified as experiencing fifteen or more days with a headache per month. It is estimated that chronic headaches affect "4% to 5% of the general population". Chronic headaches consist of different sub-groups, primarily categorized as chronic tension-type headaches and chronic migraine headaches. The treatments for chronic headache are vast and varied. Medicinal and non-medicinal methods exist to help patients cope with chronic headache, because chronic headaches cannot be cured. Whether pharmacological or not, treatment plans are often created on an individual basis. Multiple sources recommend multimodal treatment, which is a combination of medicinal and non-medicinal remedies. Some treatments are controversial and are still being tested for effectiveness. Suggested treatments for chronic headaches include medication, physical therapy, acupuncture, relaxation training, and biofeedback. In addition, dietary alteration and behavioral therapy or psychological therapy are other possible treatments for chronic headaches.
New daily persistent headache (NDPH) is a primary headache syndrome which can mimic chronic migraine and chronic tension-type headache. The headache is daily and unremitting from very soon after onset, usually in a person who does not have a history of a primary headache disorder. The pain can be intermittent, but lasts more than 3 months. Headache onset is abrupt and people often remember the date, circumstance and, occasionally, the time of headache onset. One retrospective study stated that over 80% of patients could state the exact date their headache began.
Vestibular migraine (VM) is vertigo with migraine, either as a symptom of migraine or as a related neurological disorder.
Preventive treatment of migraine can be an important component of migraine management. Such treatments can take many forms, including everything from surgery, taking certain drugs or nutritional supplements, to lifestyle alterations such as increased exercise and avoidance of migraine triggers.
Migralepsy is a rare condition in which a migraine is followed, within an hour period, by an epileptic seizure. Because of the similarities in signs, symptoms, and treatments of both conditions, such as the neurological basis, the psychological issues, and the autonomic distress that is created from them, they individually increase the likelihood of causing the other. However, also because of the sameness, they are often misdiagnosed for each other, as migralepsy rarely occurs.
Migraine treatment may be either prophylactic (preventive) or abortive (rescue). Prevention is better than cure, so the ideal treatment goal is to prevent migraine attacks. Because migraine is an exceedingly complex condition, there are various preventive treatments which have their effect by disrupting different links in the chain of events that occur during a migraine attack. As rescue treatments also target and disrupt different processes occurring during migraine, these are summarized, with their relative merits and demerits.
Migraines are often hereditary. It is estimated that 60% of migraine cases are caused by genetics. The role of natural selection in the development of migraines is not known. Fitness-impairing disorders, including migraines, tend to disappear as a result of natural selection, and their frequency decreases to near the rate of spontaneous mutation. However, it is estimated that migraines affect 15-20% of the population and is increasing. This could suggest that a central nervous system (CNS) susceptible to severe, intermittent headache has been linked to an important survival or reproductive advantage. Five possible evolutionary explanations exist: i) migraine as a defence mechanism, ii) migraine as a result of conflicts with other organisms, iii) migraine as a result of novel environmental factors, iv) migraine as a compromise between genetic harms and benefits, and v) headache as a design constraint. These considerations allow the treatment and prevention of migraine to be approached from an evolutionary medicine perspective.
References
- ↑ Oostendorp, R., Elvers, H., Mikolajewska, E., Roussel, N., Trijffel, E., Samwel, H., Nijs, J., Duquet, W. (2016). Cervico-cephalalgiaphobia: a subtype of phobia in patients with cervicogenic headache and neck pain? A pilot study. Journal of Manual & Manipulative Therapy, 24(4), pp. 200-209. doi: 10.1179/2042618615Y.0000000015
- ↑ Arnold, G., Reuter, U., Kinze, S., Wolf, T., & Einhäupl, K.M. (2008). Migraine with aura shows gadolinium enhancement which is reversed following prophylactic treatment. Wiley Online Library,18(9), pp. 644-646. doi: 0.1111/j.1468-2982.1998.1809644
- ↑ Larner A.J. (2005). Acupuncture use for the treatment of headache prior to neurological referral. The Journal of Headache and Pain , 6(2), pp. 97-99. doi: 10.1007/s10194-005-0160-7
- ↑ Peres, M.F.P., Mercante, J.P.P., Guendler, V.Z. et al. J Headache Pain (2007). , Cephalalgiaphobia
- ↑ American Psychiatric Association (2000). Diagnostic and Statistical Manual of Mental Disorders (4th ed., text revision). Washington, DC.
- ↑ Peres, M. F. P.; Mercante, J. P. P.; Guendler, V. Z.; Corchs, F.; Bernik, M. A.; Zukerman, E.; Silberstein, S. D. (February 2007). "Cephalalgiaphobia: a possible specific phobia of illness". The Journal of Headache and Pain. 8 (1): 56–59. doi:10.1007/s10194-007-0361-3. ISSN 1129-2369. PMC 3476114 . PMID 17361383.
- ↑ Peres, M.F.P., Mercante, J.P.P., Guendler, V.Z. et al. J Headache Pain (2007). , Cephalalgiaphobia
- ↑ Larner, A.J. (April 8, 2005). "Acupuncture use for the treatment of headache prior to neurological referral". J Headache Pain. 6 (2): 97–9. doi:10.1007/s10194-005-0160-7. PMC 3452311 . PMID 16362651.