Related Research Articles
Cerebrospinal fluid (CSF) is a clear, colorless body fluid found within the tissue that surrounds the brain and spinal cord of all vertebrates.

Veins are blood vessels in the circulatory system of humans and most other animals that carry blood toward the heart. Most veins carry deoxygenated blood from the tissues back to the heart; exceptions are those of the pulmonary and fetal circulations which carry oxygenated blood to the heart. In the systemic circulation arteries carry oxygenated blood away from the heart, and veins return deoxygenated blood to the heart.
Articles related to anatomy include:
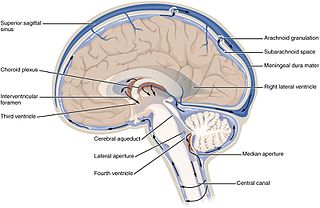
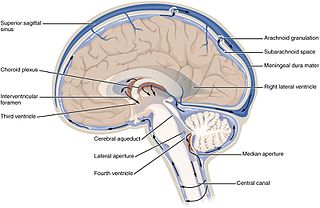
The ventricular system is a set of four interconnected cavities known as cerebral ventricles in the brain. Within each ventricle is a region of choroid plexus which produces the circulating cerebrospinal fluid (CSF). The ventricular system is continuous with the central canal of the spinal cord from the fourth ventricle, allowing for the flow of CSF to circulate.
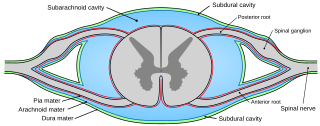
Pia mater, often referred to as simply the pia, is the delicate innermost layer of the meninges, the membranes surrounding the brain and spinal cord. Pia mater is medieval Latin meaning "tender mother". The other two meningeal membranes are the dura mater and the arachnoid mater. Both the pia and arachnoid mater are derivatives of the neural crest while the dura is derived from embryonic mesoderm. The pia mater is a thin fibrous tissue that is permeable to water and small solutes. The pia mater allows blood vessels to pass through and nourish the brain. The perivascular space between blood vessels and pia mater is proposed to be part of a pseudolymphatic system for the brain. When the pia mater becomes irritated and inflamed the result is meningitis.

In neuroanatomy, dura mater is a thick membrane made of dense irregular connective tissue that surrounds the brain and spinal cord. It is the outermost of the three layers of membrane called the meninges that protect the central nervous system. The other two meningeal layers are the arachnoid mater and the pia mater. It envelops the arachnoid mater, which is responsible for keeping in the cerebrospinal fluid. It is derived primarily from the neural crest cell population, with postnatal contributions of the paraxial mesoderm.

Cerebral circulation is the movement of blood through a network of cerebral arteries and veins supplying the brain. The rate of cerebral blood flow in an adult human is typically 750 milliliters per minute, or about 15% of cardiac output. Arteries deliver oxygenated blood, glucose and other nutrients to the brain. Veins carry "used or spent" blood back to the heart, to remove carbon dioxide, lactic acid, and other metabolic products. Because the brain would quickly suffer damage from any stoppage in blood supply, the cerebral circulatory system has safeguards including autoregulation of the blood vessels. The failure of these safeguards may result in a stroke. The volume of blood in circulation is called the cerebral blood flow. Sudden intense accelerations change the gravitational forces perceived by bodies and can severely impair cerebral circulation and normal functions to the point of becoming serious life-threatening conditions.
The emissary veins connect the extracranial venous system with the intracranial venous sinuses. They connect the veins outside the cranium to the venous sinuses inside the cranium. They drain from the scalp, through the skull, into the larger meningeal veins and dural venous sinuses.

The arachnoid mater is one of the three meninges, the protective membranes that cover the brain and spinal cord. It is so named because of its resemblance to a spider web. The arachnoid mater is a derivative of the neural crest mesoectoderm in the embryo.
The cavernous sinus within the human head is one of the dural venous sinuses creating a cavity called the lateral sellar compartment bordered by the temporal bone of the skull and the sphenoid bone, lateral to the sella turcica.
The superior sagittal sinus, within the human head, is an unpaired area along the attached margin of the falx cerebri. It allows blood to drain from the lateral aspects of anterior cerebral hemispheres to the confluence of sinuses. Cerebrospinal fluid drains through arachnoid granulations into the superior sagittal sinus and is returned to venous circulation.
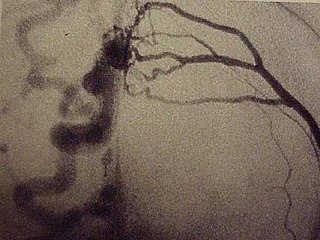
A dural arteriovenous fistula (DAVF) or malformation is an abnormal direct connection (fistula) between a meningeal artery and a meningeal vein or dural venous sinus.
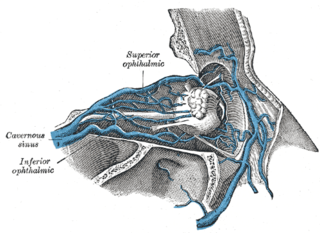
The inferior ophthalmic vein is a vein of the orbit that - together with the superior ophthalmic vein - represents the principal drainage system of the orbit. It begins from a venous network in the front of the orbit, then passes backwards through the lower orbit. It drains several structures of the orbit. It may end by splitting into two branches, one draining into the pterygoid venous plexus and the other ultimately into the cavernous sinus.
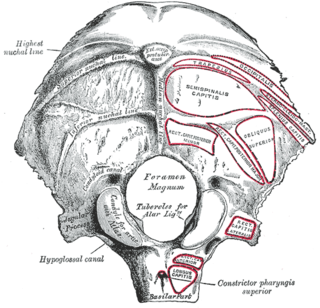
The condylar canal is a canal in the condyloid fossa of the lateral parts of occipital bone behind the occipital condyle. Resection of the rectus capitis posterior major and minor muscles reveals the bony recess leading to the condylar canal, which is situated posterior and lateral to the occipital condyle. It is immediately superior to the extradural vertebral artery, which makes a loop above the posterior C1 ring to enter the foramen magnum. The anteriomedial wall of the condylar canal thickens to join the foramen magnum rim and connect to the occipital condyle.

The internal vertebral venous plexuses lie within the vertebral canal in the epidural space, and receive tributaries from the bones and from the spinal cord.

In vertebrates, a venous plexus is a normal congregation anywhere in the body of multiple veins.
The Batson venous plexus is a network of valveless veins in the human body that connect the deep pelvic veins and thoracic veins to the internal vertebral venous plexuses. Because of their location and lack of valves, they are believed to provide a route for the spread of cancer metastases. These metastases commonly arise from cancer of the pelvic organs such as the rectum and prostate and may spread to the vertebral column or brain. The plexus is named after anatomist Oscar Vivian Batson, who first described it in 1940. Batson's plexus is part of the Cerebrospinal venous system.

Anterior spinal veins are veins that receive blood from the anterior spinal cord.

The following outline is provided as an overview of and topical guide to human anatomy:
References
- ↑ Breschet, G., Recherches anatomiques physiologiques et pathologiques sur le systáeme veineux. 1829, Paris,: Rouen fráeres. 48 p.
- 1 2 3 Batson, O.V., The Function of the Vertebral Veins and their role in the spread of metastases. Annals of Surgery, 1940. 112: p. 138-149
- ↑ Anderson, R., Diodrast studies of the vertebral and cranial venous systems to show their probable role in cerebral metastases. J Neurosurg, 1951. 8(4): p. 411-22
- 1 2 Epstein, H.M., et al., The vertebral venous plexus as a major cerebral venous outflow tract. Anesthesiology, 1970. 32(4): p. 332-7
- 1 2 Zouaoui, A. and G. Hidden, The cervical vertebral venous plexus, a drainage route for the brain. Surg Radiol Anat, 1989. 11(1): p. 79-80
- 1 2 San Millan Ruiz, D., et al., The craniocervical venous system in relation to cerebral venous drainage. AJNR Am J Neuroradiol, 2002. 23(9): p. 1500-8
- ↑ Takahashi, S., et al., Craniocervical junction venous anatomy around the suboccipital cavernous sinus: evaluation by MR imaging. Eur Radiol, 2005
- 1 2 Arnautovic, K.I., et al., The suboccipital cavernous sinus. J Neurosurg, 1997. 86(2): p. 252-62
- 1 2 3 Batson, O.V., The vertebral vein system. Caldwell lecture, 1956. Am J Roentgenol Radium Ther Nucl Med, 1957. 78(2): p. 195-212
- ↑ Herlihy, W.F., Revision of the venous system: the role of the vertebral veins. Med J Austr, 1947. 1(22): p. 661-72
- ↑ Groen, R.J., et al., Morphology of the human internal vertebral venous plexus: a cadaver study after intravenous Araldite CY 221 injection. Anat Rec, 1997. 249(2): p. 285-94
- ↑ Valdueza, J.M., et al., Postural dependency of the cerebral venous outflow. Lancet, 2000. 355(9199): p. 200-1
- ↑ Gisolf, J., et al., Human cerebral venous outflow pathway depends on posture and central venous pressure. J Physiol, 2004. 560 (Pt 1): p. 317-27
- ↑ Tobinick, E., The cerebrospinal venous system: anatomy, physiology, and clinical implications. MedGenMed, 2006. 8(1): p. 53
- ↑ Pearce, J.M.S., The craniospinal venous system. Eur Neurol, 2006. 56(2): p. 136-8
- ↑ Tubbs, R., et al., The basilar venous plexus. Clinical Anatomy, 2007. 20(7)
- 1 2 De Wyngaert, R., I. Casteels, and P. Demaerel, Orbital and anterior visual pathway infection and inflammation. Neuroradiology, 2009. 51(6): p. 385-96
- ↑ Jost, G., et al., Intradural spinal metastasis of renal cell cancer. Report of a case and review of 26 published cases. Acta Neurochir (Wien), 2009. 151(7): p. 815-21
- ↑ Morimoto, A., et al., Assessment of cervical venous blood flow and the craniocervical venus valve using ultrasound sonography. Leg Med (Tokyo), 2009. 11(1): p. 10-7
- 1 2 Nathoo, N., et al., History of the vertebral venous plexus and the significant contributions of Breschet and Batson. Neurosurgery, 2011. 69(5): p. 1007-14
- ↑ Stringer, M.D., et al., The vertebral venous plexuses: the internal veins are muscular and external veins have valves. Clin Anat, 2012. 25(5): p. 609-18
- ↑ Sugimori, K., et al., Leptomeningeal carcinomatosis from urinary bladder adenocarcinoma: a clinicopathological case study. Neuropathology, 2005. 25(1): p. 89-94
- ↑ Rajagopalan, V., et al., Bone marrow metastases from glioblastoma multiforme--A case report and review of the literature. J Neurooncol, 2005. 72(2): p. 157-61
- ↑ Tobinick, E., Kim, N., Reyzin, G. et al., Selective TNF Inhibition for Chronic Stroke and Traumatic Brain Injury: An Observational Study Involving 629 Consecutive Patients Treated with Perispinal Etanercept, CNS Drugs, 2012, 26(12):1051-1070.
- ↑ Esposito E, Cuzzocrea S. Anti-TNF therapy in the injured spinal cord. Trends Pharmacol Sci, 32(2), 107-115 (2011)
- ↑ Brochu, N., Stroke Patients Get a New Shot at Hope, Sun Sentinel, December 9, 2012, front page, Fort Lauderdale, Florida