Related Research Articles
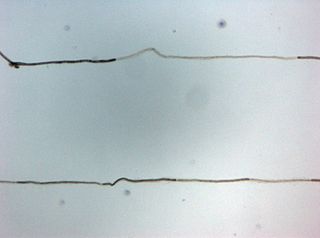
In neuroscience, an F wave is one of several motor responses which may follow the direct motor response (M) evoked by electrical stimulation of peripheral motor or mixed nerves. F-waves are the second of two late voltage changes observed after stimulation is applied to the skin surface above the distal region of a nerve, in addition to the H-reflex which is a muscle reaction in response to electrical stimulation of innervating sensory fibers. Traversal of F-waves along the entire length of peripheral nerves between the spinal cord and muscle, allows for assessment of motor nerve conduction between distal stimulation sites in the arm and leg, and related motoneurons (MN's) in the cervical and lumbosacral cord. F-waves are able to assess both afferent and efferent loops of the alpha motor neuron in its entirety. As such, various properties of F-wave motor nerve conduction are analyzed in nerve conduction studies (NCS), and often used to assess polyneuropathies, resulting from states of neuronal demyelination and loss of peripheral axonal integrity.

Lambert–Eaton myasthenic syndrome (LEMS) is a rare autoimmune disorder characterized by muscle weakness of the limbs. It is also known as myasthenic syndrome, Eaton–Lambert syndrome, and when related to cancer, carcinomatous myopathy.

Neurology is the branch of medicine dealing with the diagnosis and treatment of all categories of conditions and disease involving the nervous system, which comprises the brain, the spinal cord and the peripheral nerves. Neurological practice relies heavily on the field of neuroscience, the scientific study of the nervous system.
Clinical neurophysiology is a medical specialty that studies the central and peripheral nervous systems through the recording of bioelectrical activity, whether spontaneous or stimulated. It encompasses both research regarding the pathophysiology along with clinical methods used to diagnose diseases involving both central and peripheral nervous systems. Examinations in the clinical neurophysiology field are not limited to tests conducted in a laboratory. It is thought of as an extension of a neurologic consultation. Tests that are conducted are concerned with measuring the electrical functions of the brain, spinal cord, and nerves in the limbs and muscles. It can give the precise definition of site, the type and degree of the lesion, along with revealing the abnormalities that are in question. Due to these abilities, clinical neurophysiology is used to mainly help diagnose diseases rather than treat them.

Benign fasciculation syndrome (BFS) is characterized by fasciculation (twitching) of voluntary muscles in the body. The twitching can occur in any voluntary muscle group but is most common in the eyelids, arms, hands, fingers, legs, and feet. The tongue can also be affected. The twitching may be occasional to continuous. BFS must be distinguished from other conditions that include muscle twitches.

Polyneuropathy is damage or disease affecting peripheral nerves in roughly the same areas on both sides of the body, featuring weakness, numbness, and burning pain. It usually begins in the hands and feet and may progress to the arms and legs and sometimes to other parts of the body where it may affect the autonomic nervous system. It may be acute or chronic. A number of different disorders may cause polyneuropathy, including diabetes and some types of Guillain–Barré syndrome.

Electromyography (EMG) is a technique for evaluating and recording the electrical activity produced by skeletal muscles. EMG is performed using an instrument called an electromyograph to produce a record called an electromyogram. An electromyograph detects the electric potential generated by muscle cells when these cells are electrically or neurologically activated. The signals can be analyzed to detect abnormalities, activation level, or recruitment order, or to analyze the biomechanics of human or animal movement. Needle EMG is an electrodiagnostic medicine technique commonly used by neurologists. Surface EMG is a non-medical procedure used to assess muscle activation by several professionals, including physiotherapists, kinesiologists and biomedical engineers. In computer science, EMG is also used as middleware in gesture recognition towards allowing the input of physical action to a computer as a form of human-computer interaction.

A nerve conduction study (NCS) is a medical diagnostic test commonly used to evaluate the function, especially the ability of electrical conduction, of the motor and sensory nerves of the human body. These tests may be performed by medical specialists such as clinical neurophysiologists, physical therapists, physiatrists, and neurologists who subspecialize in electrodiagnostic medicine. In the United States, neurologists and physiatrists receive training in electrodiagnostic medicine (performing needle electromyography as part of residency training and, in some cases, acquire additional expertise during a fellowship in clinical neurophysiology, electrodiagnostic medicine, or neuromuscular medicine. Outside the US, clinical neurophysiologists learn needle EMG and NCS testing.
Proximal diabetic neuropathy, also known as diabetic amyotrophy, is a complication of diabetes mellitus that affects the nerves that supply the thighs, hips, buttocks and/or lower legs. Proximal diabetic neuropathy is a type of diabetic neuropathy characterized by muscle wasting, weakness, pain, or changes in sensation/numbness of the leg. It is caused by damage to the nerves of the lumbosacral plexus.
Chronic inflammatory demyelinating polyneuropathy (CIDP) is an acquired autoimmune disease of the peripheral nervous system characterized by progressive weakness and impaired sensory function in the legs and arms. The disorder is sometimes called chronic relapsing polyneuropathy (CRP) or chronic inflammatory demyelinating polyradiculoneuropathy. CIDP is closely related to Guillain–Barré syndrome and it is considered the chronic counterpart of that acute disease. Its symptoms are also similar to progressive inflammatory neuropathy. It is one of several types of neuropathy.

Familial amyloid polyneuropathy, also called transthyretin-related hereditary amyloidosis, transthyretin amyloidosis abbreviated also as ATTR, or Corino de Andrade's disease, is an autosomal dominant neurodegenerative disease. It is a form of amyloidosis, and was first identified and described by Portuguese neurologist Mário Corino da Costa Andrade, in 1952. FAP is distinct from senile systemic amyloidosis (SSA), which is not inherited, and which was determined to be the primary cause of death for 70% of supercentenarians who have been autopsied. FAP can be ameliorated by liver transplantation.
Critical illness polyneuropathy (CIP) and critical illness myopathy (CIM) are overlapping syndromes of diffuse, symmetric, flaccid muscle weakness occurring in critically ill patients and involving all extremities and the diaphragm with relative sparing of the cranial nerves. CIP and CIM have similar symptoms and presentations and are often distinguished largely on the basis of specialized electrophysiologic testing or muscle and nerve biopsy. The causes of CIP and CIM are unknown, though they are thought to be a possible neurological manifestation of systemic inflammatory response syndrome. Corticosteroids and neuromuscular blocking agents, which are widely used in intensive care, may contribute to the development of CIP and CIM, as may elevations in blood sugar, which frequently occur in critically ill patients.

Pronator teres syndrome is a compression neuropathy of the median nerve at the elbow. It is rare compared to compression at the wrist or isolated injury of the anterior interosseous branch of the median nerve.
Clinical Electrophysiological Testing is based on techniques derived from electrophysiology used for the clinical diagnosis of patients. There are many processes that occur in the body which produce electrical signals that can be detected. Depending on the location and the source of these signals, distinct methods and techniques have been developed to properly target them.
Electromyoneurography (EMNG) is the combined use of electromyography and electroneurography This technique allows for the measurement of a peripheral nerve's conduction velocity upon stimulation (electroneurography) alongside electrical recording of muscular activity (electromyography). Their combined use proves to be clinically relevant by allowing for both the source and location of a particular neuromuscular disease to be known, and for more accurate diagnoses.
Electrodiagnosis (EDX) is a method of medical diagnosis that obtains information about diseases by passively recording the electrical activity of body parts or by measuring their response to external electrical stimuli. The most widely used methods of recording spontaneous electrical activity are various forms of electrodiagnostic testing (electrography) such as electrocardiography (ECG), electroencephalography (EEG), and electromyography (EMG). Electrodiagnostic medicine is a medical subspecialty of neurology, clinical neurophysiology, cardiology, and physical medicine and rehabilitation. Electrodiagnostic physicians apply electrophysiologic techniques, including needle electromyography and nerve conduction studies to diagnose, evaluate, and treat people with impairments of the neurologic, neuromuscular, and/or muscular systems. The provision of a quality electrodiagnostic medical evaluation requires extensive scientific knowledge that includes anatomy and physiology of the peripheral nerves and muscles, the physics and biology of the electrical signals generated by muscle and nerve, the instrumentation used to process these signals, and techniques for clinical evaluation of diseases of the peripheral nerves and sensory pathways.

Michael Jeffrey Aminoff is a clinical neurologist and neurophysiologist whose later clinical work focused on treating Parkinson's disease and related movement disorders. He retired in 2022 and lives in San Francisco, California.
Edward Lambert was an American neurophysiologist, best known for his description of the Lambert–Eaton myasthenic syndrome and regarded as one of the founders of electromyography.
Shin Joong Oh is a South Korean and American physician who is Distinguished Professor of Neurology Emeritus at The University of Alabama at Birmingham in the United States. Oh is a clinician, researcher, and educator known for his contributions to the fields of neurology and electrodiagnostic medicine, particularly electromyography. He retired in 2014.
Zachary London is an American scientist. He is the James W. Albers Collegiate Professor of Neurology at the University of Michigan and program director of the neurology residency at the University of Michigan. He specializes in neuromuscular disease and electromyography. He has been celebrated for his innovative approach to interactive educational tools, and received the American Academy of Neurology A. B. Baker Award for Lifetime Achievement in Neurology Education in 2023.
References
- ↑ Bolton; Gilbert; Hahn; Sibbald (November 1984). "Polyneuropathy in critically ill patients". J Neurol Neurosurg Psychiatry. 47 (11): 1223–31. doi:10.1136/jnnp.47.11.1223. PMC 1028091 . PMID 6094735.
- ↑ "In memory of Private Lambert Ernest Stanley Bolton"
- ↑ "Swift Current Health Unit forerunner of Medicare in Canada"
- ↑ M.G.Taylor (April 1950). "A Canadian Health Program What Are The Issues?". Can Med Assoc J . 62 (4): 393–399. PMC 1591873 . PMID 20324555.
- ↑ "The Dorothy K. Kline Memorial Award"
- ↑ C. F. Bolton, M. A. Baltzan & R. B. Baltzan (May 1971). "Effects of renal transplantation on uremic neuropathy. A clinical and electrophysiologic study". The New England Journal of Medicine . 284 (21): 1170–1175. doi:10.1056/NEJM197105272842102. PMID 4324615.
- ↑ Charles F. Bolton (July 2010). "The discovery of critical illness polyneuropathy: a memoir". The Canadian Journal of Neurological Sciences . 37 (4): 431–438. doi: 10.1017/s031716710001043x . PMID 20724249.
- ↑ David Lacomis (March 2013). "Electrophysiology of neuromuscular disorders in critical illness". Muscle & Nerve . 47 (3): 452–463. doi: 10.1002/mus.23615 . PMID 23386582. S2CID 28785197.
- ↑ Charles Francis Bolton (2004). Neurology of Breathing. Butterworth-Heinemann. pp. 9–. ISBN 978-0-7506-7491-1.
- ↑ Hahn, Angelika F.; Young, G. Bryan (2000). "Festschrift for Dr. Charles F. Bolton". Muscle & Nerve. Supplement . 9: S1–65. doi:10.1002/1097-4598(2000)999:9<::AID-MUS1>3.0.CO;2-X. PMID 11135276. S2CID 222075103.
- ↑ "AANEM Awards History" Archived February 28, 2014, at the Wayback Machine
- ↑ "ACNS Awards History