Yuma Regional Medical Center (YRMC) is a hospital in Yuma, Arizona. It began in 1958 under the name Parkview Hospital.

The COVID-19 pandemic in the United States is part of the worldwide pandemic of coronavirus disease 2019. More than 32.5 million confirmed cases have been reported since January 2020, resulting in more than 579,000 deaths, the most of any country, and the seventeenth-highest per capita worldwide. The U.S. has about one fifth of the world's cases and deaths. More Americans have died from COVID-19 than died during both World Wars and the Vietnam War combined. COVID-19 became the third-leading cause of death in the U.S. in 2020, behind heart disease and cancer. U.S. life expectancy dropped from 78.8 years in 2019 to 77.8 years in the first half of 2020.

The COVID-19 pandemic in Turkey is part of the ongoing pandemic of coronavirus disease 2019 caused by severe acute respiratory syndrome coronavirus 2.
Sukraraj Tropical and Infectious Disease Hospital, named after Shukraraj Shastri, commonly known as Teku Hospital, is a public hospital in Teku, Kathmandu. It is the only hospital in Nepal especially designated for the treatment of tropical and infectious diseases. The hospital was established in 1933. It has a 100-bed inpatient service. It has three ICU beds and six cabin beds. It is a national referral hospital which takes in patients referred from all over the country. It also provides training to medical students. Dr. Basudev Pandey is the current director of the hospital.
Shri Ramkrishna Institute of Medical Sciences and Sanaka Hospital is a private(50 Government seats) medical college located in Durgapur, West Bengal. It was established in 2015.

Flattening the curve is a public health strategy to slow down the spread of the SARS-CoV-2 virus during the COVID-19 pandemic. The curve being flattened is the epidemic curve, a visual representation of the number of infected people needing health care over time. During an epidemic, a health care system can break down when the number of people infected exceeds the capability of the health care system's ability to take care of them. Flattening the curve means slowing the spread of the epidemic so that the peak number of people requiring care at a time is reduced, and the health care system does not exceed its capacity. Flattening the curve relies on mitigation techniques such as hand washing, use of face masks and social distancing.

The COVID-19 pandemic was confirmed to have reached the U.S. state of Arizona in January 2020. On May 3, 2021, Arizona public health authorities reported 652 new cases of COVID-19 and no new deaths, bringing the state's cumulative totals since the start of the pandemic to 864,579 cases and 17,344 deaths. Arizona currently has the 7th highest per capita case rate and the 6th highest per capita COVID-19 death rate of all US states. As of May 3, 2021, 12.03% of all Arizona residents have been infected by the COVID-19 virus, as confirmed by PCR diagnostic testing.
The COVID-19 pandemic was confirmed to have reached Somalia on 16 March 2020 when the first case was confirmed in Mogadishu. The Somali Prime Minister, Hassan Ali Khaire announced that the government has set aside five million dollars to deal with the disease. The Somali Medical Association is concerned that the death toll in the country will be huge and that Somalia will not be able to recover from the economic effects due to poor working relations between central government and federal states which leads to lack of control by central government, as well and the lack of healthcare infrastructure. It has also been speculated that President Mohamed Abdullahi Mohamed may use the pandemic as an excuse to postpone elections. There have also been concerns over freedom of the press following arrests and intimidation of journalists who have been covering the pandemic in Somalia.

The COVID-19 pandemic in Aruba is part of the ongoing global viral pandemic of coronavirus disease 2019 (COVID-19), which was documented for the first time in Aruba on 13 March 2020. As of 29 May, all cases recovered. On 29 June, two new cases were discovered.
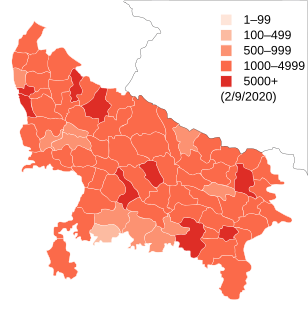
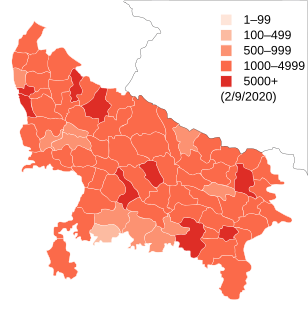
COVID-19 Pandemic spread to Uttar Pradesh in March 2020. While the World Health Organization praised the UP government for its contact tracing efforts, there were several other issues in its management of the pandemic, including under reportage of cases by the government, vaccine shortages and dismal conditions of COVID-19 hospitals.
Shortages of medical materials and other goods caused by the COVID-19 pandemic quickly became a major global issue. The matter of pandemic-related shortage has been studied in the past and has been documented in recent events. On the medical side, shortages of personal protective equipment such as medical masks, gloves, face shields, and sanitizing products, were also joined by shortages of more advanced devices such as hospital beds, Intensive care unit (ICU) beds, oxygen therapy equipment, ventilators, and ECMO devices. Human resources, especially in terms of medical staff, may be drained by the overwhelming extent of the epidemic and associated workload, together with losses by contamination, isolation, sickness, or mortality among health care workers. Territories are differently equipped to face the pandemic. Various emergency measures have been taken to ramp up equipment levels such as purchases, while calls for donations, local 3D makers, volunteer staffing, mandatory draft, or seizure of stocks and factory lines have also occurred. Bidding wars between different countries and states over these items are reported to be a major issue, with price increases, orders seized by local government, or cancelled by selling company to be redirected to higher bidder. In some cases, medical workers have been ordered to not speak about these shortages of resources.

The NHS Nightingale Hospital London is the first of the NHS Nightingale Hospitals: temporary hospitals set up by NHS England for the COVID-19 pandemic. It is housed in the ExCeL London convention centre in East London, and has an initial capacity for 500 patients, with potential for 4,000. The hospital was rapidly planned and constructed, being formally opened on 3 April and receiving its first patients on 7 April 2020.
The COVID-19 pandemic was confirmed to have reached Somaliland in March 2020. As of 3 March 2021, there are 1581 cases and 56 deaths. 30060 tests have been conducted.

On March 17, 2020, the COVID-19 pandemic was reported to have reached the United States Navajo Nation. The virus then spread rapidly through the Navajo Nation to the point that the Navajo have a higher per capita rate of infection than any state of the United States. The population according to the 2010 United States Census was 173,667. As of 4 May 2021, the number of confirmed cases was 30,543 with 1,282 deaths.

The Hospital El Salvador is a major hospital in San Salvador, El Salvador, and is planned to be the largest hospital in Latin America. The first phase was constructed between March and June 2020 as a conversion of the International Fair and Convention Center and forms part of El Salvador's response to the COVID-19 pandemic, exclusively receiving COVID-19 patients. Originally intended to be temporary, it was announced in June 2020 that the hospital conversion would be made permanent. In its first phase, the hospital has 400 available beds, a number which is expected to increase to 2,000 total beds upon completion of phase 3 of construction.

The White House COVID-19 outbreak was a cluster of SARS-CoV-2 infections that began in September 2020 and ended in January 2021 that spread among people, including many U.S. government officials, who were in close contact during the COVID-19 pandemic in Washington, D.C. Numerous high-profile individuals were infected, including President Donald Trump, who was hospitalized for three days. At least 48 White House staff members or associates, closely working with White House personnel, tested positive for the virus. The White House resisted efforts to engage in contact tracing, leaving it unclear how many people were infected in total and what the origins of the spread were.
Howard David Krein is an American otolaryngologist, plastic surgeon, and business executive. He is an assistant professor of otolaryngology at Thomas Jefferson University and is a founding partner and co-director of Thomas Jefferson University Hospital's Facial Aesthetic and Reconstructive Center. Krein is the chief medical officer at StartUp Health, a venture capital and health technology firm. He is the husband of Ashley Biden, the daughter of United States President Joe Biden. He served on the Biden Cancer Initiative's board of directors from 2017 to 2019. Krein has advised the Joe Biden 2020 presidential campaign on its COVID-19 pandemic response in an unofficial role.

The COVID-19 Advisory Board was announced in November 2020 by then-President-elect of the United States Joe Biden as part of his presidential transition. It was co-chaired by physicians David A. Kessler, Marcella Nunez-Smith, and Vivek Murthy and comprises 13 health experts. The board was then succeeded by the White House COVID-19 Response Team upon Biden's presidency.
On the night of 24 to 25 April 2021, a fire at the Ibn al-Khatib hospital in Baghdad, Iraq, left at least 82 people dead and 110 others injured. The fire was started by the explosion of oxygen tanks designated for COVID-19 patients. A lack of fire detection and suppression systems contributed to the spread of the fire, and many died as a result of being taken off their ventilators to escape the fire. The disaster led to calls for accountability, and the Minister for Health, Hassan al-Tamimi, was suspended by Prime Minister Mustafa al-Kadhimi the following day.