Methadone, sold under the brand names Dolophine and Methadose among others, is a synthetic opioid agonist used for chronic pain and also for opioid use disorder. It is used to treat chronic pain, and it is also used to treat addiction to heroin or other opioids. Prescribed for daily use, the medicine relieves cravings and removes withdrawal symptoms. Withdrawal management using methadone can be accomplished in less than a month, or it may be done gradually over a longer period of time, or simply maintained for the rest of the patient's life. While a single dose has a rapid effect, maximum effect can take up to five days of use. After long-term use, in people with normal liver function, effects last 8 to 36 hours. Methadone is usually taken by mouth and rarely by injection into a muscle or vein.
Oxycodone, sold under various brand names such as Roxicodone and OxyContin, is a semi-synthetic opioid used medically for treatment of moderate to severe pain. It is highly addictive and is a commonly abused drug. It is usually taken by mouth, and is available in immediate-release and controlled-release formulations. Onset of pain relief typically begins within fifteen minutes and lasts for up to six hours with the immediate-release formulation. In the United Kingdom, it is available by injection. Combination products are also available with paracetamol (acetaminophen), ibuprofen, naloxone, naltrexone, and aspirin.

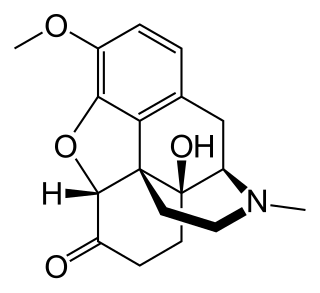
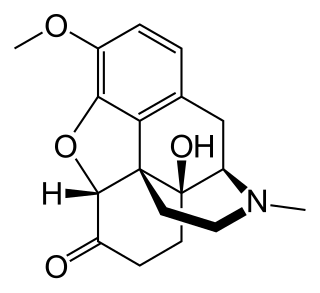
Hydromorphone, also known as dihydromorphinone, and sold under the brand name Dilaudid among others, is a morphinan opioid used to treat moderate to severe pain. Typically, long-term use is only recommended for pain due to cancer. It may be used by mouth or by injection into a vein, muscle, or under the skin. Effects generally begin within half an hour and last for up to five hours. A 2016 Cochrane review found little difference in benefit between hydromorphone and other opioids for cancer pain.

Pain management is an aspect of medicine and health care involving relief of pain in various dimensions, from acute and simple to chronic and challenging. Most physicians and other health professionals provide some pain control in the normal course of their practice, and for the more complex instances of pain, they also call on additional help from a specific medical specialty devoted to pain, which is called pain medicine.
Drug withdrawal, drug withdrawal syndrome, or substance withdrawal syndrome, is the group of symptoms that occur upon the abrupt discontinuation or decrease in the intake of pharmaceutical or recreational drugs.

Opioids are a class of drugs that derive from, or mimic, natural substances found in the opium poppy plant. Opioids work in the brain to produce a variety of effects, including pain relief. As a class of substances, they act on opioid receptors to produce morphine-like effects.

Carisoprodol, sold under the brand name Soma among others, is a medication used for musculoskeletal pain. Use is only approved for up to three weeks. Effects generally begin within half an hour and last for up to six hours. It is taken orally.

Opioid use disorder (OUD) is a substance use disorder characterized by cravings for opioids, continued use despite physical and/or psychological deterioration, increased tolerance with use, and withdrawal symptoms after discontinuing opioids. Opioid withdrawal symptoms include nausea, muscle aches, diarrhea, trouble sleeping, agitation, and a low mood. Addiction and dependence are important components of opioid use disorder.

Buprenorphine, sold under the brand name Subutex among others, is an opioid used to treat opioid use disorder, acute pain, and chronic pain. It can be used under the tongue (sublingual), in the cheek (buccal), by injection, as a skin patch (transdermal), or as an implant. For opioid use disorder, it is typically started when withdrawal symptoms have begun and for the first two days of treatment under direct observation of a health-care provider.

Sufentanil, sold under the brand names Dsuvia and Sufenta, is a synthetic opioid analgesic drug approximately 5 to 10 times as potent as its parent drug, fentanyl, and 500 times as potent as morphine. Structurally, sufentanil differs from fentanyl through the addition of a methoxymethyl group on the piperidine ring, and the replacement of the phenyl ring by thiophene. Sufentanil first was synthesized at Janssen Pharmaceutica in 1974.
Substance dependence, also known as drug dependence, is a biopsychological situation whereby an individual's functionality is dependent on the necessitated re-consumption of a psychoactive substance because of an adaptive state that has developed within the individual from psychoactive substance consumption that results in the experience of withdrawal and that necessitates the re-consumption of the drug. A drug addiction, a distinct concept from substance dependence, is defined as compulsive, out-of-control drug use, despite negative consequences. An addictive drug is a drug which is both rewarding and reinforcing. ΔFosB, a gene transcription factor, is now known to be a critical component and common factor in the development of virtually all forms of behavioral and drug addictions, but not dependence.

An opioid antagonist, or opioid receptor antagonist, is a receptor antagonist that acts on one or more of the opioid receptors.
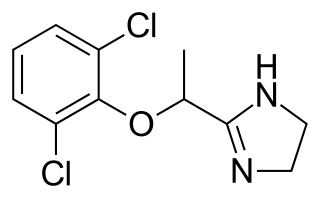
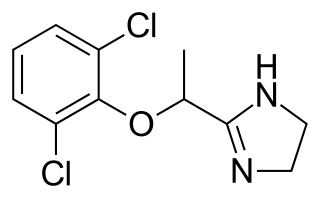
Lofexidine, sold under the brand name Lucemyra among others, is a medication historically used to treat high blood pressure; today, it is more commonly used to help with the physical symptoms of opioid withdrawal. It is taken by mouth. It is an α2A adrenergic receptor agonist. It was approved for use by the Food and Drug Administration in the United States in 2018.
An equianalgesic chart is a conversion chart that lists equivalent doses of analgesics. Equianalgesic charts are used for calculation of an equivalent dose between different analgesics. Tables of this general type are also available for NSAIDs, benzodiazepines, depressants, stimulants, anticholinergics and others.

An opioid overdose is toxicity due to excessive consumption of opioids, such as morphine, codeine, heroin, fentanyl, tramadol, and methadone. This preventable pathology can be fatal if it leads to respiratory depression, a lethal condition that can cause hypoxia from slow and shallow breathing. Other symptoms include small pupils, and unconsciousness, however its onset can depend on the method of ingestion, the dosage and individual risk factors. Although there were over 110,000 deaths in 2017 due to opioids, individuals who survived also faced adverse complications, including permanent brain damage.
Neonatal withdrawal or neonatal abstinence syndrome (NAS) or neonatal opioid withdrawal syndrome (NOWS) is a withdrawal syndrome of infants after birth caused by in utero exposure to drugs of dependence, most commonly opioids. Common signs and symptoms include tremors, irritability, vomiting, diarrhea, and fever. NAS is primarily diagnosed with a detailed medication history and scoring systems. First-line treatment should begin with non-medication interventions to support neonate growth, though medication interventions may be used in certain situations.

Buprenorphine/naloxone, sold under the brand name Suboxone among others, is a fixed-dose combination medication that includes buprenorphine and naloxone. It is used to treat opioid use disorder, and reduces the mortality of opioid use disorder by 50%. It relieves cravings to use and withdrawal symptoms. Buprenorphine/naloxone is available for use in two different forms, under the tongue or in the cheek.

Opioid withdrawal is a set of symptoms arising from the sudden withdrawal or reduction of opioids where previous usage has been heavy and prolonged. Signs and symptoms of withdrawal can include drug craving, anxiety, restless legs, nausea, vomiting, diarrhea, sweating, and an increased heart rate. Opioid use triggers a rapid adaptation in cellular signalling pathways that means, when rapidly withdrawn, there can be adverse physiological effects. All opioids, both recreational drugs and medications, when reduced or stopped, can lead to opioid withdrawal symptoms. When withdrawal symptoms are due to recreational opioid use, the term opioid use disorder is used, whereas when due to prescribed medications, the term prescription opioid use disorder is used. Opioid withdrawal can be helped by the use of opioid replacement therapy, and symptoms may be relieved by the use of medications including lofexidine and clonidine.
Opioid agonist therapy (OAT) is a treatment in which prescribed opioid agonists are given to patients who live with Opioid use disorder (OUD). The benefits of this treatment include a more manageable withdrawal experience, cognitive improvement, and lower HIV transmission. The length of OAT varies from one individual to another based on their physiology, environmental surroundings, and quality of life.

Prescription drug addiction is the chronic, repeated use of a prescription drug in ways other than prescribed for, including using someone else’s prescription. A prescription drug is a pharmaceutical drug that may not be dispensed without a legal medical prescription. Drugs in this category are supervised due to their potential for misuse and substance use disorder. The classes of medications most commonly abused are opioids, central nervous system (CNS) depressants and central nervous stimulants. In particular, prescription opioid is most commonly abused in the form of prescription analgesics.