Osteoporosis is a systemic skeletal disorder characterized by low bone mass, micro architectural deterioration of bone tissue leading to bone fragility, and consequent increase in fracture risk. It is the most common reason for a broken bone among the elderly. Bones that commonly break include the vertebrae in the spine, the bones of the forearm, and the hip. Until a broken bone occurs there are typically no symptoms. Bones may weaken to such a degree that a break may occur with minor stress or spontaneously. After a broken bone, chronic pain and a decreased ability to carry out normal activities may occur.

Dual-energy X-ray absorptiometry is a means of measuring bone mineral density (BMD) using spectral imaging. Two X-ray beams, with different energy levels, are aimed at the patient's bones. When soft tissue absorption is subtracted out, the bone mineral density (BMD) can be determined from the absorption of each beam by bone. Dual-energy X-ray absorptiometry is the most widely used and most thoroughly studied bone density measurement technology.

Paget's disease of bone is a condition involving cellular remodeling and deformity of one or more bones. The affected bones show signs of dysregulated bone remodeling at the microscopic level, specifically excessive bone breakdown and subsequent disorganized new bone formation. These structural changes cause the bone to weaken, which may result in deformity, pain, fracture or arthritis of associated joints.
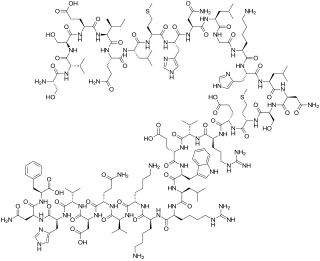
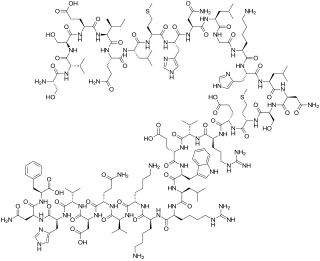
Teriparatide is a form of parathyroid hormone consisting of the first (N-terminus) 34 amino acids, which is the bioactive portion of the hormone. It is an effective anabolic agent used in the treatment of some forms of osteoporosis. It is also occasionally used off-label to speed fracture healing. Teriparatide is identical to a portion of human parathyroid hormone (PTH) and intermittent use activates osteoblasts more than osteoclasts, which leads to an overall increase in bone.

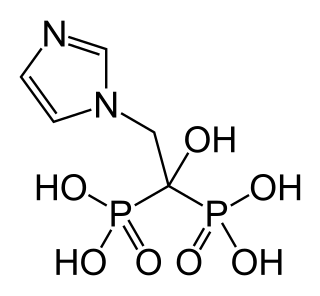
Alendronic acid, sold under the brand name Fosamax among others, is a bisphosphonate medication used to treat osteoporosis and Paget's disease of bone. It is taken by mouth. Use is often recommended together with vitamin D, calcium supplementation, and lifestyle changes.
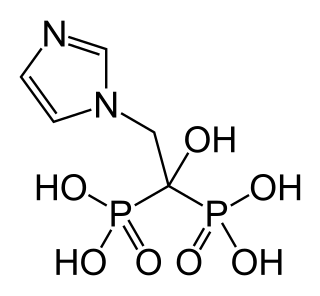
Zoledronic acid, also known as zoledronate, is a medication used to treat a number of bone diseases. These include osteoporosis, high blood calcium due to cancer, bone breakdown due to cancer, and Paget’s disease of bone. It is given by injection into a vein.

Bone density, or bone mineral density (BMD), is the amount of bone mineral in bone tissue. The concept is of mass of mineral per volume of bone, although clinically it is measured by proxy according to optical density per square centimetre of bone surface upon imaging. Bone density measurement is used in clinical medicine as an indirect indicator of osteoporosis and fracture risk. It is measured by a procedure called densitometry, often performed in the radiology or nuclear medicine departments of hospitals or clinics. The measurement is painless and non-invasive and involves low radiation exposure. Measurements are most commonly made over the lumbar spine and over the upper part of the hip. The forearm may be scanned if the hip and lumbar spine are not accessible.

Quantitative computed tomography (QCT) is a medical technique that measures bone mineral density (BMD) using a standard X-ray Computed Tomography (CT) scanner with a calibration standard to convert Hounsfield Units (HU) of the CT image to bone mineral density values. Quantitative CT scans are primarily used to evaluate bone mineral density at the lumbar spine and hip.
Relative energy deficiency in sport (RED-S) is a syndrome in which disordered eating, amenorrhoea/oligomenorrhoea, and decreased bone mineral density are present. It is caused by eating too little food to support the amount of energy being expended by an athlete, often at the urging of a coach or other authority figure who believes that athletes are more likely to win competitions when they have an extremely lean body type. RED-S is a serious illness with lifelong health consequences and can potentially be fatal.

Osteonecrosis of the jaw (ONJ) is a severe bone disease (osteonecrosis) that affects the jaws. Various forms of ONJ have been described over the last 160 years, and a number of causes have been suggested in the literature.

Denosumab is a human monoclonal antibody for the treatment of osteoporosis, treatment-induced bone loss, metastases to bone, and giant cell tumor of bone.

Strontium ranelate, a strontium(II) salt of ranelic acid, is a medication for osteoporosis marketed as Protelos or Protos by Servier. Studies indicate it can also slow the course of osteoarthritis of the knee. The drug is unusual in that it both increases deposition of new bone by osteoblasts and reduces the resorption of bone by osteoclasts. It is therefore promoted as a "dual action bone agent" (DABA).
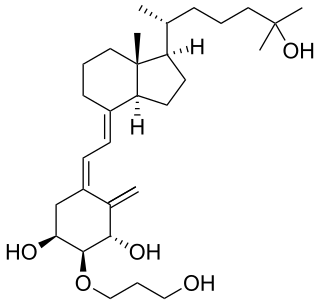
Senile osteoporosis has been recently recognized as a geriatric syndrome with a particular pathophysiology. There are different classification of osteoporosis: primary, in which bone loss is a result of aging and secondary, in which bone loss occurs from various clinical and lifestyle factors. Primary, or involuntary osteoporosis, can further be classified into Type I or Type II. Type I refers to postmenopausal osteoporosis and is caused by the deficiency of estrogen. While senile osteoporosis is categorized as an involuntary, Type II, and primary osteoporosis, which affects both men and women over the age of 70 years. It is accompanied by vitamin D deficiency, body's failure to absorb calcium, and increased parathyroid hormone.

Medication-related osteonecrosis of the jaw is progressive death of the jawbone in a person exposed to a medications known to increase the risk of disease, in the absence of a previous radiation treatment. It may lead to surgical complication in the form of impaired wound healing following oral and maxillofacial surgery, periodontal surgery, or endodontic therapy.
FRAX is a diagnostic tool used to evaluate the 10-year probability of bone fracture risk. It was developed by the University of Sheffield. FRAX integrates clinical risk factors and bone mineral density at the femoral neck to calculate the 10-year probability of hip fracture and the 10-year probability of a major osteoporotic fracture. The models used to develop the FRAX diagnostic tool were derived from studying patient populations in North America, Europe, Latin America, Asia and Australia.
Abaloparatide is a parathyroid hormone-related protein (PTHrP) analog drug used to treat osteoporosis. Like the related drug teriparatide, and unlike bisphosphonates, it is an anabolic agent.
The trabecular bone score is a measure of bone texture correlated with bone microarchitecture and a marker for the risk of osteoporosis. Introduced in 2008, its main projected use is alongside measures of bone density in better predicting fracture risk in people with metabolic bone problems.
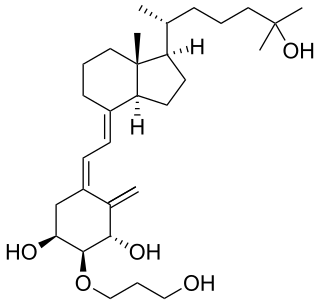
Eldecalcitol is a drug used in Japan for the treatment of osteoporosis. It is an analog of vitamin D. Osteoporosis is a common bone disease among the older generation, with an estimated prevalence of over 200 million people. This condition often results in bone fractures due to abnormally low bone mass density, and is a leading cause of disability, especially among developed countries with longer average life spans. Osteoporosis is more common in women than with men.
Dual X-ray absorptiometry and laser technique (DXL) in the area of bone density studies for osteoporosis assessment is an improvement to the DXA Technique, adding an exact laser measurement of the thickness of the region scanned. The addition of object thickness adds a third input to the two x-ray energies used by DXA, better solving the equation for bone and excluding more efficiently these soft tissues components.

Radiofrequency Echographic Multi Spectrometry (R.E.M.S.) is an innovative, non-ionizing technology for osteoporosis diagnosis and for fracture risk assessment. R.E.M.S. processes the raw, unfiltered ultrasound signals acquired during an echographic scan of the axial sites, femur and spine. The analysis is performed in the frequency domain and it is based on the comparison of the spectra obtained from the patient under examination with a series of spectral reference models, a process which allows the estimation of bone mineral density (BMD). The accuracy of this technology for BMD estimation and fracture risk evaluation has been validated in different clinical studies by comparing R.E.M.S. to DXA technology, currently considered the Gold Standard for bone mass evaluation, which partially measures bone strength.