Related Research Articles

Dementia is a syndrome associated with many neurodegenerative diseases, characterized by a general decline in cognitive abilities that affects a person's ability to perform everyday activities. This typically involves problems with memory, thinking, behavior, and motor control. Aside from memory impairment and a disruption in thought patterns, the most common symptoms of dementia include emotional problems, difficulties with language, and decreased motivation. The symptoms may be described as occurring in a continuum over several stages. Dementia ultimately has a significant effect on the individual, their caregivers, and their social relationships in general. A diagnosis of dementia requires the observation of a change from a person's usual mental functioning and a greater cognitive decline than might be caused by the normal aging process.

Cognition is the "mental action or process of acquiring knowledge and understanding through thought, experience, and the senses". It encompasses all aspects of intellectual functions and processes such as: perception, attention, thought, imagination, intelligence, the formation of knowledge, memory and working memory, judgment and evaluation, reasoning and computation, problem-solving and decision-making, comprehension and production of language. Cognitive processes use existing knowledge to discover new knowledge.
Delirium is a specific state of acute confusion attributable to the direct physiological consequence of a medical condition, effects of a psychoactive substance, or multiple causes, which usually develops over the course of hours to days. As a syndrome, delirium presents with disturbances in attention, awareness, and higher-order cognition. People with delirium may experience other neuropsychiatric disturbances including changes in psychomotor activity, disrupted sleep-wake cycle, emotional disturbances, disturbances of consciousness, or, altered state of consciousness, as well as perceptual disturbances, although these features are not required for diagnosis.

Dementia with Lewy bodies (DLB) is a type of dementia characterized by changes in sleep, behavior, cognition, movement, and regulation of automatic bodily functions. Memory loss is not always an early symptom. The disease worsens over time and is usually diagnosed when cognitive impairment interferes with normal daily functioning. Together with Parkinson's disease dementia, DLB is one of the two Lewy body dementias. It is a common form of dementia, but the prevalence is not known accurately and many diagnoses are missed. The disease was first described on autopsy by Kenji Kosaka in 1976, and he named the condition several years later.
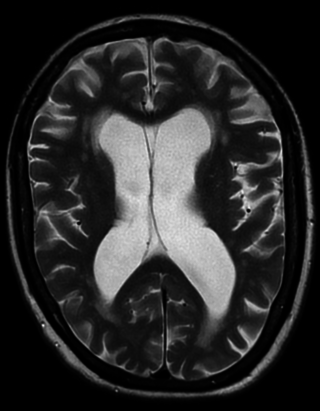
Vascular dementia is dementia caused by a series of strokes. Restricted blood flow due to strokes reduces oxygen and glucose delivery to the brain, causing cell injury and neurological deficits in the affected region. Subtypes of vascular dementia include subcortical vascular dementia, multi-infarct dementia, stroke-related dementia, and mixed dementia.

Neuropsychological tests are specifically designed tasks that are used to measure a psychological function known to be linked to a particular brain structure or pathway. Tests are used for research into brain function and in a clinical setting for the diagnosis of deficits. They usually involve the systematic administration of clearly defined procedures in a formal environment. Neuropsychological tests are typically administered to a single person working with an examiner in a quiet office environment, free from distractions. As such, it can be argued that neuropsychological tests at times offer an estimate of a person's peak level of cognitive performance. Neuropsychological tests are a core component of the process of conducting neuropsychological assessment, along with personal, interpersonal and contextual factors.

Donepezil, sold under the brand name Aricept among others, is a medication used to treat dementia of the Alzheimer's type. It appears to result in a small benefit in mental function and ability to function. Use, however, has not been shown to change the progression of the disease. Treatment should be stopped if no benefit is seen. It is taken by mouth or via a transdermal patch.
Cognitive disorders (CDs), also known as neurocognitive disorders (NCDs), are a category of mental health disorders that primarily affect cognitive abilities including learning, memory, perception, and problem-solving. Neurocognitive disorders include delirium, mild neurocognitive disorders, and major neurocognitive disorder. They are defined by deficits in cognitive ability that are acquired, typically represent decline, and may have an underlying brain pathology. The DSM-5 defines six key domains of cognitive function: executive function, learning and memory, perceptual-motor function, language, complex attention, and social cognition.
The mini–mental state examination (MMSE) or Folstein test is a 30-point questionnaire that is used extensively in clinical and research settings to measure cognitive impairment. It is commonly used in medicine and allied health to screen for dementia. It is also used to estimate the severity and progression of cognitive impairment and to follow the course of cognitive changes in an individual over time; thus making it an effective way to document an individual's response to treatment. The MMSE's purpose has been not, on its own, to provide a diagnosis for any particular nosological entity.
Cognitive impairment is an inclusive term to describe any characteristic that acts as a barrier to the cognition process or different areas of cognition. Cognition, also known as cognitive function, refers to the mental processes of how a person gains knowledge, uses existing knowledge, and understands things that are happening around them using their thoughts and senses. Cognitive impairment can be in different domains or aspects of a person's cognitive function including memory, attention span, planning, reasoning, decision-making, language, executive functioning, and visuospatial functioning. The term cognitive impairment covers many different diseases and conditions and may also be symptom or manifestation of a different underlying condition. Examples include impairments in overall intelligence, specific and restricted impairments in cognitive abilities, neuropsychological impairments, or it may describe drug-induced impairment in cognition and memory. Cognitive impairments may be short-term, progressive, or permanent.
Mild cognitive impairment (MCI) is a diagnosis that reflects an intermediate stage of cognitive impairment that is often, but not always, a transitional phase from cognitive changes in normal aging to those typically found in dementia, especially dementia due to Alzheimer's disease. MCI may include both memory and non-memory neurocognitive impairments. About 50 percent of people diagnosed with MCI have Alzheimer's disease and go on to develop Alzheimer's dementia within five years. MCI can also serve as an early indicator for other types of dementia, although MCI may also remain stable or remit. Many definitions of MCI exist. A common feature of many of these is that MCI involves cognitive impairments that are measurable but that are not significant enough to interfere with instrumental activities of daily living.
The MCI Screen is a brief neuropsychological test checking for mild cognitive impairment (MCI).
Pseudodementia is a condition that leads to cognitive and functional impairment imitating dementia that is secondary to psychiatric disorders, especially depression. Pseudodementia can develop in a wide range of neuropsychiatric disease such as depression, schizophrenia and other psychosis, mania, dissociative disorders, and conversion disorders. The presentations of pseudodementia may mimic organic dementia, but are essentially reversible on treatment and doesn't lead to actual brain degeneration. However, it has been found that some of the cognitive symptoms associated with pseudodementia can persist as residual symptoms and even transform into true neurodegenerative dementia in some cases.
Psychological therapies for dementia are starting to gain some momentum. Improved clinical assessment in early stages of Alzheimer's disease and other forms of dementia, increased cognitive stimulation of the elderly, and the prescription of drugs to slow cognitive decline have resulted in increased detection in the early stages. Although the opinions of the medical community are still apprehensive to support cognitive therapies in dementia patients, recent international studies have started to create optimism.
Elizabeth Kerr Warrington FRS is a British neuropsychologist specialised in the study of dementia. She holds a PhD in Psychology visual processing and is now an emeritus professor of clinical neuropsychology at the University College London. She formerly worked as the Head of the Department of Neuropsychology at the National Hospital for Neurology and Neurosurgery where she is also a member of the Dementia Research Centre. She was made a Fellow of the Royal Society in 1986.

Alzheimer's disease (AD) is a neurodegenerative disease that usually starts slowly and progressively worsens. It is the cause of 60–70% of cases of dementia. The most common early symptom is difficulty in remembering recent events. As the disease advances, symptoms can include problems with language, disorientation, mood swings, loss of motivation, self-neglect, and behavioral issues. As a person's condition declines, they often withdraw from family and society. Gradually, bodily functions are lost, ultimately leading to death. Although the speed of progression can vary, the average life expectancy following diagnosis is three to twelve years.
The General Practitioner Assessment of Cognition (GPCOG) is a brief screening test for cognitive impairment introduced by Brodaty et al. in 2002. It was specifically developed for the use in the primary care setting.
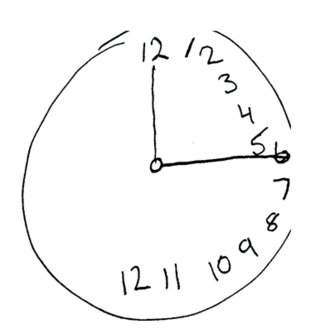
The Montreal Cognitive Assessment (MoCA) is a widely used screening assessment for detecting cognitive impairment. It was created in 1996 by Ziad Nasreddine in Montreal, Quebec. It was validated in the setting of mild cognitive impairment (MCI), and has subsequently been adopted in numerous other clinical settings. This test consists of 30 points and takes 10 minutes for the individual to complete. The original English version is performed in seven steps, which may change in some countries dependent on education and culture. The basics of this test include short-term memory, executive function, attention, focus, and more.
Although there are many physiological and psychological gender differences in humans, memory, in general, is fairly stable across the sexes. By studying the specific instances in which males and females demonstrate differences in memory, we are able to further understand the brain structures and functions associated with memory.
The Addenbrooke's Cognitive Examination (ACE) and its subsequent versions are neuropsychological tests used to identify cognitive impairment in conditions such as dementia.
References
- ↑ EL, Teng; Al., Et (2018-12-06). "The Cognitive Abilities Screening Instrument (CASI): a practical test for cross-cultural epidemiological studies of dementia". International Psychogeriatrics. 6 (1): 45–58, discussion 62. doi: 10.1017/S1041610294001602 . PMID 8054493. S2CID 25322040.
- ↑ KN, Lin; Al., Et (2018-12-06). "[Cognitive Abilities Screening Instrument, Chinese Version 2.0 (CASI C-2.0): administration and clinical application]". Acta Neurologica Taiwanica. 21 (4): 180–9. PMID 23329550.