Related Research Articles

Clinical trials are prospective biomedical or behavioral research studies on human participants designed to answer specific questions about biomedical or behavioral interventions, including new treatments and known interventions that warrant further study and comparison. Clinical trials generate data on dosage, safety and efficacy. They are conducted only after they have received health authority/ethics committee approval in the country where approval of the therapy is sought. These authorities are responsible for vetting the risk/benefit ratio of the trial—their approval does not mean the therapy is 'safe' or effective, only that the trial may be conducted.

A generic drug is a pharmaceutical drug that contains the same chemical substance as a drug that was originally protected by chemical patents. Generic drugs are allowed for sale after the patents on the original drugs expire. Because the active chemical substance is the same, the medical profile of generics is equivalent in performance compared to their performance at the time when they were patented drugs. A generic drug has the same active pharmaceutical ingredient (API) as the original, but it may differ in some characteristics such as the manufacturing process, formulation, excipients, color, taste, and packaging.
Prescription drug list prices in the United States continually are among the highest in the world. The high cost of prescription drugs became a major topic of discussion in the 21st century, leading up to the American health care reform debate of 2009, and received renewed attention in 2015. One major reason for high prescription drug prices in the United States relative to other countries is the inability of government-granted monopolies in the American health care sector to use their bargaining power to negotiate lower prices, and the American payer ends up subsidizing the world's R&D spending on drugs.

Biogen Inc. is an American multinational biotechnology company based in Cambridge, Massachusetts, United States specializing in the discovery, development, and delivery of therapies for the treatment of neurological diseases to patients worldwide. Biogen operates in Argentina, Brazil, Canada, China, France, Germany, Hungary, India, Italy, Japan, Mexico, Netherlands, Poland, Sweden, and Switzerland.
An orphan drug is a pharmaceutical agent that is developed to treat certain rare medical conditions. An orphan drug would not be profitable to produce without government assistance, due to the small population of patients affected by the conditions. The conditions that orphan drugs are used to treat are referred to as orphan diseases. The assignment of orphan status to a disease and to drugs developed to treat it is a matter of public policy that depends on the legislation of the country.

The pharmaceutical industry is an industry in medicine that discovers, develops, produces, and markets pharmaceutical drugs for use as medications to be administered to patients, with the aim to cure and prevent diseases, or alleviate symptoms. Pharmaceutical companies may deal in generic or brand medications and medical devices. They are subject to a variety of laws and regulations that govern the patenting, testing, safety, efficacy using drug testing and marketing of drugs. The global pharmaceuticals market produced treatments worth $1,228.45 billion in 2020 and showed a compound annual growth rate (CAGR) of 1.8%.
Gilead Sciences, Inc. is an American biopharmaceutical company headquartered in Foster City, California that focuses on researching and developing antiviral drugs used in the treatment of HIV/AIDS, hepatitis B, hepatitis C, influenza, and COVID-19, including ledipasvir/sofosbuvir and sofosbuvir. Gilead is a member of the NASDAQ Biotechnology Index and the S&P 500.

Medical research, also known as experimental medicine, encompasses a wide array of research, extending from "basic research", – involving fundamental scientific principles that may apply to a preclinical understanding – to clinical research, which involves studies of people who may be subjects in clinical trials. Within this spectrum is applied research, or translational research, conducted to expand knowledge in the field of medicine.
The pharmaceutical industry is one of the leading industries in the People's Republic of China, covering synthetic chemicals and drugs, prepared Chinese medicines, medical devices, apparatus and instruments, hygiene materials, packing materials, and pharmaceutical machinery. China has the second-largest pharmaceutical market in the world as of 2017 which is worth US$110 billion. China accounts for 20% of the world's population but only a small fraction of the global drug market. China's changing health-care environment is designed to extend basic health insurance to a larger portion of the population and give individuals greater access to products and services. Following the period of change, the pharmaceutical industry is expected to continue its expansion.
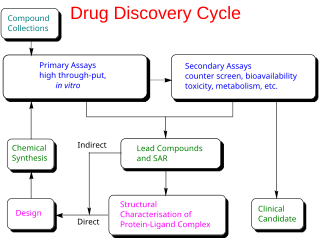
Drug development is the process of bringing a new pharmaceutical drug to the market once a lead compound has been identified through the process of drug discovery. It includes preclinical research on microorganisms and animals, filing for regulatory status, such as via the United States Food and Drug Administration for an investigational new drug to initiate clinical trials on humans, and may include the step of obtaining regulatory approval with a new drug application to market the drug. The entire process—from concept through preclinical testing in the laboratory to clinical trial development, including Phase I–III trials—to approved vaccine or drug typically takes more than a decade.

ViroPharma Incorporated was a pharmaceutical company that developed and sold drugs that addressed serious diseases treated by physician specialists and in hospital settings. The company focused on product development activities on viruses and human disease, including those caused by cytomegalovirus (CMV) and hepatitis C virus (HCV) infections. It was purchased by Shire in 2013, with Shire paying around $4.2 billion for the company in a deal that was finalized in January 2014. ViroPharma was a member of the NASDAQ Biotechnology Index and the S&P 600.
Medication costs, also known as drug costs are a common health care cost for many people and health care systems. Prescription costs are the costs to the end consumer. Medication costs are influenced by multiple factors such as patents, stakeholder influence, and marketing expenses. A number of countries including Canada, parts of Europe, and Brazil use external reference pricing as a means to compare drug prices and to determine a base price for a particular medication. Other countries use pharmacoeconomics, which looks at the cost/benefit of a product in terms of quality of life, alternative treatments, and cost reduction or avoidance in other parts of the health care system. Structures like the UK's National Institute for Health and Clinical Excellence and to a lesser extent Canada's Common Drug Review evaluate products in this way.
A drug pipeline is the set of drug candidates that an individual pharmaceutical company or the entire pharmaceutical industry collectively has under discovery or development at any given point in time. The drug pipeline is also sometimes restricted to a particular drug class or extended to mean the process of discovering drugs. The R&D pipeline involves various phases that can broadly be grouped in 4 stages: discovery, pre-clinical, clinical trials and marketing. Pharmaceutical companies usually have a number of compounds in their pipelines at any given time.
Santaris Pharma A/S was a biopharmaceutical company founded in 2003 in Copenhagen, Denmark. The company also had a branch in San Diego, California that opened in 2009. Created by a merger between Cureon and Pantheco, Santaris developed RNA-targeted medicines using a Locked Nucleic Acid (LNA) Drug Platform and Drug Development Engine.
The phases of clinical research are the stages in which scientists conduct experiments with a health intervention to obtain sufficient evidence for a process considered effective as a medical treatment. For drug development, the clinical phases start with testing for drug safety in a few human subjects, then expand to many study participants to determine if the treatment is effective. Clinical research is conducted on drug candidates, vaccine candidates, new medical devices, and new diagnostic assays.
Bad Pharma: How Drug Companies Mislead Doctors and Harm Patients is a book by the British physician and academic Ben Goldacre about the pharmaceutical industry, its relationship with the medical profession, and the extent to which it controls academic research into its own products. It was published in the UK in September 2012 by the Fourth Estate imprint of HarperCollins, and in the United States in February 2013 by Faber and Faber.
Alnylam Pharmaceuticals, Inc. is an American biopharmaceutical company focused on the discovery, development and commercialization of RNA interference (RNAi) therapeutics for genetically defined diseases. The company was founded in 2002 and is headquartered in Cambridge, Massachusetts. In 2016, Forbes included the company on its "100 Most Innovative Growth Companies" list.

Basimglurant (INN) is a negative allosteric modulator of the mGlu5 receptor which is under development by Roche and Chugai Pharmaceutical for the treatment of treatment-resistant depression and fragile X syndrome. As of November 2016, it has undergone phase II clinical trials for both of these indications.
The Tufts Center for the Study of Drug Development is an independent, academic, non-profit research center at Tufts University in Boston, dedicated to researching drug development. It was established in 1976 by American physician Louis Lasagna. The Center develops and publishes information to help researchers, regulators, and policy makers in areas related to the pharmaceutical and biotechnology industries. In any given year, approximately 55% of Tufts CSDD's operating expenses are supported by grants from the private sector and 45% from the public sector.

Ipragliflozin is a pharmaceutical drug for treatment of type 2 diabetes. Ipragliflozin, jointly developed by Astellas Pharma and Kotobuki Pharmaceutical, was approved in Japan on January 17, 2014, and in Russia on May 22, 2019.
References
- ↑ Sertkaya A, Wong HH, Jessup A, Beleche T (April 2016). "Key cost drivers of pharmaceutical clinical trials in the United States". Clinical Trials. 13 (2): 117–126. doi: 10.1177/1740774515625964 . PMID 26908540. S2CID 24308679.
- ↑ Paul SM, Mytelka DS, Dunwiddie CT, Persinger CC, Munos BH, Lindborg SR, Schacht AL (March 2010). "How to improve R&D productivity: the pharmaceutical industry's grand challenge". Nature Reviews. Drug Discovery. 9 (3): 203–214. doi: 10.1038/nrd3078 . PMID 20168317. S2CID 1299234.
- 1 2 Herper M (11 August 2013). "The Cost Of Creating A New Drug Now $5 Billion, Pushing Big Pharma To Change". Forbes, Pharma & Healthcare. Retrieved 17 July 2016.
- ↑ Wouters OJ, McKee M, Luyten J (March 2020). "Estimated Research and Development Investment Needed to Bring a New Medicine to Market, 2009-2018". JAMA. 323 (9): 844–853. doi:10.1001/jama.2020.1166. PMC 7054832 . PMID 32125404.
- ↑ Maxmen A (August 2016). "Busting the billion-dollar myth: how to slash the cost of drug development". Nature. 536 (7617): 388–390. Bibcode:2016Natur.536..388M. doi: 10.1038/536388a . PMID 27558048.
- ↑ Team T. "How Big Is Roche's R&D Expense?". Forbes. Retrieved 2020-01-14.
- ↑ Frank RG, Ginsburg PB (17 November 2017). "Pharmaceutical industry profits and research and development". Brookings. Retrieved 2020-01-14.
- ↑ Klotz L (16 January 2014). "What Is the Real Drug Development Cost for Very Small Biotech Companies?". Genetic Engineering & Biotechnology News. Retrieved March 15, 2016.
- 1 2 3 4 5 "New Drug Development Process" (PDF). California Biomedical Research Association. Archived from the original (PDF) on March 14, 2016. Retrieved March 15, 2016.
- ↑ "Animal Models in Drug Discovery". Taconic Biosciences. Retrieved 2020-01-14.
- 1 2 Herper M. "The Truly Staggering Cost Of Inventing New Drugs". Forbes. Retrieved 2016-03-15.
- ↑ Gaffney A. "FDA Publishes All User Fee Rates for Fiscal Year 2014 | RAPS". www.raps.org. Archived from the original on 2016-03-17. Retrieved 2016-03-15.
- ↑ Pérez-Rodríguez, Jorge V.; Valcarcel, Beatriz G. L. (2012-06-01). "Do product innovation and news about the R&D process produce large price changes and overreaction? The case of pharmaceutical stock prices". Applied Economics. 44 (17): 2217–2229. doi:10.1080/00036846.2011.562172. ISSN 0003-6846.
- ↑ Ben Adams (3 June 2019). "The top 10 pharma R&D budgets in 2018: Roche". FierceBiotech. Retrieved 2020-01-14.
- ↑ Pear R (1 December 2001). "Research Cost For New Drugs Said to Soar". New York Times. Retrieved 21 November 2014.
- ↑ Silverman E (20 November 2014). "What Does It Cost to Develop a New Drug? Latest Study Says $2.6 Billion". Wall Street Journal. Retrieved 21 November 2014.
- ↑ Pierson R (18 November 2014). "CORRECTED-Tufts says average new drug costs $2.6 bln to develop, critics wary". Reuters. Retrieved 21 November 2014.
- ↑ Carroll A (19 November 2014). "$2.6 Billion to Develop a Drug? New Estimate Makes Questionable Assumptions". New York Times. Retrieved 25 November 2014.
- ↑ DiMasi JA, Grabowski HG, Hansen RW (May 2016). "Innovation in the pharmaceutical industry: New estimates of R&D costs". Journal of Health Economics. 47: 20–33. doi:10.1016/j.jhealeco.2016.01.012. hdl: 10161/12742 . PMID 26928437.
- ↑ "Big pharma says drug prices reflect R&D cost. Researchers call BS". Ars Technica. 14 October 2022. Retrieved 21 October 2022.
- ↑ Wouters, Olivier J.; Berenbrok, Lucas A.; He, Meiqi; Li, Yihan; Hernandez, Inmaculada (26 September 2022). "Association of Research and Development Investments With Treatment Costs for New Drugs Approved From 2009 to 2018". JAMA Network Open. 5 (9): e2218623. doi: 10.1001/jamanetworkopen.2022.18623 . ISSN 2574-3805. PMC 9513642 . PMID 36156148.