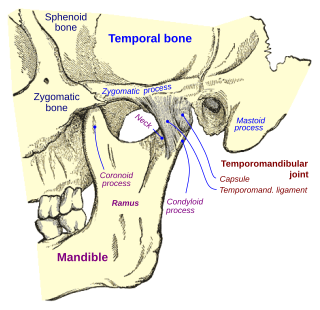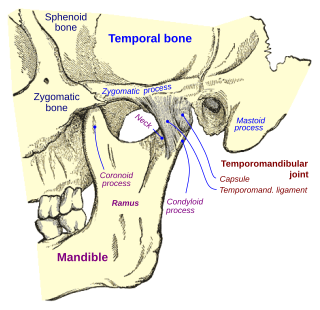
Temporomandibular joint dysfunction is an umbrella term covering pain and dysfunction of the muscles of mastication and the temporomandibular joints. The most important feature is pain, followed by restricted mandibular movement, and noises from the temporomandibular joints (TMJ) during jaw movement. Although TMD is not life-threatening, it can be detrimental to quality of life; this is because the symptoms can become chronic and difficult to manage.

Back pain is pain felt in the back. It may be classified as neck pain (cervical), middle back pain (thoracic), lower back pain (lumbar) or coccydynia based on the segment affected. The lumbar area is the most common area affected. An episode of back pain may be acute, subacute or chronic depending on the duration. The pain may be characterized as a dull ache, shooting or piercing pain or a burning sensation. Discomfort can radiate to the arms and hands as well as the legs or feet, and may include numbness or weakness in the legs and arms.
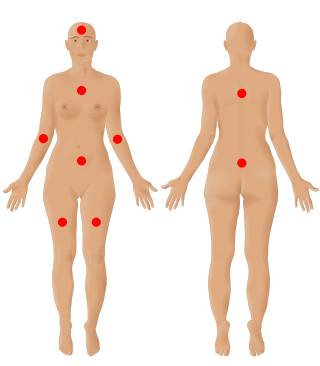
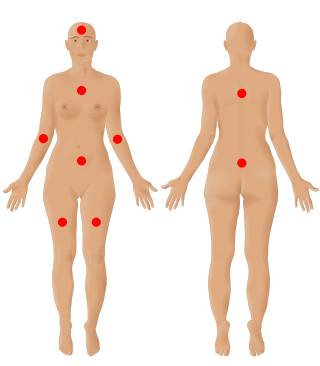
Fibromyalgia is a medical syndrome that causes chronic widespread pain, accompanied by fatigue, awakening unrefreshed, and cognitive symptoms. Other symptoms can include headaches, lower abdominal pain or cramps, and depression. People with fibromyalgia can also experience insomnia and general hypersensitivity. The cause of fibromyalgia is unknown, but is believed to involve a combination of genetic and environmental factors. Environmental factors may include psychological stress, trauma, and some infections. Since the pain appears to result from processes in the central nervous system, the condition is referred to as a "central sensitization syndrome".

Pain management is an aspect of medicine and health care involving relief of pain in various dimensions, from acute and simple to chronic and challenging. Most physicians and other health professionals provide some pain control in the normal course of their practice, and for the more complex instances of pain, they also call on additional help from a specific medical specialty devoted to pain, which is called pain medicine.

Ankylosing spondylitis (AS) is a type of arthritis from the disease spectrum of axial spondyloarthritis. It is characterized by long-term inflammation of the joints of the spine, typically where the spine joins the pelvis. With AS, eye and bowel problems—as well as back pain—may occur. Joint mobility in the affected areas sometimes worsens over time. Ankylosing spondylitis is believed to involve a combination of genetic and environmental factors. More than 90% of people affected in the UK have a specific human leukocyte antigen known as the HLA-B27 antigen. The underlying mechanism is believed to be autoimmune or autoinflammatory. Diagnosis is based on symptoms with support from medical imaging and blood tests. AS is a type of seronegative spondyloarthropathy, meaning that tests show no presence of rheumatoid factor (RF) antibodies.

Osteoarthritis (OA) is a type of degenerative joint disease that results from breakdown of joint cartilage and underlying bone. It is believed to be the fourth leading cause of disability in the world, affecting 1 in 7 adults in the United States alone. The most common symptoms are joint pain and stiffness. Usually the symptoms progress slowly over years. Other symptoms may include joint swelling, decreased range of motion, and, when the back is affected, weakness or numbness of the arms and legs. The most commonly involved joints are the two near the ends of the fingers and the joint at the base of the thumbs, the knee and hip joints, and the joints of the neck and lower back. The symptoms can interfere with work and normal daily activities. Unlike some other types of arthritis, only the joints, not internal organs, are affected.

Raynaud syndrome, also known as Raynaud's phenomenon, is a medical condition in which the spasm of small arteries causes episodes of reduced blood flow to end arterioles. Typically the fingers, and, less commonly, the toes, are involved. Rarely, the nose, ears, nipples, or lips are affected. The episodes classically result in the affected part turning white and then blue. Often, numbness or pain occurs. As blood flow returns, the area turns red and burns. The episodes typically last minutes but can last several hours. The condition is named after the physician Auguste Gabriel Maurice Raynaud, who first described it in his doctoral thesis in 1862.

Low back pain or lumbago is a common disorder involving the muscles, nerves, and bones of the back, in between the lower edge of the ribs and the lower fold of the buttocks. Pain can vary from a dull constant ache to a sudden sharp feeling. Low back pain may be classified by duration as acute, sub-chronic, or chronic. The condition may be further classified by the underlying cause as either mechanical, non-mechanical, or referred pain. The symptoms of low back pain usually improve within a few weeks from the time they start, with 40–90% of people recovered by six weeks.

Juvenile idiopathic arthritis (JIA), formerly known as juvenile rheumatoid arthritis (JRA), is the most common chronic rheumatic disease of childhood, affecting approximately 3.8 to 400 out of 100,000 children. Juvenile, in this context, refers to disease onset before 16 years of age, while idiopathic refers to a condition with no defined cause, and arthritis is inflammation within the joint.

Spondylosis is the degeneration of the vertebral column from any cause. In the more narrow sense it refers to spinal osteoarthritis, the age-related degeneration of the spinal column, which is the most common cause of spondylosis. The degenerative process in osteoarthritis chiefly affects the vertebral bodies, the neural foramina and the facet joints. If severe, it may cause pressure on the spinal cord or nerve roots with subsequent sensory or motor disturbances, such as pain, paresthesia, imbalance, and muscle weakness in the limbs.
Postherpetic neuralgia (PHN) is neuropathic pain that occurs due to damage to a peripheral nerve caused by the reactivation of the varicella zoster virus. PHN is defined as pain in a dermatomal distribution that lasts for at least 90 days after an outbreak of herpes zoster. Several types of pain may occur with PHN including continuous burning pain, episodes of severe shooting or electric-like pain, and a heightened sensitivity to gentle touch which would not otherwise cause pain or to painful stimuli. Abnormal sensations and itching may also occur.

Alcoholic polyneuropathy is a neurological disorder in which peripheral nerves throughout the body malfunction simultaneously. It is defined by axonal degeneration in neurons of both the sensory and motor systems and initially occurs at the distal ends of the longest axons in the body. This nerve damage causes an individual to experience pain and motor weakness, first in the feet and hands and then progressing centrally. Alcoholic polyneuropathy is caused primarily by chronic alcoholism; however, vitamin deficiencies are also known to contribute to its development. This disease typically occurs in chronic alcoholics who have some sort of nutritional deficiency. Treatment may involve nutritional supplementation, pain management, and abstaining from alcohol.
Indigestion, also known as dyspepsia or upset stomach, is a condition of impaired digestion. Symptoms may include upper abdominal fullness, heartburn, nausea, belching, or upper abdominal pain. People may also experience feeling full earlier than expected when eating. Indigestion is relatively common, affecting 20% of people at some point during their life, and is frequently caused by gastroesophageal reflux disease (GERD) or gastritis.
Sacroiliitis is inflammation within the sacroiliac joint. It is a feature of spondyloarthropathies, such as axial spondyloarthritis, psoriatic arthritis, reactive arthritis or arthritis related to inflammatory bowel diseases, including ulcerative colitis or Crohn's disease. It is also the most common presentation of arthritis from brucellosis.

Burning mouth syndrome (BMS) is a burning, tingling or scalding sensation in the mouth, lasting for at least four to six months, with no underlying known dental or medical cause. No related signs of disease are found in the mouth. People with burning mouth syndrome may also have a subjective xerostomia, paraesthesia, or an altered sense of taste or smell.
Greater trochanteric pain syndrome (GTPS), a form of bursitis, is inflammation of the trochanteric bursa, a part of the hip.

The signs and symptoms of multiple sclerosis (MS) encompass a wide range of neurological and physical manifestations, including vision problems, muscle weakness, coordination difficulties, and cognitive impairment, varying significantly in severity and progression among individuals.

Neurogenic claudication (NC), also known as pseudoclaudication, is the most common symptom of lumbar spinal stenosis (LSS) and describes intermittent leg pain from impingement of the nerves emanating from the spinal cord. Neurogenic means that the problem originates within the nervous system. Claudication, from Latin claudicare 'to limp', refers to painful cramping or weakness in the legs. NC should therefore be distinguished from vascular claudication, which stems from a circulatory problem rather than a neural one.

Blurred vision is an ocular symptom where vision becomes less precise and there is added difficulty to resolve fine details.
Visceral pain is pain that results from the activation of nociceptors of the thoracic, pelvic, or abdominal viscera (organs). Visceral structures are highly sensitive to distension (stretch), ischemia and inflammation, but relatively insensitive to other stimuli that normally evoke pain such as cutting or burning.