A nerve is an enclosed, cable-like bundle of nerve fibers in the peripheral nervous system.
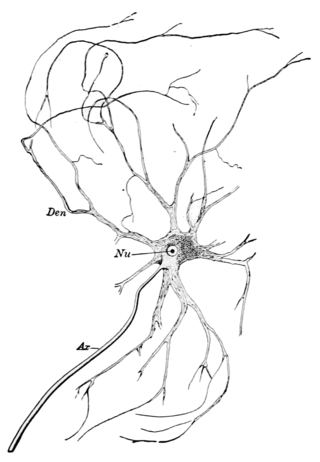
Nervous tissue, also called neural tissue, is the main tissue component of the nervous system. The nervous system regulates and controls body functions and activity. It consists of two parts: the central nervous system (CNS) comprising the brain and spinal cord, and the peripheral nervous system (PNS) comprising the branching peripheral nerves. It is composed of neurons, also known as nerve cells, which receive and transmit impulses, and neuroglia, also known as glial cells or glia, which assist the propagation of the nerve impulse as well as provide nutrients to the neurons.
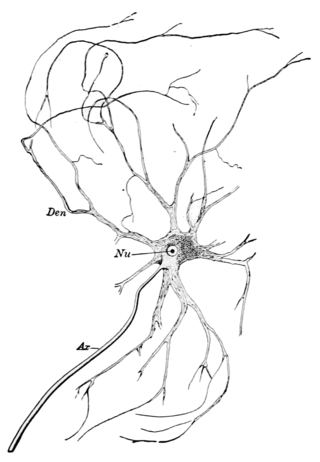
A motor nerve, or efferent nerve, is a nerve that contains exclusively efferent nerve fibers and transmits motor signals from the central nervous system (CNS) to the muscles of the body. This is different from the motor neuron, which includes a cell body and branching of dendrites, while the nerve is made up of a bundle of axons. Motor nerves act as efferent nerves which carry information out from the CNS to muscles, as opposed to afferent nerves, which transfer signals from sensory receptors in the periphery to the CNS. Efferent nerves can also connect to glands or other organs/issues instead of muscles. The vast majority of nerves contain both sensory and motor fibers and are therefore called mixed nerves.

Cryosurgery is the use of extreme cold in surgery to destroy abnormal or diseased tissue; thus, it is the surgical application of cryoablation. Cryosurgery has been historically used to treat a number of diseases and disorders, especially a variety of benign and malignant skin conditions.
Cryotherapy, sometimes known as cold therapy, is the local or general use of low temperatures in medical therapy. Cryotherapy may be used to treat a variety of tissue lesions. The most prominent use of the term refers to the surgical treatment, specifically known as cryosurgery or cryoablation. Cryosurgery is the application of extremely low temperatures to destroy abnormal or diseased tissue and is used most commonly to treat skin conditions.
Neurotmesis is part of Seddon's classification scheme used to classify nerve damage. It is the most serious nerve injury in the scheme. In this type of injury, both the nerve and the nerve sheath are disrupted. While partial recovery may occur, complete recovery is impossible.
Axonotmesis is an injury to the peripheral nerve of one of the extremities of the body. The axons and their myelin sheath are damaged in this kind of injury, but the endoneurium, perineurium and epineurium remain intact. Motor and sensory functions distal to the point of injury are completely lost over time leading to Wallerian degeneration due to ischemia, or loss of blood supply. Axonotmesis is usually the result of a more severe crush or contusion than neurapraxia.
Neuralgia is pain in the distribution of a nerve or nerves, as in intercostal neuralgia, trigeminal neuralgia, and glossopharyngeal neuralgia.
In medicine, a stinger, also called a burner or nerve pinch injury, is a neurological injury suffered by athletes, mostly in high-contact sports such as ice hockey, rugby, American football, and wrestling. The spine injury is characterized by a shooting or stinging pain that travels down one arm, followed by numbness and weakness in the parts of the arms, including the biceps, deltoid, and spinati muscles. Many athletes in contact sports have suffered stingers, but they are often unreported to medical professionals.

A brachial plexus injury (BPI), also known as brachial plexus lesion, is an injury to the brachial plexus, the network of nerves that conducts signals from the spinal cord to the shoulder, arm and hand. These nerves originate in the fifth, sixth, seventh and eighth cervical (C5–C8), and first thoracic (T1) spinal nerves, and innervate the muscles and skin of the chest, shoulder, arm and hand.

Radiofrequency ablation (RFA), also called fulguration, is a medical procedure in which part of the electrical conduction system of the heart, tumor or other dysfunctional tissue is ablated using the heat generated from medium frequency alternating current. RFA is generally conducted in the outpatient setting, using either local anesthetics or twilight anesthesia. When it is delivered via catheter, it is called radiofrequency catheter ablation.

Cryoablation is a process that uses extreme cold to destroy tissue. Cryoablation is performed using hollow needles (cryoprobes) through which cooled, thermally conductive fluids are circulated. Cryoprobes are positioned adjacent to the target in such a way that the freezing process will destroy the diseased tissue. Once the probes are in place, the attached cryogenic freezing unit removes heat from ("cools") the tip of the probe and by extension from the surrounding tissues.
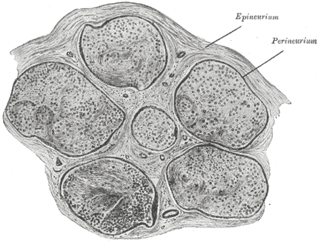
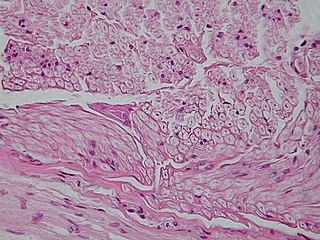
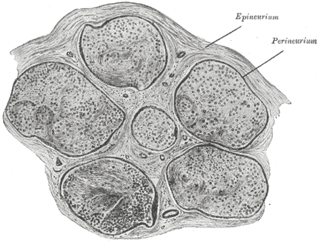
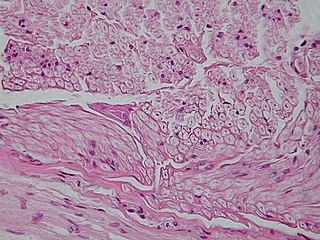
The endoneurium is a layer of delicate connective tissue around the myelin sheath of each myelinated nerve fiber in the peripheral nervous system. Its component cells are called endoneurial cells. The endoneuria with their enclosed nerve fibers are bundled into groups called nerve fascicles, each fascicle within its own protective sheath called a perineurium. In sufficiently large nerves multiple fascicles, each with its blood supply and fatty tissue, may be bundled within yet another sheath, the epineurium.

Nerve injury is an injury to a nerve. There is no single classification system that can describe all the many variations of nerve injuries. In 1941, Seddon introduced a classification of nerve injuries based on three main types of nerve fiber injury and whether there is continuity of the nerve. Usually, however, nerve injuries are classified in five stages, based on the extent of damage to both the nerve and the surrounding connective tissue, since supporting glial cells may be involved.
Neuroregeneration involves the regrowth or repair of nervous tissues, cells or cell products. Neuroregenerative mechanisms may include generation of new neurons, glia, axons, myelin, or synapses. Neuroregeneration differs between the peripheral nervous system (PNS) and the central nervous system (CNS) by the functional mechanisms involved, especially in the extent and speed of repair. When an axon is damaged, the distal segment undergoes Wallerian degeneration, losing its myelin sheath. The proximal segment can either die by apoptosis or undergo the chromatolytic reaction, which is an attempt at repair. In the CNS, synaptic stripping occurs as glial foot processes invade the dead synapse.

Group C nerve fibers are one of three classes of nerve fiber in the central nervous system (CNS) and peripheral nervous system (PNS). The C group fibers are unmyelinated and have a small diameter and low conduction velocity, whereas Groups A and B are myelinated. Group C fibers include postganglionic fibers in the autonomic nervous system (ANS), and nerve fibers at the dorsal roots. These fibers carry sensory information.
Dental anesthesia is the application of anesthesia to dentistry. It includes local anesthetics, sedation, and general anesthesia.

Nerve injury classification assists in prognosis and determination of treatment strategy for nerve injuries. Classification was described by Seddon in 1943 and by Sunderland in 1951. In the lowest degree of nerve the nerve remains intact, but signaling ability is damaged, termed neurapraxia. In the second degree the axon is damaged, but the surrounding connecting tissue remains intact – axonotmesis. The last degree, in which both the axon and connective tissue are damaged, is called neurotmesis.
Nerve allotransplantation is the transplantation of a nerve to a receiver from a donor of the same species. For example, nerve tissue is transplanted from one person to another. Allotransplantation is a commonly used type of transplantation of which nerve repair is one specific aspect.

Nerve entrapment involves a cascade of physiological changes caused by compression and tension. Some of these changes are irreversible. The magnitude and duration of the forces determines the extent of injury. In the acute form, mechanical injury and metabolic blocks impede nerve function. In the chronic form, there is a sequence of changes starting with a breakdown of the blood-nerve-barrier, followed by edema with connective tissue changes, followed by diffuse demyelination, and finally followed by axonmetesis. The injury will often be a mixed lesion where mild/moderate compression is a combination of a metabolic block and neuropraxia, while severe compression combines elements of neuropraxia and axonmetesis.