Related Research Articles

Pancreatitis is a condition characterized by inflammation of the pancreas. The pancreas is a large organ behind the stomach that produces digestive enzymes and a number of hormones. There are two main types: acute pancreatitis, and chronic pancreatitis.
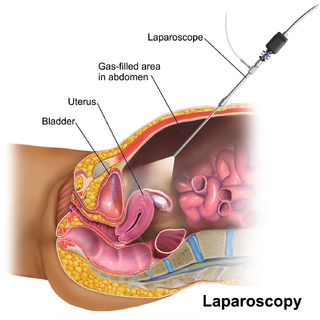
Laparoscopy is an operation performed in the abdomen or pelvis using small incisions with the aid of a camera. The laparoscope aids diagnosis or therapeutic interventions with a few small cuts in the abdomen.

Appendicitis is inflammation of the appendix. Symptoms commonly include right lower abdominal pain, nausea, vomiting, and decreased appetite. However, approximately 40% of people do not have these typical symptoms. Severe complications of a ruptured appendix include widespread, painful inflammation of the inner lining of the abdominal wall and sepsis.

In vertebrates, the gallbladder, also known as the cholecyst, is a small hollow organ where bile is stored and concentrated before it is released into the small intestine. In humans, the pear-shaped gallbladder lies beneath the liver, although the structure and position of the gallbladder can vary significantly among animal species. It receives and stores bile, produced by the liver, via the common hepatic duct, and releases it via the common bile duct into the duodenum, where the bile helps in the digestion of fats.
Cholecystitis is inflammation of the gallbladder. Symptoms include right upper abdominal pain, pain in the right shoulder, nausea, vomiting, and occasionally fever. Often gallbladder attacks precede acute cholecystitis. The pain lasts longer in cholecystitis than in a typical gallbladder attack. Without appropriate treatment, recurrent episodes of cholecystitis are common. Complications of acute cholecystitis include gallstone pancreatitis, common bile duct stones, or inflammation of the common bile duct.

Cholecystectomy is the surgical removal of the gallbladder. Cholecystectomy is a common treatment of symptomatic gallstones and other gallbladder conditions. In 2011, cholecystectomy was the eighth most common operating room procedure performed in hospitals in the United States. Cholecystectomy can be performed either laparoscopically, or via an open surgical technique.

Acute pancreatitis (AP) is a sudden inflammation of the pancreas. Causes, in order of frequency, include: 1) a gallstone impacted in the common bile duct beyond the point where the pancreatic duct joins it; 2) heavy alcohol use; 3) systemic disease; 4) trauma; 5) and, in minors, mumps. Acute pancreatitis may be a single event; it may be recurrent; or it may progress to chronic pancreatitis.

Gastrointestinal diseases refer to diseases involving the gastrointestinal tract, namely the esophagus, stomach, small intestine, large intestine and rectum, and the accessory organs of digestion, the liver, gallbladder, and pancreas.

Common bile duct stone, also known as choledocholithiasis, is the presence of gallstones in the common bile duct (CBD). This condition can cause jaundice and liver cell damage. Treatments include choledocholithotomy and endoscopic retrograde cholangiopancreatography (ERCP).

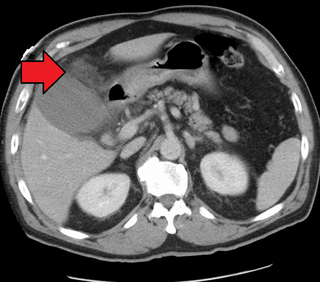
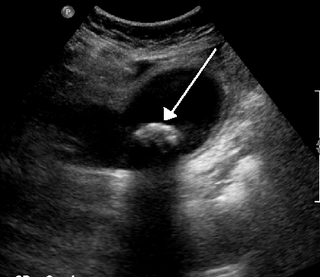
A pancreatic pseudocyst is a circumscribed collection of fluid rich in pancreatic enzymes, blood, and non-necrotic tissue, typically located in the lesser sac of the abdomen. Pancreatic pseudocysts are usually complications of pancreatitis, although in children they frequently occur following abdominal trauma. Pancreatic pseudocysts account for approximately 75% of all pancreatic masses.

Pseudocysts are like cysts, but lack epithelial or endothelial cells. Initial management consists of general supportive care. Symptoms and complications caused by pseudocysts require surgery. Computed tomography (CT) scans are used for initial imaging of cysts, and endoscopic ultrasounds are used in differentiating between cysts and pseudocysts. Endoscopic drainage is a popular and effective method of treating pseudocysts.
Pancreatic divisum is a congenital anomaly in the anatomy of the ducts of the pancreas in which a single pancreatic duct is not formed, but rather remains as two distinct dorsal and ventral ducts. Most individuals with pancreas divisum remain without symptoms or complications. A minority of people with pancreatic divisum may develop episodes of abdominal pain, nausea or vomiting due to acute or chronic pancreatitis. The presence of pancreas divisum is usually identified with cross sectional diagnostic imaging, such as MRI or computed tomography (CT) imaging. In some cases, endoscopic retrograde cholangiopancreatography (ERCP) is performed, revealing the diagnosis of pancreas divisum. If no symptoms or complications are present, then treatment is not necessary. However, if there is recurrent pancreatitis, then a sphincterotomy of the minor papilla may be indicated.

Ascending cholangitis, also known as acute cholangitis or simply cholangitis, is inflammation of the bile duct, usually caused by bacteria ascending from its junction with the duodenum. It tends to occur if the bile duct is already partially obstructed by gallstones.

Hemosuccus pancreaticus is a rare cause of hemorrhage in the gastrointestinal tract. It is caused by a bleeding source in the pancreas, pancreatic duct, or structures adjacent to the pancreas, such as the splenic artery, that bleed into the pancreatic duct, which is connected with the bowel at the duodenum, the first part of the small intestine. Patients with hemosuccus may develop symptoms of gastrointestinal hemorrhage, such as blood in the stools, maroon stools, or melena, which is a dark, tarry stool caused by digestion of red blood cells. They may also develop abdominal pain. It is associated with pancreatitis, pancreatic cancer and aneurysms of the splenic artery. Hemosuccus may be identified with endoscopy (esophagogastroduodenoscopy), where fresh blood may be seen from the pancreatic duct. Alternatively, angiography may be used to inject the celiac axis to determine the blood vessel that is bleeding. This may also be used to treat hemosuccus, as embolization of the end vessel may terminate the hemorrhage. However, a distal pancreatectomy—surgery to remove of the tail of the pancreas—may be required to stop the hemorrhage.
Biliary colic, also known as symptomatic cholelithiasis, a gallbladder attack or gallstone attack, is when a colic occurs due to a gallstone temporarily blocking the cystic duct. Typically, the pain is in the right upper part of the abdomen, and can be severe. Pain usually lasts from 15 minutes to a few hours. Often, it occurs after eating a heavy meal, or during the night. Repeated attacks are common.

Sphincter of Oddi dysfunction refers to a group of functional disorders leading to abdominal pain due to dysfunction of the Sphincter of Oddi: functional biliary sphincter of Oddi and functional pancreatic sphincter of Oddi disorder. The sphincter of Oddi is a sphincter muscle, a circular band of muscle at the bottom of the biliary tree which controls the flow of pancreatic juices and bile into the second part of the duodenum. The pathogenesis of this condition is recognized to encompass stenosis or dyskinesia of the sphincter of Oddi ; consequently the terms biliary dyskinesia, papillary stenosis, and postcholecystectomy syndrome have all been used to describe this condition. Both stenosis and dyskinesia can obstruct flow through the sphincter of Oddi and can therefore cause retention of bile in the biliary tree and pancreatic juice in the pancreatic duct.
Pancreatic abscess is a late complication of acute necrotizing pancreatitis, occurring more than 4 weeks after the initial attack. A pancreatic abscess is a collection of pus resulting from tissue necrosis, liquefaction, and infection. It is estimated that approximately 3% of the patients with acute pancreatitis will develop an abscess.
A pancreatic injury is some form of trauma sustained by the pancreas. The injury can be sustained through either blunt forces, such as a motor vehicle accident, or penetrative forces, such as that of a gunshot wound. The pancreas is one of the least commonly injured organs in abdominal trauma.

Biloma occurs when there is excess bile in the abdominal cavity. It happens when there is a bile leak. There is an increased chance of a person developing biloma after having a gallbladder removal surgery, known as Laparoscopic cholecystectomy. This procedure can be complicated by biloma with incidence of 0.3–2%. Other causes are liver biopsy, abdominal trauma, and, rarely, spontaneous perforation. The formation of Biloma does not occur frequently. Biliary fistulas are also caused by injury to the bile duct and can result in the formation of bile leaks. Biliary fistulas are abnormal communications between organs and the biliary tract. Once diagnosed, they usually require drainage. The term "biloma" was first coined in 1979 by Gould and Patel. They first discover it after they reported a case with extrahepatic bile leakage. The cause of this is trauma to the upper right quadrant of the abdomen. Originally, Biloma was described as an "encapsulated collection" of extrahepatic bile. Biloma is now described as extrabiliary collections of bile that can be either intrahepatic or extrahepatic. The most common cause to Biloma is trauma to the liver. There are other causes such as abdominal surgery, endoscopic surgery and percutaneous catheter drainage. Injury and abdominal trauma can cause damage to the biliary tree. The biliary tree is a system of vessels that direct secreations from the liver, gallbladder, and pancreas through a series of ducts into the duodenum. This can result in a bile leak which is a common cause of the formation of Biloma. It is possible for Biloma to be associated with mortality, though it is not common. Bile leaks occur in about one percent of causes.

Choledochoduodenostomy (CDD) is a surgical procedure to create an anastomosis, a surgical connection, between the common bile duct (CBD) and an alternative portion of the duodenum. In healthy individuals, the CBD meets the pancreatic duct at the ampulla of Vater, which drains via the major duodenal papilla to the second part of duodenum. In cases of benign conditions such as narrowing of the distal CBD or recurrent CBD stones, performing a CDD provides the diseased patient with CBD drainage and decompression. A side-to-side anastomosis is usually performed.
References
- ↑ "Cystogastrostomy". Right Diagnosis. Health Grades Inc. Retrieved 2 October 2014.
- ↑ Ehrlich EW, Gonzales-Lavin L (December 1966). "Pseudocysts treated by cystogastrostomy. Assessment by catheter contrast visualization". Archives of Surgery. 93 (6): 996–1001. doi:10.1001/archsurg.1966.01330060140020. PMID 5954338.
- ↑ Habashi S, Draganov PV (January 2009). "Pancreatic pseudocyst". World Journal of Gastroenterology. 15 (1): 38–47. doi:10.3748/wjg.15.38. PMC 2653285 . PMID 19115466. Archived from the original on 12 October 2014.
- 1 2 3 Varadarajulu S, Bang JY, Sutton BS, Trevino JM, Christein JD, Wilcox CM (September 2013). "Equal efficacy of endoscopic and surgical cystogastrostomy for pancreatic pseudocyst drainage in a randomized trial". Gastroenterology. 145 (3): 583–90.e1. doi:10.1053/j.gastro.2013.05.046. PMID 23732774.
- ↑ "Pancreatic pseudocyst". Medline Plus. U.S. National Library of Medicine. Retrieved 22 October 2014.
- 1 2 Giovannini M (January 2005). "Endoscopic ultrasound-guided pancreatic pseudocyst drainage". Gastrointestinal Endoscopy Clinics of North America. 15 (1): 179–88, xi. doi:10.1016/j.giec.2004.07.007. PMID 15555960.
- ↑ "Acute pancreatitis: therapy". Johns Hopkins. Retrieved 22 October 2014.
- ↑ Lutfi R, Jyot B, Rossi M, Jefferson E, Salti G (November 2010). "Hand-sewn cystogastrostomy using the novel single-incision laparoscopy with flexible-tip laparoscope". Journal of Laparoendoscopic & Advanced Surgical Techniques. Part A. 20 (9): 761–766. doi:10.1089/lap.2009.0421. PMID 20874414.
- ↑ Elechi EN, Callender CO, Calhoun T, Kurtz LH (November 1980). "Pancreatic abscess: a major complication of cystogastrostomy". Journal of the National Medical Association. 72 (11): 1067–1074. PMC 2552595 . PMID 7441786.
- ↑ Karavias T, Dollinger P, Häring R (1993). "Cystogastrostomy in the treatment of pancreatic pseudocysts". In Beger HG, Büchler M, Malfertheiner P (eds.). Standards in Pancreatic Surgery. Berlin, Heidelberg: Springer. pp. 540–543. ISBN 978-3-642-77437-9.