Related Research Articles

A psychiatric hospital, also known as a mental health hospital, or a behavioral health hospital, is a specialized medical facility that focuses on the treatment of severe mental disorders. These institutions cater to patients with conditions such as schizophrenia, bipolar disorder, major depressive disorder, and eating disorders, among others.
Anti-psychiatry, sometimes spelled antipsychiatry, is a movement based on the view that psychiatric treatment can be often more damaging than helpful to patients. The term anti-psychiatry was coined in 1912, and the movement emerged in the 1960s, highlighting controversies about psychiatry. Objections include the reliability of psychiatric diagnosis, the questionable effectiveness and harm associated with psychiatric medications, the failure of psychiatry to demonstrate any disease treatment mechanism for psychiatric medication effects, and legal concerns about equal human rights and civil freedom being nullified by the presence of diagnosis. Historical critiques of psychiatry came to light after focus on the extreme harms associated with electroconvulsive therapy and insulin shock therapy. The term "anti-psychiatry" is in dispute and often used to dismiss all critics of psychiatry, many of whom agree that a specialized role of helper for people in emotional distress may at times be appropriate, and allow for individual choice around treatment decisions.
William Walters Sargant was a British psychiatrist who is remembered for the evangelical zeal with which he promoted treatments such as psychosurgery, deep sleep treatment, electroconvulsive therapy and insulin shock therapy.

The Maudsley Hospital is a British psychiatric hospital in south London. The Maudsley is the largest mental health training institution in the UK. It is part of South London and Maudsley NHS Foundation Trust, and works in partnership with the Institute of Psychiatry, King's College London. The hospital was one of the originating institutions in producing the Maudsley Prescribing Guidelines. It is part of the King's Health Partners academic health science centre and the National Institute for Health and Care Research (NIHR) Biomedical Research Centre for Mental Health.

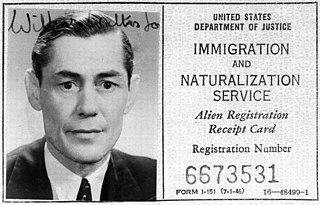
Insulin shock therapy or insulin coma therapy was a form of psychiatric treatment in which patients were repeatedly injected with large doses of insulin in order to produce daily comas over several weeks. It was introduced in 1927 by Austrian-American psychiatrist Manfred Sakel and used extensively in the 1940s and 1950s, mainly for schizophrenia, before falling out of favour and being replaced by neuroleptic drugs in the 1960s.

Fulbourn Hospital is a mental health facility located between the Cambridgeshire village of Fulbourn and the Cambridge city boundary at Cherry Hinton, about 5 miles (8 km) south-east of the city centre. It is managed by the Cambridgeshire and Peterborough NHS Foundation Trust. The Ida Darwin Hospital site is situated behind Fulbourn Hospital. It is run and managed by the same trust, with both hospitals sharing the same facilities and staff pool.

Claybury Hospital was a psychiatric hospital in Woodford Bridge, London. It was built to a design by the English architect George Thomas Hine who was a prolific Victorian architect of hospital buildings. It was opened in 1893 making it the Fifth Middlesex County Asylum. Historic England identified the hospital as being "the most important asylum built in England after 1875".

Powick Hospital, which opened in 1847 was a psychiatric facility located on 552 acres (223 ha) outside the village of Powick, near Malvern, Worcestershire. At its peak, the hospital housed around 1,000 patients in buildings designed for 400. During the 1950s the hospital gained an internationally acclaimed reputation for its use of the drug LSD in psychotherapy pioneered and conducted by Ronald A. Sandison. In 1968 the institution was surrounded by controversy concerning serious neglect of patients. In 1989 it was closed down leaving Barnsley Hall Hospital in Bromsgrove as the remaining psychiatric hospital in the county. Most of the complex has been demolished to make way for a housing estate.

The Austen Riggs Center is a psychiatric treatment facility located in Stockbridge, Massachusetts. It was founded in 1913 as the Stockbridge Institute for the Study and Treatment of Psychoneuroses by Austen Fox Riggs. The institution was renamed in his honor on July 21, 1919.

Asylum architecture in the United States, including the architecture of psychiatric hospitals, affected the changing methods of treating the mentally ill in the nineteenth century: the architecture was considered part of the cure. Doctors believed that ninety percent of insanity cases were curable, but only if treated outside the home, in large-scale buildings. Nineteenth-century psychiatrists considered the architecture of asylums, especially their planning, to be one of the most powerful tools for the treatment of the insane, targeting social as well as biological factors to facilitate the treatment of mental illnesses. The construction and usage of these quasi-public buildings served to legitimize developing ideas in psychiatry. About 300 psychiatric hospitals, known at the time as insane asylums or colloquially as “loony bins” or “nuthouses,” were constructed in the United States before 1900. Asylum architecture is notable for the way similar floor plans were built in a wide range of architectural styles.

Psychiatry is the medical specialty devoted to the diagnosis, prevention, and treatment of deleterious mental conditions. These include various matters related to mood, behaviour, cognition, perceptions, and emotions.
Christine Dean FRCPsych is an English psychiatrist consulting at the Priory Hospital, Roehampton, the British Association of Performing Arts Medicine (BAPAM), The Helen Bamber Foundation, in her private practice and as a medical member of the Mental Health Review Tribunals, Ministry of Justice.
This is a timeline of the modern development of psychiatry. Related information can be found in the Timeline of psychology and Timeline of psychotherapy articles.
Ted Chabasinski is an American psychiatric survivor, human rights activist and attorney who lives in Berkeley, California. At the age of six, he was taken from his foster family's home and committed to a New York psychiatric facility. Diagnosed with childhood schizophrenia, he underwent intensive electroshock therapy and remained an inmate in a state psychiatric hospital until the age of seventeen. He subsequently trained as a lawyer and became active in the psychiatric survivors movement. In 1982, he was a leader in an initially successful campaign seeking to ban the use of electroshock in Berkeley, California.

The lunatic asylum, insane asylum or mental asylum was an institution where people with mental illness were confined. It was an early precursor of the modern psychiatric hospital.
Winfred Overholser was an American psychiatrist, president of the American Psychiatric Association, and for 25 years the superintendent of St. Elizabeths Hospital, a federal institution for the mentally ill in Washington, D.C.

David Kennedy Henderson FRSE FRCPE was a Scottish physician and psychiatrist and served as president of the Royal College of Physicians of Edinburgh 1949 to 1951.

David John Impastato was an American neuropsychiatrist who pioneered the use of electroconvulsive therapy (ECT) in the United States. A treatment for mental illness initially called "electroshock," ECT was developed in 1937 by Dr. Ugo Cerletti and Lucio Bini, working in Rome. Impastato has been credited with the earliest documented use of the revolutionary method in North America, administered in early 1940 to a schizophrenic female patient in New York City. Soon after, he and colleague Dr. Renato Almansi completed the first case study of ECT to appear in a U.S. publication. Impastato spent the next four decades refining the technique, gaining recognition as one of its most authoritative spokesmen. He taught, lectured widely and published over fifty articles on his work. He called on ECT practitioners to observe the strictest protocols of patient safety, countered resistance to ECT from both the medical and cultural establishments, and met later challenges to electroconvulsive therapy from developments in psychopharmacology. Impastato would live to see ECT recommended by the American Psychiatric Association for a distinct core of intractable mental disorders. The U.S. Food and Drug Administration took longer to respond to the treatment's potential. But in 2016 the FDA drafted guidelines for ECT similar to those of the APA, as well as proposing regulations for treatment with Class II and Class III devices. Though still not free of controversy, electroconvulsive therapy is the treatment of choice for an estimated 100,000 patients a year in the United States.

Eileen Skellern FRCN (1923–1980) was an English psychiatric nurse who was involved in pioneering psychosocial and psychotherapeutic methods for treating patients. She helped open up new roles for nurses in mental health work, and demonstrated that they could be equal partners in a team, taking personal responsibility for patient care while collaborating with doctors and playing an important part in new developments in therapeutic treatment. While also taking a lead in education, administration and policy development, she did research and published in medical and nursing journals, and was a member of key committees in her field.
Ronald Arthur Sandison was a British psychiatrist and psychotherapist. Among his other work. he is particularly noted for his pioneering studies and use of lysergic acid diethylamide (LSD) as a psychotheraputic drug. As a consultant psychiatrist, his LSD work was mainly carried out during the 1950s and '60s at Powick Hospital, a large psychiatric facility near Malvern, Worcestershire, after which he spent several years in Southampton, where he was instrumental in the establishment of the university medical school. He returned to his native Shetland Isles in the 1970s and worked in psychotherapy there. He later specialised in psychosexual medicine on the UK mainland. Sandison died at the age of 94, and was buried in Ledbury near Malvern.
References
- 1 2 Kennard 2010.
- ↑ D.H, Clark (1967). "Psychiatric halfway house". hdl:1842/17103.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Havergal, Chris (2 April 2010). "Tributes to man who made hospital human". Cambridge News. 2010. Archived from the original on 17 July 2013. Retrieved 17 July 2013.
- ↑ Dopson, Laurence (19 July 2010). "Doctor David Clark: Pioneer of the social model in psychiatry".
- Kennard, David (11 May 2010). "Psychiatrist who breathed new life into mental health care". The Guardian. Retrieved 17 July 2013.