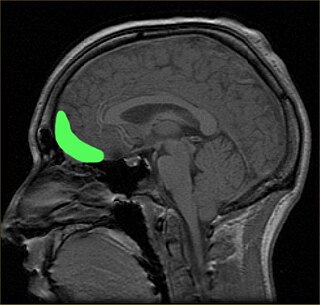
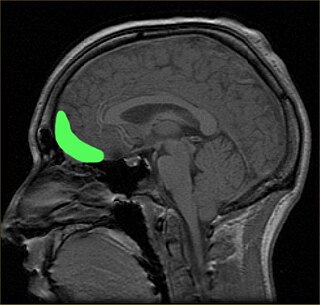
Bilateral cingulotomy is a form of psychosurgery, introduced in 1948 as an alternative to lobotomy. Today, it is mainly used in the treatment of depression and obsessive-compulsive disorder. In the early years of the twenty-first century, it was used in Russia to treat addiction. It is also used in the treatment of chronic pain. The objective of this procedure is the severing of the supracallosal fibres of the cingulum bundle, which pass through the anterior cingulate gyrus.

Tourette syndrome or Tourette's syndrome is a common neurodevelopmental disorder that begins in childhood or adolescence. It is characterized by multiple movement (motor) tics and at least one vocal (phonic) tic. Common tics are blinking, coughing, throat clearing, sniffing, and facial movements. These are typically preceded by an unwanted urge or sensation in the affected muscles known as a premonitory urge, can sometimes be suppressed temporarily, and characteristically change in location, strength, and frequency. Tourette's is at the more severe end of a spectrum of tic disorders. The tics often go unnoticed by casual observers.

Trichotillomania (TTM), also known as hair-pulling disorder or compulsive hair pulling, is a mental disorder characterized by a long-term urge that results in the pulling out of one's own hair. A brief positive feeling may occur as hair is removed. Efforts to stop pulling hair typically fail. Hair removal may occur anywhere; however, the head and around the eyes are most common. The hair pulling is to such a degree that it results in distress and hair loss can be seen.

Obsessive–compulsive personality disorder (OCPD) is a cluster C personality disorder marked by a spectrum of obsessions with rules, lists, schedules, and order, among other things. Symptoms are usually present by the time a person reaches adulthood, and are visible in a variety of situations. The cause of OCPD is thought to involve a combination of genetic and environmental factors, namely problems with attachment.

In the human brain, the anterior cingulate cortex (ACC) is the frontal part of the cingulate cortex that resembles a "collar" surrounding the frontal part of the corpus callosum. It consists of Brodmann areas 24, 32, and 33.

The caudate nucleus is one of the structures that make up the corpus striatum, which is a component of the basal ganglia in the human brain. While the caudate nucleus has long been associated with motor processes due to its role in Parkinson's disease, it plays important roles in various other nonmotor functions as well, including procedural learning, associative learning and inhibitory control of action, among other functions. The caudate is also one of the brain structures which compose the reward system and functions as part of the cortico–basal ganglia–thalamic loop.
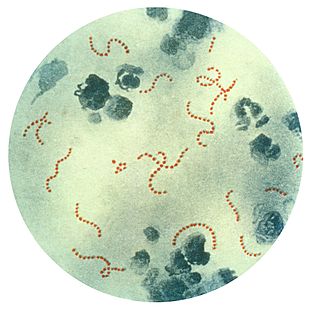
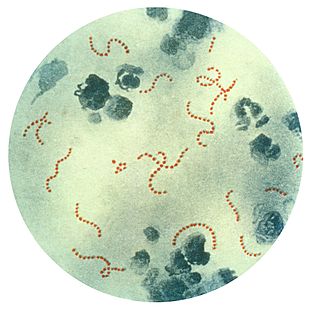
Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS) is a controversial hypothetical diagnosis for a subset of children with rapid onset of obsessive-compulsive disorder (OCD) or tic disorders. Symptoms are proposed to be caused by group A streptococcal (GAS), and more specifically, group A beta-hemolytic streptococcal (GABHS) infections. OCD and tic disorders are hypothesized to arise in a subset of children as a result of a post-streptococcal autoimmune process. The proposed link between infection and these disorders is that an autoimmune reaction to infection produces antibodies that interfere with basal ganglia function, causing symptom exacerbations, and this autoimmune response results in a broad range of neuropsychiatric symptoms.
The orbitofrontal cortex (OFC) is a prefrontal cortex region in the frontal lobes of the brain which is involved in the cognitive process of decision-making. In non-human primates it consists of the association cortex areas Brodmann area 11, 12 and 13; in humans it consists of Brodmann area 10, 11 and 47.

An intrusive thought is an unwelcome, involuntary thought, image, or unpleasant idea that may become an obsession, is upsetting or distressing, and can feel difficult to manage or eliminate. When such thoughts are associated with obsessive-compulsive disorder (OCD), Tourette's syndrome (TS), depression, body dysmorphic disorder (BDD), and sometimes attention-deficit hyperactivity disorder (ADHD), the thoughts may become paralyzing, anxiety-provoking, or persistent. Intrusive thoughts may also be associated with episodic memory, unwanted worries or memories from OCD, post-traumatic stress disorder, other anxiety disorders, eating disorders, or psychosis. Intrusive thoughts, urges, and images are of inappropriate things at inappropriate times, and generally have aggressive, sexual, or blasphemous themes.
The obsessive–compulsive spectrum is a model of medical classification where various psychiatric, neurological and/or medical conditions are described as existing on a spectrum of conditions related to obsessive–compulsive disorder (OCD). "The disorders are thought to lie on a spectrum from impulsive to compulsive where impulsivity is said to persist due to deficits in the ability to inhibit repetitive behavior with known negative consequences, while compulsivity persists as a consequence of deficits in recognizing completion of tasks." OCD is a mental disorder characterized by obsessions and/or compulsions. An obsession is defined as "a recurring thought, image, or urge that the individual cannot control". Compulsion can be described as a "ritualistic behavior that the person feels compelled to perform". The model suggests that many conditions overlap with OCD in symptomatic profile, demographics, family history, neurobiology, comorbidity, clinical course and response to various pharmacotherapies. Conditions described as being on the spectrum are sometimes referred to as obsessive–compulsive spectrum disorders.
Exposure therapy is a technique in behavior therapy to treat anxiety disorders.
Primarily obsessional obsessive–compulsive disorder, also known as purely obsessional obsessive–compulsive disorder, is a lesser-known form or manifestation of OCD. It is not a diagnosis in the DSM-5. For people with primarily obsessional OCD, there are fewer observable compulsions, compared to those commonly seen with the typical form of OCD. While ritualizing and neutralizing behaviors do take place, they are mostly cognitive in nature, involving mental avoidance and excessive rumination. Primarily obsessional OCD takes the form of intrusive thoughts often of a distressing, sexual, or violent nature.

Obsessive–compulsive disorder (OCD) is a mental and behavioral disorder in which an individual has intrusive thoughts and feels the need to perform certain routines (compulsions) repeatedly to relieve the distress caused by the obsession, to the extent where it impairs general function.
Susan Swedo is a researcher in the field of pediatrics and neuropsychiatry. Beginning in 1998, she was Chief of the Pediatrics & Developmental Neuroscience Branch at the US National Institute of Mental Health. In 1994, Swedo was lead author on a paper describing pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS), a controversial hypothesis proposing a link between Group A streptococcal infection in children and some rapid-onset cases of obsessive-compulsive disorder (OCD) or tic disorders such as Tourette syndrome. Swedo retired from the NIH in 2019, and serves on the PANDAS Physician Network.
The biology of obsessive–compulsive disorder (OCD) refers biologically based theories about the mechanism of OCD. Cognitive models generally fall into the category of executive dysfunction or modulatory control. Neuroanatomically, functional and structural neuroimaging studies implicate the prefrontal cortex (PFC), basal ganglia (BG), insula, and posterior cingulate cortex (PCC). Genetic and neurochemical studies implicate glutamate and monoamine neurotransmitters, especially serotonin and dopamine.
The cause of obsessive–compulsive disorder is understood mainly through identifying biological risk factors that lead to obsessive–compulsive disorder (OCD) symptomology. The leading hypotheses propose the involvement of the orbitofrontal cortex, basal ganglia, and/or the limbic system, with discoveries being made in the fields of neuroanatomy, neurochemistry, neuroimmunology, neurogenetics, and neuroethology.
In psychology, relationship obsessive–compulsive disorder (ROCD) is a form of obsessive–compulsive disorder focusing on close or intimate relationships. Such obsessions can become extremely distressing and debilitating, having negative impacts on relationships functioning.

Wayne Goodman is an American psychiatrist and researcher who specializes in Obsessive-Compulsive Disorder (OCD). He is the principal developer, along with his colleagues, of the Yale-Brown Obsessive Compulsive Scale (Y-BOCS).

Jonathan Stuart Abramowitz is an American clinical psychologist and Professor in the Department of Psychology and Neuroscience at the University of North Carolina at Chapel Hill (UNC-CH). He is an expert on obsessive-compulsive disorder (OCD) and anxiety disorders whose work is highly cited. He maintains a research lab and currently serves as the Director of the UNC-CH Clinical Psychology PhD Program. Abramowitz approaches the understanding and treatment of psychological problems from a cognitive-behavioral perspective.

Carolyn I. Rodriguez is a Puerto Rican psychiatrist, neuroscientist, and clinical researcher developing treatments for obsessive compulsive disorder as well as mapping circuit dysfunction in the human brain. Rodriguez holds appointments in both clinical and academic departments at Stanford University. Rodriguez is a Clinical Lab Director at the Stanford Center for Cognitive and Neurobiological Imaging, an associate professor and Associate Chair of Psychiatry and Behavioral Sciences, and a Director of several specialized translational research programs.