Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer in adults and is currently the most common cause of death in people with cirrhosis. HCC is the third leading cause of cancer-related deaths worldwide.
Transcatheter arterial chemoembolization (TACE) is a minimally invasive procedure performed in interventional radiology to restrict a tumor's blood supply. Small embolic particles coated with chemotherapeutic drugs are injected selectively through a catheter into an artery directly supplying the tumor. These particles both block the blood supply and induce cytotoxicity, attacking the tumor in several ways.

Targeted therapy or molecularly targeted therapy is one of the major modalities of medical treatment (pharmacotherapy) for cancer, others being hormonal therapy and cytotoxic chemotherapy. As a form of molecular medicine, targeted therapy blocks the growth of cancer cells by interfering with specific targeted molecules needed for carcinogenesis and tumor growth, rather than by simply interfering with all rapidly dividing cells. Because most agents for targeted therapy are biopharmaceuticals, the term biologic therapy is sometimes synonymous with targeted therapy when used in the context of cancer therapy. However, the modalities can be combined; antibody-drug conjugates combine biologic and cytotoxic mechanisms into one targeted therapy.

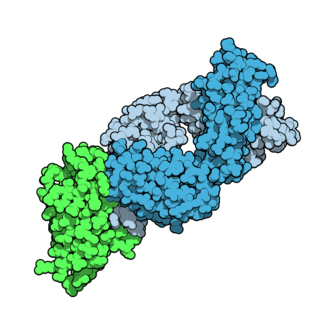
Ipilimumab, sold under the brand name Yervoy, is a monoclonal antibody medication that works to activate the immune system by targeting CTLA-4, a protein receptor that downregulates the immune system.
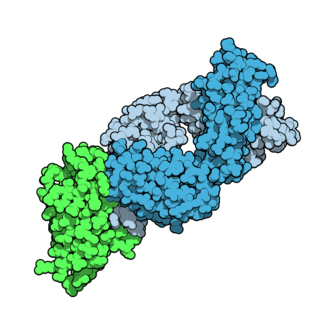
Tremelimumab, sold under the brand name Imjudo, is a fully human monoclonal antibody used for the treatment of hepatocellular carcinoma. Tremelimumab is designed to attach to and block CTLA-4, a protein that controls the activity of T cells, which are part of the immune system.
Percutaneous hepatic perfusion (PHP) is a regionalized, minimally-invasive approach to cancer treatment currently undergoing Phase II and Phase III clinical testing. PHP treats a variety of hepatic tumors by isolating the liver and exposing the organ to high-dose chemotherapy. As demonstrated in clinical trials, patients treated by PHP can tolerate much higher doses of chemotherapeutic agents than those receiving traditional systemic chemotherapy without increased toxicities.
Hepatic arterial infusion (HAI) is a medical procedure that delivers chemotherapy directly to the liver. The procedure, mostly used in combination with systemic chemotherapy, plays a role in the treatment of liver metastases in patients with colorectal cancer (CRC). Although surgical resection remains the standard of care for these liver metastases, majority of patients have lesions that are unresectable.

Selective internal radiation therapy (SIRT), also known as transarterial radioembolization (TARE), radioembolization or intra-arterial microbrachytherapy is a form of radiation therapy used in interventional radiology to treat cancer. It is generally for selected patients with surgically unresectable cancers, especially hepatocellular carcinoma or metastasis to the liver. The treatment involves injecting tiny microspheres of radioactive material into the arteries that supply the tumor, where the spheres lodge in the small vessels of the tumor. Because this treatment combines radiotherapy with embolization, it is also called radioembolization. The chemotherapeutic analogue is called chemoembolization, of which transcatheter arterial chemoembolization (TACE) is the usual form.
Cixutumumab (IMC-A12) is a human monoclonal antibody for the treatment of solid tumors.
Ramucirumab is a fully human monoclonal antibody (IgG1) developed for the treatment of solid tumors. This drug was developed by ImClone Systems Inc. It was isolated from a native phage display library from Dyax.
Glembatumumab vedotin is an antibody-drug conjugate (ADC) that targets cancer cells expressing transmembrane glycoprotein NMB (GPNMB).

Vemurafenib (INN), sold under the brand name Zelboraf, is a medication used for the treatment of late-stage melanoma. It is an inhibitor of the B-Raf enzyme and was developed by Plexxikon.

Wolfram Samlowski is an American medical oncologist with Comprehensive Cancer Centers of Nevada (CCCN) and a member of the Research Developmental Therapeutics and Genitourinary Committees for US Oncology. His research interests include translational research and development of novel cancer immunotherapy agents, translational drug development as well as gene therapy. His clinical interests are in developing more effective treatments for advanced stages of melanoma and non-melanoma skin cancers, and renal cancer.
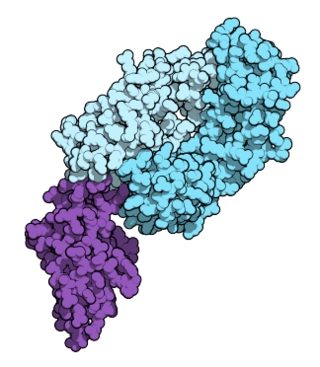
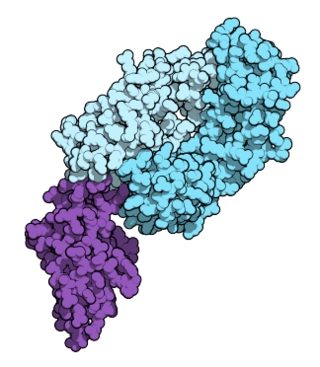
Nivolumab, sold under the brand name Opdivo, is a medication used to treat a number of types of cancer. This includes melanoma, lung cancer, malignant pleural mesothelioma, renal cell carcinoma, Hodgkin lymphoma, head and neck cancer, urothelial carcinoma, colon cancer, esophageal squamous cell carcinoma, liver cancer, gastric cancer, and esophageal or gastroesophageal junction (GEJ) cancer. It is used by slow injection into a vein.

Pembrolizumab, sold under the brand name Keytruda, is a humanized antibody used in cancer immunotherapy that treats melanoma, lung cancer, head and neck cancer, Hodgkin lymphoma, stomach cancer, cervical cancer, and certain types of breast cancer. It is given by slow injection into a vein.
Hepatic artery embolization, also known as trans-arterial embolization (TAE), is one of the several therapeutic methods to treat primary liver tumors or metastases to the liver. The embolization therapy can reduce the size of the tumor, and decrease the tumor's impact such its hormone production, effectively decreasing symptoms. The treatment was initially developed in the early 1970s. The several types of hepatic artery treatments are based on the observation that tumor cells get nearly all their nutrients from the hepatic artery, while the normal cells of the liver get about 70-80 percent of their nutrients and 50% their oxygen supply from the portal vein, and thus can survive with the hepatic artery effectively blocked. In practice, hepatic artery embolization occludes the blood flow to the tumors, achieving significant tumor shrinkage in over 80% of people. Shrinkage rates vary.

Binimetinib, also known as Mektovi and ARRY-162, is an anti-cancer small molecule that was developed by Array Biopharma to treat various cancers. Binimetinib is a selective inhibitor of MEK, a central kinase in the tumor-promoting MAPK pathway. Inappropriate activation of the pathway has been shown to occur in many cancers. In June 2018 it was approved by the FDA in combination with encorafenib for the treatment of patients with unresectable or metastatic BRAF V600E or V600K mutation-positive melanoma.
Interventional oncology is a subspecialty field of interventional radiology that deals with the diagnosis and treatment of cancer and cancer-related problems using targeted minimally invasive procedures performed under image guidance. Interventional oncology has developed to a separate pillar of modern oncology and it employs X-ray, ultrasound, computed tomography (CT) or magnetic resonance imaging (MRI) to help guide miniaturized instruments to allow targeted and precise treatment of solid tumours located in various organs of the human body, including but not limited to the liver, kidneys, lungs, and bones. Interventional oncology treatments are routinely carried out by interventional radiologists in appropriate settings and facilities.
The immune-related response criteria (irRC) is a set of published rules that define when tumors in cancer patients improve ("respond"), stay the same ("stabilize"), or worsen ("progress") during treatment, where the compound being evaluated is an immuno-oncology drug. Immuno-oncology, part of the broader field of cancer immunotherapy, involves agents which harness the body's own immune system to fight cancer. Traditionally, patient responses to new cancer treatments have been evaluated using two sets of criteria, the WHO criteria and the response evaluation criteria in solid tumors (RECIST). The immune-related response criteria, first published in 2009, arose out of observations that immuno-oncology drugs would fail in clinical trials that measured responses using the WHO or RECIST Criteria, because these criteria could not account for the time gap in many patients between initial treatment and the apparent action of the immune system to reduce the tumor burden.
Transarterial bland embolization is a catheter-based tumor treatment of the liver. In this procedure, a variety of embolizing agents can be delivered through the tumor’s feeding artery in order to completely occlude the tumor’s blood supply. The anti-tumor effects are solely based on tumor ischemia and infarction of tumor tissue, as no chemotherapeutic agents are administered. The rationale for the use of bland embolization for hepatocellular carcinoma(HCC) and/or other hyper-vascular tumors is based on the fact that normal liver receives a dual blood supply from the hepatic artery (25%) and the portal vein (75%). As the tumor grows, it becomes increasingly dependent on the hepatic artery for blood supply. Once a tumor nodule reaches a diameter of 2 cm or more, most of the blood supply is derived from the hepatic artery. Therefore, bland embolization and transarterial chemoembolization (TACE) consist of the selective angiographic occlusion of the tumor arterial blood supply with a variety of embolizing agents, with or without the precedence of local chemotherapy infusion. The occlusion by embolic particles results in tumor hypoxia and necrosis, without affecting the normal hepatic parenchyma.