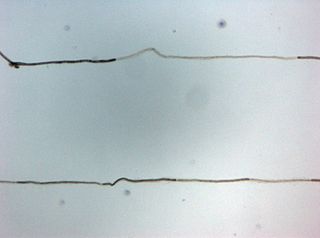
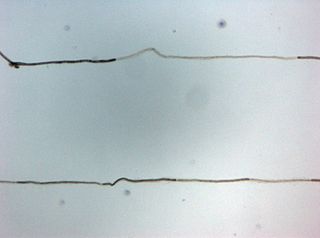
In neuroscience, an F wave is one of several motor responses which may follow the direct motor response (M) evoked by electrical stimulation of peripheral motor or mixed nerves. F-waves are the second of two late voltage changes observed after stimulation is applied to the skin surface above the distal region of a nerve, in addition to the H-reflex which is a muscle reaction in response to electrical stimulation of innervating sensory fibers. Traversal of F-waves along the entire length of peripheral nerves between the spinal cord and muscle, allows for assessment of motor nerve conduction between distal stimulation sites in the arm and leg, and related motoneurons (MN's) in the cervical and lumbosacral cord. F-waves are able to assess both afferent and efferent loops of the alpha motor neuron in its entirety. As such, various properties of F-wave motor nerve conduction are analyzed in nerve conduction studies (NCS), and often used to assess polyneuropathies, resulting from states of neuronal demyelination and loss of peripheral axonal integrity.

Lambert–Eaton myasthenic syndrome (LEMS) is a rare autoimmune disorder characterized by muscle weakness of the limbs.
Diabetic neuropathy is various types of nerve damage associated with diabetes mellitus. Symptoms depend on the site of nerve damage and can include motor changes such as weakness; sensory symptoms such as numbness, tingling, or pain; or autonomic changes such as urinary symptoms. These changes are thought to result from a microvascular injury involving small blood vessels that supply nerves. Relatively common conditions which may be associated with diabetic neuropathy include distal symmetric polyneuropathy; third, fourth, or sixth cranial nerve palsy; mononeuropathy; mononeuropathy multiplex; diabetic amyotrophy; and autonomic neuropathy.

Polyneuropathy is damage or disease affecting peripheral nerves in roughly the same areas on both sides of the body, featuring weakness, numbness, and burning pain. It usually begins in the hands and feet and may progress to the arms and legs and sometimes to other parts of the body where it may affect the autonomic nervous system. It may be acute or chronic. A number of different disorders may cause polyneuropathy, including diabetes and some types of Guillain–Barré syndrome.

Electromyography (EMG) is a technique for evaluating and recording the electrical activity produced by skeletal muscles. EMG is performed using an instrument called an electromyograph to produce a record called an electromyogram. An electromyograph detects the electric potential generated by muscle cells when these cells are electrically or neurologically activated. The signals can be analyzed to detect abnormalities, activation level, or recruitment order, or to analyze the biomechanics of human or animal movement. Needle EMG is an electrodiagnostic medicine technique commonly used by neurologists. Surface EMG is a non-medical procedure used to assess muscle activation by several professionals, including physiotherapists, kinesiologists and biomedical engineers. In computer science, EMG is also used as middleware in gesture recognition towards allowing the input of physical action to a computer as a form of human-computer interaction.

Alcoholic polyneuropathy is a neurological disorder in which peripheral nerves throughout the body malfunction simultaneously. It is defined by axonal degeneration in neurons of both the sensory and motor systems and initially occurs at the distal ends of the longest axons in the body. This nerve damage causes an individual to experience pain and motor weakness, first in the feet and hands and then progressing centrally. Alcoholic polyneuropathy is caused primarily by chronic alcoholism; however, vitamin deficiencies are also known to contribute to its development. This disease typically occurs in chronic alcoholics who have some sort of nutritional deficiency. Treatment may involve nutritional supplementation, pain management, and abstaining from alcohol.

A nerve conduction study (NCS) is a medical diagnostic test commonly used to evaluate the function, especially the ability of electrical conduction, of the motor and sensory nerves of the human body. These tests may be performed by medical specialists such as clinical neurophysiologists, physical therapists, physiatrists, and neurologists who subspecialize in electrodiagnostic medicine. In the United States, neurologists and physiatrists receive training in electrodiagnostic medicine as part of residency training and in some cases acquire additional expertise during a fellowship in clinical neurophysiology, electrodiagnostic medicine, or neuromuscular medicine. Outside the US, clinical neurophysiologists learn needle EMG and NCS testing.

In neuroscience, nerve conduction velocity (CV) is the speed at which an electrochemical impulse propagates down a neural pathway. Conduction velocities are affected by a wide array of factors, which include age, sex, and various medical conditions. Studies allow for better diagnoses of various neuropathies, especially demyelinating diseases as these conditions result in reduced or non-existent conduction velocities. CV is an important aspect of nerve conduction studies.
Proximal diabetic neuropathy, also known as diabetic amyotrophy, is a complication of diabetes mellitus that affects the nerves that supply the thighs, hips, buttocks and/or lower legs. Proximal diabetic neuropathy is a type of diabetic neuropathy characterized by muscle wasting, weakness, pain, or changes in sensation/numbness of the leg. It is caused by damage to the nerves of the lumbosacral plexus.
Chronic inflammatory demyelinating polyneuropathy (CIDP) is an acquired autoimmune disease of the peripheral nervous system characterized by progressive weakness and impaired sensory function in the legs and arms. The disorder is sometimes called chronic relapsing polyneuropathy (CRP) or chronic inflammatory demyelinating polyradiculoneuropathy. CIDP is closely related to Guillain–Barré syndrome and it is considered the chronic counterpart of that acute disease. Its symptoms are also similar to progressive inflammatory neuropathy. It is one of several types of neuropathy.

Centronuclear myopathies (CNM) are a group of congenital myopathies where cell nuclei are abnormally located in the center of muscle cells instead of their normal location at the periphery.

Rheobase is a measure of membrane potential excitability. In neuroscience, rheobase is the minimal current amplitude of infinite duration that results in the depolarization threshold of the cell membranes being reached, such as an action potential or the contraction of a muscle. In Greek, the root rhe translates to "current or flow", and basi means "bottom or foundation": thus the rheobase is the minimum current that will produce an action potential or muscle contraction.

Radiculopathy, also commonly referred to as pinched nerve, refers to a set of conditions in which one or more nerves are affected and do not work properly. Radiculopathy can result in pain, weakness, altered sensation (paresthesia) or difficulty controlling specific muscles. Pinched nerves arise when surrounding bone or tissue, such as cartilage, muscles or tendons, put pressure on the nerve and disrupt its function.
Sudomotor function refers to the autonomic nervous system control of sweat gland activity in response to various environmental and individual factors. Sweat production is a vital thermoregulatory mechanism used by the body to prevent heat-related illness as the evaporation of sweat is the body’s most effective method of heat reduction and the only cooling method available when the air temperature rises above skin temperature. In addition, sweat plays key roles in grip, microbial defense, and wound healing.
Critical illness polyneuropathy (CIP) and critical illness myopathy (CIM) are overlapping syndromes of diffuse, symmetric, flaccid muscle weakness occurring in critically ill patients and involving all extremities and the diaphragm with relative sparing of the cranial nerves. CIP and CIM have similar symptoms and presentations and are often distinguished largely on the basis of specialized electrophysiologic testing or muscle and nerve biopsy. The causes of CIP and CIM are unknown, though they are thought to be a possible neurological manifestation of systemic inflammatory response syndrome. Corticosteroids and neuromuscular blocking agents, which are widely used in intensive care, may contribute to the development of CIP and CIM, as may elevations in blood sugar, which frequently occur in critically ill patients.

Hereditary motor and sensory neuropathies (HMSN) is a name sometimes given to a group of different neuropathies which are all characterized by their impact upon both afferent and efferent neural communication. HMSN are characterised by atypical neural development and degradation of neural tissue. The two common forms of HMSN are either hypertrophic demyelinated nerves or complete atrophy of neural tissue. Hypertrophic condition causes neural stiffness and a demyelination of nerves in the peripheral nervous system, and atrophy causes the breakdown of axons and neural cell bodies. In these disorders, a patient experiences progressive muscle atrophy and sensory neuropathy of the extremities.
Repetitive nerve stimulation is a variant of the nerve conduction study where electrical stimulation is delivered to a motor nerve repeatedly several times per second. By observing the change in the muscle electrical response (CMAP) after several stimulations, a physician can assess for the presence of a neuromuscular junction disease, and differentiate between presynaptic and postsynaptic conditions. The test was first described by German neurologist Friedrich Jolly in 1895, and is also known as Jolly's test.
Clinical Electrophysiological Testing is based on techniques derived from electrophysiology used for the clinical diagnosis of patients. There are many processes that occur in the body which produce electrical signals that can be detected. Depending on the location and the source of these signals, distinct methods and techniques have been developed to properly target them.
Electrodiagnosis (EDX) is a method of medical diagnosis that obtains information about diseases by passively recording the electrical activity of body parts or by measuring their response to external electrical stimuli. The most widely used methods of recording spontaneous electrical activity are various forms of electrodiagnostic testing (electrography) such as electrocardiography (ECG), electroencephalography (EEG), and electromyography (EMG). Electrodiagnostic medicine is a medical subspecialty of neurology, clinical neurophysiology, cardiology, and physical medicine and rehabilitation. Electrodiagnostic physicians apply electrophysiologic techniques, including needle electromyography and nerve conduction studies to diagnose, evaluate, and treat people with impairments of the neurologic, neuromuscular, and/or muscular systems. The provision of a quality electrodiagnostic medical evaluation requires extensive scientific knowledge that includes anatomy and physiology of the peripheral nerves and muscles, the physics and biology of the electrical signals generated by muscle and nerve, the instrumentation used to process these signals, and techniques for clinical evaluation of diseases of the peripheral nerves and sensory pathways.
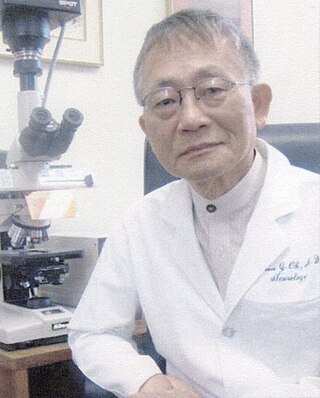
Shin Joong Oh is a Korean physician who is Distinguished Professor of Neurology Emeritus at The University of Alabama at Birmingham in the United States. Oh is a clinician, researcher, and educator known for his contributions to the fields of neurology and electrodiagnostic medicine, particularly electromyography. He retired in 2014.