A polyp is an abnormal growth of tissue projecting from a mucous membrane. If it is attached to the surface by a narrow elongated stalk, it is said to be pedunculated; if it is attached without a stalk, it is said to be sessile. Polyps are commonly found in the colon, stomach, nose, ear, sinus(es), urinary bladder, and uterus. They may also occur elsewhere in the body where there are mucous membranes, including the cervix, vocal folds, and small intestine. Some polyps are tumors (neoplasms) and others are non-neoplastic, for example hyperplastic or dysplastic, which are benign. The neoplastic ones are usually benign, although some can be pre-malignant, or concurrent with a malignancy.

Esophagogastroduodenoscopy (EGD) or oesophagogastroduodenoscopy (OGD), also called by various other names, is a diagnostic endoscopic procedure that visualizes the upper part of the gastrointestinal tract down to the duodenum. It is considered a minimally invasive procedure since it does not require an incision into one of the major body cavities and does not require any significant recovery after the procedure. However, a sore throat is common.

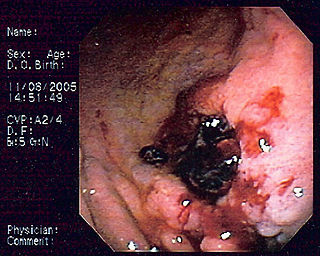
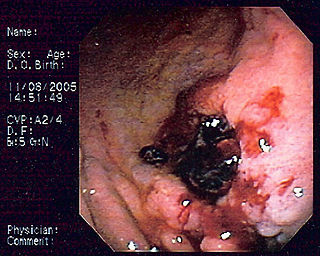
Dieulafoy's lesion is a medical condition characterized by a large tortuous artery most commonly in the stomach wall (submucosal) that erodes and bleeds. It can present in any part of the gastrointestinal tract. It can cause gastric hemorrhage but is relatively uncommon. It is thought to cause less than 5% of all gastrointestinal bleeds in adults. It was named after French surgeon Paul Georges Dieulafoy, who described this condition in his paper "Exulceratio simplex: Leçons 1-3" in 1898. It is also called "caliber-persistent artery" or "aneurysm" of gastric vessels. However, unlike most other aneurysms, these are thought to be developmental malformations rather than degenerative changes.

A hamartoma is a mostly benign, local malformation of cells that resembles a neoplasm of local tissue but is usually due to an overgrowth of multiple aberrant cells, with a basis in a systemic genetic condition, rather than a growth descended from a single mutated cell (monoclonality), as would typically define a benign neoplasm/tumor. Despite this, many hamartomas are found to have clonal chromosomal aberrations that are acquired through somatic mutations, and on this basis the term hamartoma is sometimes considered synonymous with neoplasm. Hamartomas are by definition benign, slow-growing or self-limiting, though the underlying condition may still predispose the individual towards malignancies.
Primary gastric lymphoma is an uncommon condition, accounting for less than 15% of gastric malignancies and about 2% of all lymphomas. However, the stomach is a very common extranodal site for lymphomas. It is also the most common source of lymphomas in the gastrointestinal tract.

Double-balloon enteroscopy, also known as push-and-pull enteroscopy, is an endoscopic technique for visualization of the small bowel. It was developed by Hironori Yamamoto in 2001. It is novel in the field of diagnostic gastroenterology as it is the first endoscopic technique that allows for the entire gastrointestinal tract to be visualized in real time.

A bowel resection or enterectomy is a surgical procedure in which a part of an intestine (bowel) is removed, from either the small intestine or large intestine. Often the word enterectomy is reserved for the sense of small bowel resection, in distinction from colectomy, which covers the sense of large bowel resection. Bowel resection may be performed to treat gastrointestinal cancer, bowel ischemia, necrosis, or obstruction due to scar tissue, volvulus, and hernias. Some patients require ileostomy or colostomy after this procedure as alternative means of excretion. Complications of the procedure may include anastomotic leak or dehiscence, hernias, or adhesions causing partial or complete bowel obstruction. Depending on which part and how much of the intestines are removed, there may be digestive and metabolic challenges afterward, such as short bowel syndrome.

The submucosa is a thin layer of tissue in various organs of the gastrointestinal, respiratory, and genitourinary tracts. It is the layer of dense irregular connective tissue that supports the mucosa and joins it to the muscular layer, the bulk of overlying smooth muscle.

Colonic polypectomy is the removal of colorectal polyps in order to prevent them from turning cancerous.

An endoclip is a metallic mechanical device used in endoscopy in order to close two mucosal surfaces without the need for surgery and suturing. Its function is similar to a suture in gross surgical applications, as it is used to join together two disjointed surfaces, but, can be applied through the channel of an endoscope under direct visualization. Endoclips have found use in treating gastrointestinal bleeding, in preventing bleeding after therapeutic procedures such as polypectomy, and in closing gastrointestinal perforations. Many forms of endoclips exist of different shapes and sizes, including two and three prong devices, which can be administered using single use and reloadable systems, and may or may not open and close to facilitate placement.

A colorectal polyp is a polyp occurring on the lining of the colon or rectum. Untreated colorectal polyps can develop into colorectal cancer.
Therapeutic endoscopy is the medical term for an endoscopic procedure during which treatment is carried out via the endoscope. This contrasts with diagnostic endoscopy, where the aim of the procedure is purely to visualize a part of the gastrointestinal, respiratory or urinary tract in order to aid diagnosis. In practice, a procedure which starts as a diagnostic endoscopy may become a therapeutic endoscopy depending on the findings, such as in cases of upper gastrointestinal bleeding, or the finding of polyps during colonoscopy.
The non-lifting sign is a finding on endoscopic examination that provides information on the suitability of large flat or sessile colorectal polyps for polypectomy by endoscopic mucosal resection (EMR). When fluid is injected under a polyp in preparation for endoscopic mucosal resection, some polyps do not "lift", indicating that the polyp is not separating from the submucosa. This makes polypectomy more technically difficult, and increases the risk of intestinal perforation if polypectomy is then attempted. It is also thought to be indicative of an early colorectal cancer that has invaded the submucosa significantly, which would make surgical removal of the tumour preferable to allow complete removal of the cancer. Consequently, the non-lifting sign is generally considered to be a contraindication to performing endoscopic mucosal resection.

Intraductal papillary mucinous neoplasm (IPMN) is a type of tumor that can occur within the cells of the pancreatic duct. IPMN tumors produce mucus, and this mucus can form pancreatic cysts. Although intraductal papillary mucinous neoplasms are benign tumors, they can progress to pancreatic cancer. As such IPMN is viewed as a precancerous condition. Once an intraductal papillary mucinous neoplasm has been found, the management options include close monitoring and pre-emptive surgery.

An inflammatory fibroid polyp(IFP) is an uncommon digestive system tumor. J. Vanek initially identified it as a separate pathological entity in 1949 when he reported six case reports of eosinophilic infiltration in gastric submucosal granulomas. It is a single, non-encapsulated polypoid lesion that is typically submucosal. It is characterized by a large number of small blood vessels, oedematous connective tissue, and an inflammatory eosinophilic infiltrate.
Endoscopic mucosal resection is a technique used to remove cancerous or other abnormal lesions found in the digestive tract. It is one method of performing a mucosectomy.
Endoscopic endonasal surgery is a minimally invasive technique used mainly in neurosurgery and otolaryngology. A neurosurgeon or an otolaryngologist, using an endoscope that is entered through the nose, fixes or removes brain defects or tumors in the anterior skull base. Normally an otolaryngologist performs the initial stage of surgery through the nasal cavity and sphenoid bone; a neurosurgeon performs the rest of the surgery involving drilling into any cavities containing a neural organ such as the pituitary gland. The use of endoscope was first introduced in Transsphenoidal Pituitary Surgery by R Jankowsky, J Auque, C Simon et al. in 1992 G.
The per-oral endoscopic myotomy, or POEM, is a minimally invasive surgical procedure for the treatment of achalasia wherein the inner circular muscle layer of the lower esophageal sphincter is divided through a submucosal tunnel. This enables food and liquids to pass into the stomach, a process that is impaired in achalasia. The tunnel is created, and the myotomy performed, using a flexible endoscope, meaning the entire procedure can be done without external incisions.
Pancreatic mucinous cystic neoplasm (MCN) is a type of cystic lesion that occurs in the pancreas. Amongst individuals undergoing surgical resection of a pancreatic cyst, about 23 percent were mucinous cystic neoplasms. These lesions are benign, though there is a high rate of progression to cancer. As such, surgery should be pursued when feasible. The rate of malignancy present in MCN is about 10 percent. If resection is performed before invasive malignancy develops, prognosis is excellent. The extent of invasion is the single most important prognostic factor in predicting survival.

Haruhiro Inoue is a Japanese thoracic surgeon and endoscopist best known for the development of the cap endoscopic mucosal resection technique, and the first per-oral endoscopic myotomy performed in humans. He is a professor at Showa University and Director of the Digestive Disease Centre at Showa University Koto-Toyosu Hospital in Tokyo. He is known for his work in endoscopy and his contribution to the development of endoscopic technologies and procedures.