| Esophageal dilatation | |
|---|---|
 Oesophagal Bougie Dilator | |
| Specialty | gastroenterologist |
Esophageal dilatation is a therapeutic endoscopic procedure that enlarges the lumen of the esophagus. [1]
| Esophageal dilatation | |
|---|---|
 Oesophagal Bougie Dilator | |
| Specialty | gastroenterologist |
Esophageal dilatation is a therapeutic endoscopic procedure that enlarges the lumen of the esophagus. [1]
It can be used to treat a number of medical conditions that result in narrowing of the esophageal lumen, or decrease motility in the distal esophagus. These include the following:
There are three major classes of dilators:[ citation needed ]
Complications of esophageal dilatation include the following:[ citation needed ]

The esophagus or oesophagus, colloquially known also as the food pipe, food tube, or gullet, is an organ in vertebrates through which food passes, aided by peristaltic contractions, from the pharynx to the stomach. The esophagus is a fibromuscular tube, about 25 cm (10 in) long in adults, that travels behind the trachea and heart, passes through the diaphragm, and empties into the uppermost region of the stomach. During swallowing, the epiglottis tilts backwards to prevent food from going down the larynx and lungs. The word oesophagus is from Ancient Greek οἰσοφάγος (oisophágos), from οἴσω (oísō), future form of φέρω + ἔφαγον.

Esophageal achalasia, often referred to simply as achalasia, is a failure of smooth muscle fibers to relax, which can cause the lower esophageal sphincter to remain closed. Without a modifier, "achalasia" usually refers to achalasia of the esophagus. Achalasia can happen at various points along the gastrointestinal tract; achalasia of the rectum, for instance, may occur in Hirschsprung's disease. The lower esophageal sphincter is a muscle between the esophagus and stomach that opens when food comes in. It closes to avoid stomach acids from coming back up. A fully understood cause to the disease is unknown, as are factors that increase the risk of its appearance. Suggestions of a genetically transmittable form of achalasia exist, but this is neither fully understood, nor agreed upon.

Esophagitis, also spelled oesophagitis, is a disease characterized by inflammation of the esophagus. The esophagus is a tube composed of a mucosal lining, and longitudinal and circular smooth muscle fibers. It connects the pharynx to the stomach; swallowed food and liquids normally pass through it.

In medicine, a stent is a tube usually constructed of a metallic alloy or a polymer. It is inserted into the lumen of an anatomic vessel or duct to keep the passageway open. Stenting refers to the placement of a stent. The word "stent" is also used as a verb to describe the placement of such a device, particularly when a disease such as atherosclerosis has pathologically narrowed a structure such as an artery.

Endoscopic retrograde cholangiopancreatography (ERCP) is a technique that combines the use of endoscopy and fluoroscopy to diagnose and treat certain problems of the biliary or pancreatic ductal systems. It is primarily performed by highly skilled and specialty trained gastroenterologists. Through the endoscope, the physician can see the inside of the stomach and duodenum, and inject a contrast medium into the ducts in the biliary tree and pancreas so they can be seen on radiographs.

Eosinophilic esophagitis (EoE) is an allergic inflammatory condition of the esophagus that involves eosinophils, a type of white blood cell. In healthy individuals, the esophagus is typically devoid of eosinophils. In EoE, eosinophils migrate to the esophagus in large numbers. When a trigger food is eaten, the eosinophils contribute to tissue damage and inflammation. Symptoms include swallowing difficulty, food impaction, vomiting, and heartburn.
Esophageal dysphagia is a form of dysphagia where the underlying cause arises from the body of the esophagus, lower esophageal sphincter, or cardia of the stomach, usually due to mechanical causes or motility problems.

A Schatzki ring or Schatzki–Gary ring is a narrowing of the lower esophagus that can cause difficulty swallowing (dysphagia). The narrowing is caused by a ring of mucosal tissue or muscular tissue. A Schatzki ring is a specific type of "esophageal ring", and Schatzki rings are further subdivided into those above the esophagus/stomach junction, and those found at the squamocolumnar junction in the lower esophagus.

A self-expandable metallic stent is a metallic tube, or stent that holds open a structure in the gastrointestinal tract to allow the passage of food, chyme, stool, or other secretions related to digestion. Surgeons insert SEMS by endoscopy, inserting a fibre optic camera—either through the mouth or colon—to reach an area of narrowing. As such, it is termed an endoprosthesis. SEMS can also be inserted using fluoroscopy where the surgeon uses an X-ray image to guide insertion, or as an adjunct to endoscopy.

A benign esophageal stricture, or peptic stricture, is a narrowing or tightening of the esophagus that causes swallowing difficulties.
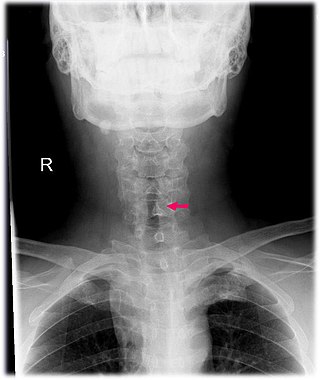
Subglottic stenosis is a congenital or acquired narrowing of the subglottic airway. It can be congenital, acquired, iatrogenic, or very rarely, idiopathic. It is defined as the narrowing of the portion of the airway that lies between the vocal cords and the lower part of the cricoid cartilage. In a normal infant, the subglottic airway is 4.5-5.5 millimeters wide, while in a premature infant, the normal width is 3.5 millimeters. Subglottic stenosis is defined as a diameter of under 4 millimeters in an infant. Acquired cases are more common than congenital cases due to prolonged intubation being introduced in the 1960s. It is most frequently caused by certain medical procedures or external trauma, although infections and systemic diseases can also cause it.

Percutaneous transhepatic cholangiography, percutaneous hepatic cholangiogram (PTHC) is a radiological technique used to visualize the anatomy of the biliary tract. A contrast medium is injected into a bile duct in the liver, after which X-rays are taken. It allows access to the biliary tree in cases where endoscopic retrograde cholangiopancreatography has been unsuccessful. Initially reported in 1937, the procedure became popular in 1952.

An esophageal food bolus obstruction is a medical emergency caused by the obstruction of the esophagus by an ingested foreign body.

An esophageal stent is a stent (tube) placed in the esophagus to keep a blocked area open so the patient can swallow soft food and liquids. They are effective in the treatment of conditions causing intrinsic esophageal obstruction or external esophageal compression. For the palliative treatment of esophageal cancer most esophageal stents are self-expandable metallic stents. For benign esophageal disease such as refractory esophageal strictures, plastic stents are available. Common complications include chest pain, overgrowth of tissue around the stent and stent migration. Esophageal stents may also be used to staunch the bleeding of esophageal varices.
Therapeutic endoscopy is the medical term for an endoscopic procedure during which treatment is carried out via the endoscope. This contrasts with diagnostic endoscopy, where the aim of the procedure is purely to visualize a part of the gastrointestinal, respiratory or urinary tract in order to aid diagnosis. In practice, a procedure which starts as a diagnostic endoscopy may become a therapeutic endoscopy depending on the findings, such as in cases of upper gastrointestinal bleeding, or the finding of polyps during colonoscopy.

Esophageal intramucosal pseudodiverticulosis (EIPD) is a rare condition wherein the wall of the esophagus develops numerous small outpouchings (pseudodiverticulae). Individuals with the condition typically develop difficulty swallowing. The outpouchings represent the ducts of submucosal glands of the esophagus. It typically affects individuals in their sixth and seventh decades of life. While it is associated with certain chronic conditions, particularly alcoholism, diabetes and gastroesophageal reflux disease, the cause of the condition is unknown. Treatment involves medications to treat concomitant conditions such as reflux and esophageal spasm, and dilation of strictures in the esophagus.

Lymphocytic esophagitis is a rare and poorly understood medical disorder involving inflammation in the esophagus. The disease is named from the primary inflammatory process, wherein lymphocytes are seen within the esophageal mucosa. Symptoms of the condition include difficulty swallowing, heartburn and food bolus obstruction. The condition was first described in 2006 by Rubio and colleagues. Initial reports questioned whether this was a true medical disorder, or whether the inflammation was secondary to another condition, such as gastroesophageal reflux disease.
Functional Lumen Imaging Probe (FLIP) is a test used to evaluate the function of the esophagus, by measuring the dimensions of the esophageal lumen using impedance planimetry. Typically performed with sedation during upper endoscopy, FLIP is used to evaluate for esophageal motility disorders, such as achalasia, diffuse esophageal spasm, etc.

Biliary endoscopic sphincterotomy is a procedure where the sphincter of Oddi and the segment of the common bile duct where it enters the duodenum are cannulated and then cut with a sphincterotome, a device that includes a wire which cuts with an electric current (electrocautery).
Esophagogastric junction outflow obstruction (EGJOO) is an esophageal motility disorder characterized by increased pressure where the esophagus connects to the stomach at the lower esophageal sphincter. EGJOO is diagnosed by esophageal manometry. However, EGJOO has a variety of etiologies; evaluating the cause of obstruction with additional testing, such as upper endoscopy, computed tomography, or endoscopic ultrasound may be necessary. When possible, treatment of EGJOO should be directed at the cause of obstruction. When no cause for obstruction is found, observation alone may be considered if symptoms are minimal. Functional EGJOO with significant or refractory symptoms may be treated with pneumatic dilation, per-oral endoscopic myotomy (POEM), or botulinum toxin injection.