| Mediastinitis | |
|---|---|
 | |
| Mediastinum | |
| Specialty | Pulmonology |
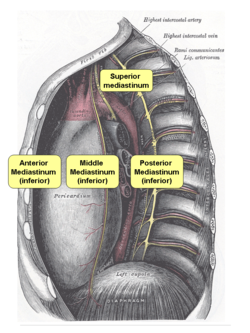
Mediastinitis is inflammation of the tissues in the mid-chest, or mediastinum. It can be either acute or chronic. It is thought to be due to four different etiologies: [1]
Contents
- Symptoms
- Acute
- Chronic
- Causes
- Acute 2
- Chronic 2
- Etiology
- Diagnosis
- Acute 3
- Chronic 3
- Treatment
- Prognosis
- References
- External links
- direct contamination
- hematogenous or lymphatic spread
- extension of infection from the neck or retroperitoneum
- extension from the lung or pleura
Acute mediastinitis is usually caused by bacteria and is most often due to perforation of the esophagus. As the infection can progress rapidly, this is considered a serious condition.
Chronic sclerosing (or fibrosing) mediastinitis, while potentially serious, is caused by a long-standing inflammation of the mediastinum, leading to growth of acellular collagen and fibrous tissue within the chest and around the central vessels and airways. It has a different cause, treatment, and prognosis than acute infectious mediastinitis.
Space infections: Pretracheal space – lies anterior to trachea. Pretracheal space infection leads to mediastinitis. Here, the fascia fuses with the pericardium and the parietal pleura, which explains the occurrence of empyema and pericardial effusion in mediastinitis. However, infectious of other spaces can also lead to mediastinitis.