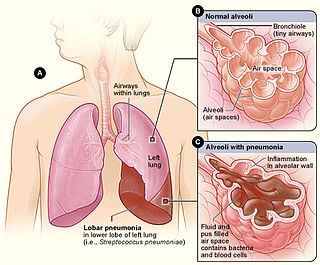
Pneumonia is an inflammatory condition of the lung primarily affecting the small air sacs known as alveoli. Symptoms typically include some combination of productive or dry cough, chest pain, fever, and difficulty breathing. The severity of the condition is variable.

Sputum is mucus that is coughed up from the lower airways. In medicine, sputum samples are usually used for a naked eye examination, microbiological investigation of respiratory infections and cytological investigations of respiratory systems. It is crucial that the specimen does not include any mucoid material from the nose or oral cavity.
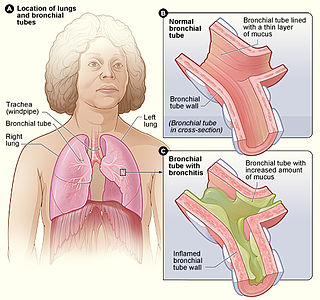
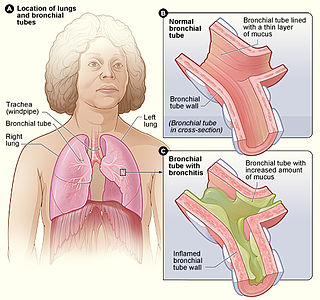
Acute bronchitis, also known as a chest cold, is short-term bronchitis – inflammation of the bronchi of the lungs. The most common symptom is a cough. Other symptoms include coughing up mucus, wheezing, shortness of breath, fever, and chest discomfort. The infection may last from a few to ten days. The cough may persist for several weeks afterward with the total duration of symptoms usually around three weeks. Some have symptoms for up to six weeks.
Atypical pneumonia, also known as walking pneumonia, is any type of pneumonia not caused by one of the pathogens most commonly associated with the disease. Its clinical presentation contrasts to that of "typical" pneumonia. A variety of microorganisms can cause it. When it develops independently from another disease, it is called primary atypical pneumonia (PAP).
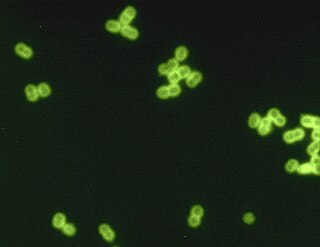
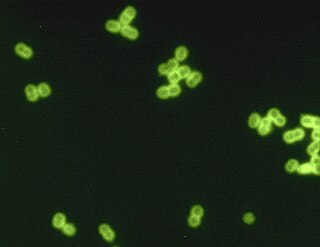
Streptococcus pneumoniae, or pneumococcus, is a Gram-positive, spherical bacteria, alpha-hemolytic member of the genus Streptococcus. S. pneumoniae cells are usually found in pairs (diplococci) and do not form spores and are non motile. As a significant human pathogenic bacterium S. pneumoniae was recognized as a major cause of pneumonia in the late 19th century, and is the subject of many humoral immunity studies.
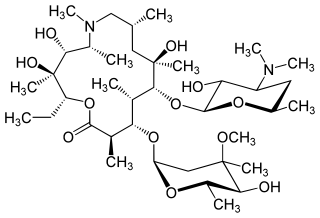
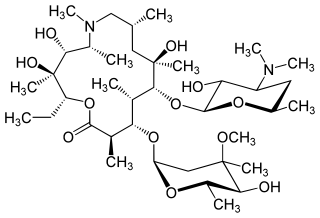
Azithromycin, sold under the brand names Zithromax and Azasite, is an antibiotic medication used for the treatment of a number of bacterial infections. This includes middle ear infections, strep throat, pneumonia, traveler's diarrhea, and certain other intestinal infections. Along with other medications, it may also be used for malaria. It is administered by mouth, into a vein, or into the eye.

Haemophilus influenzae is a Gram-negative, non-motile, coccobacillary, facultatively anaerobic, capnophilic pathogenic bacterium of the family Pasteurellaceae. The bacteria are mesophilic and grow best at temperatures between 35 and 37 °C.

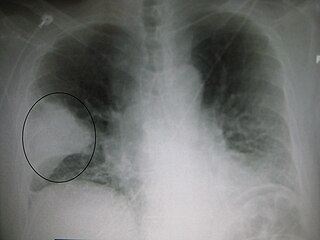
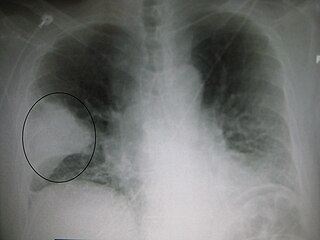
Lower respiratory tract infection (LRTI) is a term often used as a synonym for pneumonia but can also be applied to other types of infection including lung abscess and acute bronchitis. Symptoms include shortness of breath, weakness, fever, coughing and fatigue. A routine chest X-ray is not always necessary for people who have symptoms of a lower respiratory tract infection.

The bacterial capsule is a large structure common to many bacteria. It is a polysaccharide layer that lies outside the cell envelope, and is thus deemed part of the outer envelope of a bacterial cell. It is a well-organized layer, not easily washed off, and it can be the cause of various diseases.
Community-acquired pneumonia (CAP) refers to pneumonia contracted by a person outside of the healthcare system. In contrast, hospital-acquired pneumonia (HAP) is seen in patients who have recently visited a hospital or who live in long-term care facilities. CAP is common, affecting people of all ages, and its symptoms occur as a result of oxygen-absorbing areas of the lung (alveoli) filling with fluid. This inhibits lung function, causing dyspnea, fever, chest pains and cough.
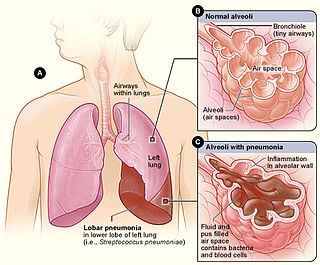
Lobar pneumonia is a form of pneumonia characterized by inflammatory exudate within the intra-alveolar space resulting in consolidation that affects a large and continuous area of the lobe of a lung.
Pneumococcal pneumonia is a type of bacterial pneumonia that is caused by Streptococcus pneumoniae (pneumococcus). It is the most common bacterial pneumonia found in adults, the most common type of community-acquired pneumonia, and one of the common types of pneumococcal infection. The estimated number of Americans with pneumococcal pneumonia is 900,000 annually, with almost 400,000 cases hospitalized and fatalities accounting for 5-7% of these cases.

Gemifloxacin mesylate, sold under the brand name Factive among others, is a broad-spectrum quinolone antibacterial agent used in the treatment of acute bacterial exacerbation of chronic bronchitis and mild-to-moderate pneumonia. It is taken by mouth. Vansen Pharma Inc. licensed the active ingredient from LG Life Sciences of Korea.

Hospital-acquired pneumonia (HAP) or nosocomial pneumonia refers to any pneumonia contracted by a patient in a hospital at least 48–72 hours after being admitted. It is thus distinguished from community-acquired pneumonia. It is usually caused by a bacterial infection, rather than a virus.

Ceftibuten is a third-generation cephalosporin antibiotic. It is an orally administered agent, with two dosage forms, capsule or oral suspension. It is marketed by Pernix Therapeutics under the trade name Cedax.
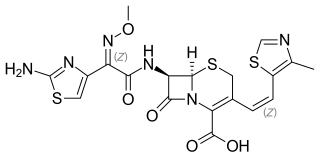
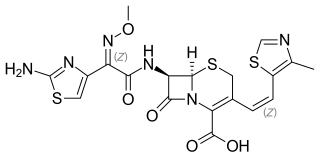
Cefditoren, also known as cefditoren pivoxil is an antibiotic used to treat infections caused by Gram-positive and Gram-negative bacteria that are resistant to other antibiotics. It is mainly used for treatment of community acquired pneumonia. It is taken by mouth and is in the cephalosporin family of antibiotics, which is part of the broader beta-lactam group of antibiotics.

Cefodizime is a 3rd generation cephalosporin antibiotic with broad spectrum activity against aerobic gram positive and gram negative bacteria. Clinically, it has been shown to be effective against upper and lower respiratory tract infections, urinary tract infections, and gonorrhea. Cefodizime is a bactericidal antibiotic that targets penicillin-binding proteins (PBPs) 1A/B, 2, and 3 resulting in the eventual death of the bacterial cell. In vivo experimental models of infection showed that bacterial clearance by this drug is at least as effective compared with other 3rd generation cephalosporins. It has similar adverse effect profile to other 3rd generation cephalosporins as well, mainly being limited to gastrointestinal or dermatological side effects.
Pneumococcal infection is an infection caused by the bacterium Streptococcus pneumoniae.

An acute exacerbation of chronic obstructive pulmonary disease, or acute exacerbations of chronic bronchitis (AECB), is a sudden worsening of chronic obstructive pulmonary disease (COPD) symptoms including shortness of breath, quantity and color of phlegm that typically lasts for several days.
Pneumonia can be classified in several ways, most commonly by where it was acquired, but may also by the area of lung affected or by the causative organism. There is also a combined clinical classification, which combines factors such as age, risk factors for certain microorganisms, the presence of underlying lung disease or systemic disease and whether the person has recently been hospitalized.